-
PDF
- Split View
-
Views
-
Cite
Cite
Fahad K Uddin, Lorenzo K Sampson, Chronic abdominal pain leads to discovery of congenital anomaly, Journal of Surgical Case Reports, Volume 2022, Issue 8, August 2022, rjac381, https://doi.org/10.1093/jscr/rjac381
Close - Share Icon Share
Abstract
A 43-year-old female with no history of a cholecystectomy presented with chronic right sided abdominal pain that became worse after fatty food intake. This led to an extensive workup for gallbladder disease for the patient’s source of her pain. She had an initial ultrasound, which showed a collapsed gallbladder around gallstones, which signified chronic cholecystitis. This was confirmed with a hepatobiliary iminodiacetic acid scan with Choletec and morphine as there was no visualization of the gallbladder. Due to the patient’s persistent abdominal pain with associated symptoms and radiographic evidence of cholecystitis, she was taken to the operating theater for a laparoscopic cholecystectomy and the absence of a gallbladder was discovered. The goal of this clinical case report is to highlight this rare anomaly and how it presents in a clinical setting.
INTRODUCTION
Gallbladder agenesis is a rare anomaly in which there is a congenital absence of a gallbladder. The gallbladder is an intraperitoneal organ that stores bile to help emulsify fat and aid in its digestion. Embryologically, this organ is derived from a small ventral outgrowth of the hepatic diverticulum, which arises from the distal end of the primitive foregut around the third week of development [1]. A failure of this developmental process may lead to its congenital absence. Most patients are asymptomatic, and this is discovered incidentally when imaging is done for other reasonings.
CASE REPORT
A 43-year-old female presents to the surgery clinic due to chronic right sided abdominal pain characterized as a cramping and fluttering like sensation. Associated symptoms include nausea, vomiting, episodes of post-prandial loose non-bloody stools and abdominal distension with a sensation of bloating. Medical history includes hyperlipidemia, and she denies any surgical procedures specifically of the abdomen. She does endorse alcohol use.
At her initial presentation in the emergency department, the patient underwent an abdominal ultrasound, which showed a collapsed gallbladder around gallstones. Due to this finding, she was referred to the surgery clinic. After further discussion with the patient at the clinic, her symptomology was more characteristic of colonic spasm for which she was prescribed hycosamine. A hepatobiliary iminodiacetic acid (HIDA) scan was ordered for further investigation, but she failed to follow up.
The patient returned to the clinic 2 years later due to continued pain, located over the epigastric, right upper and right lower aspects of her abdomen. She underwent the HIDA scan with 5-mCi Choletec, which demonstrated a non-visualized gallbladder throughout the entire study even with the administration of 3.6-mg morphine, which were consistent with chronic cholecystitis. At her subsequent clinic visit, she continued to report right upper quadrant pain, which now radiated to the right side of her back worse after fatty food intake and with associated nausea. Because of her HIDA scan finding of cholecystitis and her continued symptoms, she was scheduled for an outpatient laparoscopic cholecystectomy.
The patient was taken to the operating room and was prepped in normal sterile fashion with proper induction of anesthesia. Laparoscopic ports were placed in the supraumbilical and subxiphoid aspect of the abdomen and two were placed in the right subcostal aspect of the abdomen using 5-mm laparoscopic trocars. The patient was noted to have significant omental adhesions off the transverse colon attaching to the liver and ~25–30 min were spent lysing these adhesions. Once these were mobilized, the liver was elevated in a superior cephalad fashion, which did not show the presence of a gallbladder, signifying gallbladder

Image showing the absence of a gallbladder within the fossa of the liver.
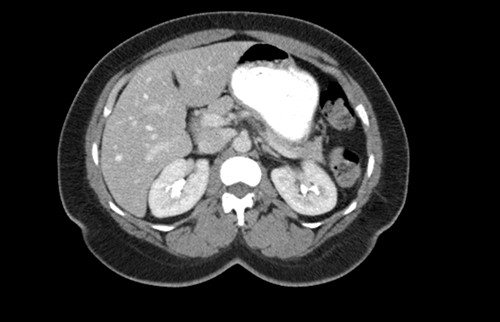
CT scan of the abdomen showing the absence of the gallbladder within the gallbladder fossa. This image also depicts the absence of malrotation of the gut or horseshoe kidney.

CT scan of the abdomen showing the absence of the gallbladder within the gallbladder fossa. This image also depicts the absence of malrotation of the gut or horseshoe kidney.
agenesis as seen in Fig. 1. The port sites were sutured closed, and no post-operative complications were noted. It was concluded that the adhesions were causing the patient’s chronic abdominal pain which resolved. A computed tomography (CT) scan of the abdomen seen in Figs 2 and 3 confirmed the absence of a gallbladder with no associated pathology depicted.
DISCUSSION
Gallbladder agenesis is a rare anomaly in which an individual is born without a gallbladder. This phenomenon affects <0.1% of the population with only 400 cases documented in medical literature to this day [2, 3]. This anomaly is discovered incidentally during workups for symptoms consisting of gallbladder pathology as seen in our patient. Initial work up for a gallbladder pathology includes a right upper quadrant ultrasound and, in this patient, it showed a collapsed gallbladder around gallstones, as seen in Fig. 4. This pointed to a diagnosis of cholecystitis. A further look with a HIDA scan confirmed this diagnosis as it showed the absence of radiotracer entering the gallbladder even after the administration of morphine, seen in Figs 5 and 6. A non-visualized gallbladder typically occurs due a gallstone obstructing the passage of the radiotracer entering the gallbladder [4]. Gallbladder agenesis could cause this radiographic finding as well, however, this anomaly was low in our differential as the initial ultrasound showed a collapsed gallbladder and the patient’s absence of other medical conditions associated with gallbladder agenesis, such as Klippel–Feil syndrome, horseshoe kidney, malrotation of the gut or aberrant left pulmonary artery, none of which were suspected in our patient seen on examination and radiographically [1]. The normal location of the gallbladder is located on the undersurface of the liver, aligning with the intrahepatic line that separates the right and left hepatic lobe. There was no sign of this organ once the liver was elevated, seen in Fig. 1. The likely cause of this patient’s chronic right sided abdominal pain were the multiple abdominal adhesions, which were lysed.
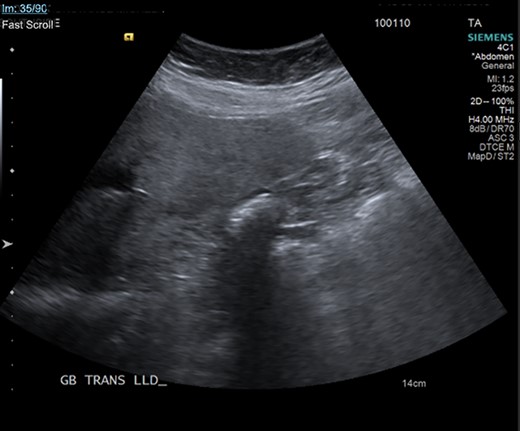
Ultrasound of the gallbladder showing echogenic shadow from the gallbladder fossa around gallstones, suggesting a collapsed gallbladder around stones.
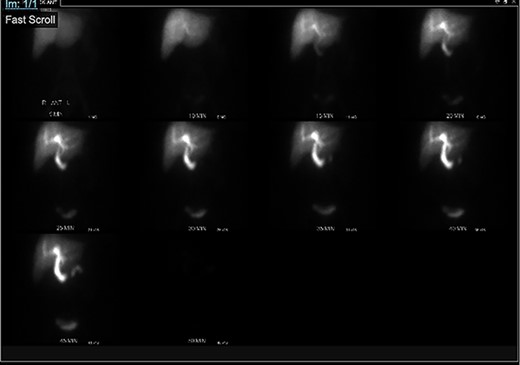
HIDA scan showing normal extraction of radiotracer into the biliary tree with non-visualization of the gallbladder, pre morphine.
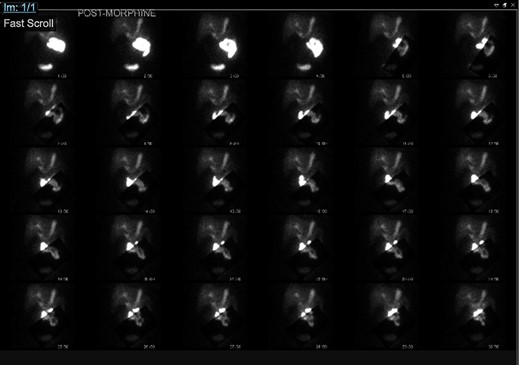
HIDA scan showing normal extraction of radiotracer into the biliary tree with non-visualization of the gallbladder, post morphine.
The focus of treatment for symptomatic gallbladder agenesis once it is confirmed is conservative management, including smooth muscle relaxants such as hycosamine, which was given to our patient early during her evaluation. Another option for refractory cases include a sphincterotomy, which is a procedure that dissects the sphincter of Oddi and intraduodenal segment of the common bile duct using endoscopic retrograde cholangiopancreatography [5]. This procedure is carried out for Sphincter of Oddi Dysfunction in which the sphincter fails to relax causing backup of bile and pancreatic juice, causing chronic abdominal pain. This diagnosis would have been sought out if our patient’s pain did not improve.
AUTHORS’ CONTRIBUTIONS
Dr. Lorenzo K. Sampson, MD was the lead surgeon on this case, provided this case to be written into a case report, and revised the intellectual information of this report; Fahad Kausar Uddin was the assistant to the surgeon during this case and contributed to the design, acquisition and analysis of case information. and was responsible for creating this case report.
ACKNOWLEDGMENTS
Special thank you to Aiken Regional Medical Centers and Dr. Lorenzo K. Sampson, MD for providing the opportunity to work on this case and create a case report on this rare pathology.
INFORMED CONSENT
Verbal and written consent was obtained from the patient by Dr. Lorenzo K. Sampson, MD.
CONFLICT OF INTEREST STATEMENT
There were no conflict of interest for this case report.
FUNDING
None declared.



