-
PDF
- Split View
-
Views
-
Cite
Cite
Hiroshi Noguchi, Masao Koda, Toru Funayama, Hiroshi Takahashi, Kousei Miura, Fumihiko Eto, Yosuke Shibao, Kosuke Sato, Tomoyuki Asada, Masashi Yamazaki, Surgical treatment for kyphotic deformity after anterior cervical fusion with a severely tortuous vertebral artery: a case report, Journal of Surgical Case Reports, Volume 2022, Issue 8, August 2022, rjac363, https://doi.org/10.1093/jscr/rjac363
Close - Share Icon Share
Abstract
We performed salvage surgery on a patient with kyphotic deformity after anterior cervical fusion with a tortuous vertebral artery (VA). A 69-year-old woman had undergone anterior cervical corpectomy and fusion 12 years ago. Her cervical alignment gradually became kyphotic because of bone graft collapse. Ten years after surgery, she experienced severe neck pain, recurrence of myelopathic symptoms and difficulty in keeping her head straight. The patient was diagnosed with rigid cervical kyphosis at C4–6 vertebral levels, with the right tortuous VA invaginating into the C4 vertebral body. We selected a three-stage, anterior–posterior–anterior approach to reduce cervical alignment. The key to a successful surgery in this case was to retract the tortuous VA within the C4 vertebral body, followed by total uncinectomy. Careful preoperative VA evaluation was a decisive factor in surgical planning.
INTRODUCTION
Cervical kyphotic deformity, caused by congenital and acquired factors, can have detrimental effects on an individual’s life and compromise forward gaze and postural retention. Additionally, myelopathy and nerve root symptoms due to compression of the cervical spinal cord are often observed.
Surgical treatment can adopt an anterior, posterior or combined approach; however, there is no established strategy. Treatment strategies are developed on a case-by-case basis, taking into consideration factors, such as the severity and rigidity of the kyphotic deformity, a coexisting facet joint fusion and patient background, including comorbidities and age.
Vertebral artery (VA) injury can occur during cervical spine surgery because it runs near the operative site, especially in cases with VA Anomalies. Though rare (incidence, 0.3–0.5%), iatrogenic VA injury may result in devastating complications, such as massive intra- or postoperative hemorrhage, cardiac arrest, neurologic sequelae or death [1–3].
Herein, we report a rare case of corrective surgery for severe kyphotic deformity with a tortuous VA within the C4 vertebral body.

History of kyphosis after ACCF (anterior cervical corpectomy and fusion), and the patient had undergone ACCF 12 years ago for cervical spondylotic myelopathy; the kyphotic changes occurred early in the postoperative period and gradually progressed. POY1, 5, 12: Postoperative year 1, 5, 12.
CASE REPORT
A 69-year-old woman had undergone anterior cervical corpectomy and fusion 12 years ago for cervical spondylotic myelopathy. Postoperatively, her right-hand numbness and weakness had improved; however, her cervical alignment gradually became kyphotic because of bone graft collapse (Fig. 1). Ten years after surgery, she experienced severe neck pain, omalgia, mild numbness and muscle weakness in both upper limbs. Her symptoms deteriorated within 1 year, and she complained of horizontal gaze disturbances.
On admission, she presented with mild gait disturbance. Cervical range of motion was 60°of forward flexion and −15°of backward flexion. The patient had no upper or lower limb weakness; however, she reported dull neck and shoulder pain, decreased hand dexterity and decreased sensation in the right upper limb. Deep tendon reflexes were increased in both upper limbs, and the patellar and Achilles tendon reflexes were not increased in both sides because of lumbar spondylolisthesis. The Japanese Orthopedic Association (JOA) score for cervical myelopathy was 13 (out of 17 points).
On clinical examination, we observed severe kyphosis (C2–7 angle: −65) with C4–6 fusion. Magnetic resonance imaging (MRI) and computed tomography (CT) myelography revealed C3/4 spinal canal stenosis with C3 anterior slip. Imaging showed two right transverse foramina at the C4 level and a tortuous right VA invaginating into the C4 vertebral body (Fig. 2).
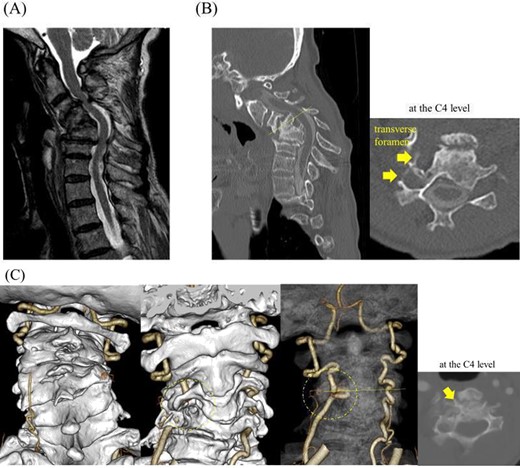
CT myelography, MRI and CT angiography on admission; (A) stenosis at the C3/4 level with C3 anterior slip was observed on magnetic resonance T2-weighted images, and (B) the C4–6 vertebrae were fused into a single mass; note local kyphosis and scoliosis due to vertebral collapse, and a transverse slice at the C4 level showed two transverse foramina on the right side, and (C) the right VA invaginating into the C4 vertebral body was shown in a transverse slice at the C4 level on CT angiography.
We planned a three-stage, anterior–posterior–anterior approach. In the first stage, we opted for a right-sided approach to reach the right VA. The VA was identified at the C3 level by resection of the C3 anterior tubercle of the transverse process. The VA was explored distally to the C4 vertebral body followed by resection of the C4 anterior wall. A piece of cotton was then inserted along the inner wall of the foramen transversum, the osteophyte was removed and the VA was separated from the vertebral body (Fig. 3). We performed subtotal corpectomy of C4–6 and total uncinectomy of C3/4 and C6/7; osteotomy proceeded without injuring the VA.
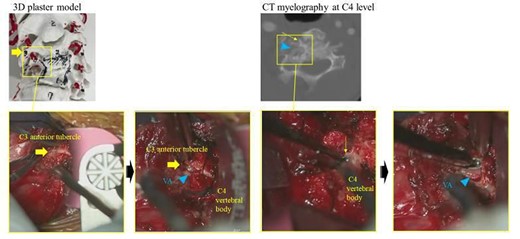
VA identification under the C3 anterior tubercle, and VA separation at the C4 vertebral body; (A) the abnormal VA in the C4 vertebra could not be directly confirmed even via the anterior cervical approach; VA was directly identified under the C3 anterior tubercle and then explored distally to secure the VA inside the C4 vertebral body; (B) after inserting a piece of cotton along the inner wall of the foramen transversum and removing the osteophyte, the VA could be separated from the C4 vertebral body.
In the second stage, bilateral resection of the fused C3/4, 4/5 and 5/6 facet joints and C3–5 laminae was performed, followed by corrective fixation of C2-T1 (C2, C7 and T1 pedicle screws and C3 and C4 lateral mass screws were placed and corrected with lordotic rod). The C2–7 angle was corrected from −65° to −6°. In the third stage, an autologous fibula was grafted into the space created after resection (Fig. 4).
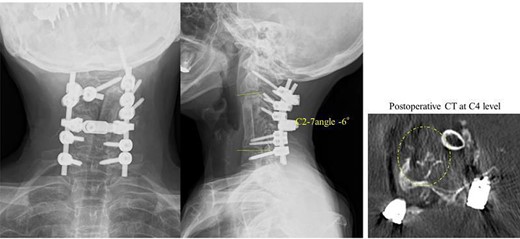
Radiography image after the three-stage combined surgery; cervical alignment was improved after this approach (the C2–7 angle was corrected from −65° to −6°).
Operation duration was 639 min, with an estimated blood loss of 620 ml. Intraoperative monitoring showed no substantial loss of motor-evoked potentials.
Postoperative complications, including pharynx swelling and wound dehiscence, were treated. After surgery, neck deformity was reduced, the patient was able to perform her daily activities and was free of neck-pain. She was discharged home 4 weeks after surgery. Her JOA score improved to 15 points (recovery rate, 50%) 1 year after surgery.
DISCUSSION
In this report, we describe a successful salvage surgery performed on a patient with rigid kyphotic deformity after anterior cervical fusion with a tortuous VA. This case was an instructive lesson on surgical strategy, preoperative evaluation and intraoperative approach of tortuous VA.
Abnormal tortuosity and migration of the VA can be rare causes of VA injury [4, 5]. In the present case, there was no abnormal VA running on the images at the time of anterior fixation. The anomalous VAs were suspected to have occurred by developing a snaking pathway and eroding the posterior lateral vertebral body in response after degenerative osteoarthritic changes. The incidence of a VA loop was reported to be 1% in 1054 subjects [6], and studies that reviewed 250 MRI scans found that 7.6% of arteries exhibit inward migration, resulting in an increased risk of injury [7, 8]. These data suggest that even if drilling is performed within safe ranges, the patient will have a risk of VA injury.
In the presence of abnormally located VA, the standard landmarks may not prevent iatrogenic injury. Thus, it is imperative that the surgical team recognizes VA anomalies preoperatively. Advanced imaging techniques, such as contrast-enhanced CT angiography (CTA), are essential for the accurate evaluation of the VA course [9]. We found 3D CTA particularly useful; this technique allowed us to generate a 3D model to better visualize the location of the abnormal VA, which is often difficult to discern with conventional CT.
Our strategy to expose the VA at the C3 transverse foramen level and retract it from the vertebral body before the C4 corpectomy was pivotal for achieving complete protection of the artery. By comparison, the C4 corpectomy without VA protection could result in accidental injury. Furthermore, in case of VA injury, our approach would facilitate treatment options, such as tamponade, repair, ligation and vascular coagulation because the VA could be approached directly [1–3].
In conclusion, correction of cervical kyphotic deformities is a complex procedure. The presence of an abnormal VA could result in complications during corpectomy. This report highlights the importance of careful preoperative evaluation of VA anatomy that would allow the surgeon to select the appropriate surgical strategy and lead to a safe outcome.
CONFLICT OF INTEREST STATEMENT
The authors declare that they have no conflicts of interest.
FUNDING
None.



