-
PDF
- Split View
-
Views
-
Cite
Cite
Emad Amirhom, Manasa Dondapati, Nisha Horton, Alison R Pescovitz, Large colonic lipoma as a lead point for intussusception in an adult, Journal of Surgical Case Reports, Volume 2022, Issue 7, July 2022, rjac327, https://doi.org/10.1093/jscr/rjac327
Close - Share Icon Share
Abstract
Intussusception is the telescoping of proximal loop of the bowel within distal loop resulting in obliteration of the lumen. Although it frequently occurs with the most common cause of intestinal obstruction in children, it is a rare phenomenon and an uncommon cause of acute intestinal obstruction in adults. Unlike pediatric intussusception, where the cause is idiopathic, adult intussusception is associated with underlying pathology as a lead point. The underlying pathology usually is malignant, but the prognosis is better when there is a benign lead point. The benign lead point intussusceptions are rare and are treated with reduction when there are no signs of ischemia. When there is ischemia or when reduction is not feasible, they are treated with surgical resection. In this report, we describe a rare case of an adult intussusception from a large colonic lipoma in a 79-year-old male, treated successfully with surgical resection.
INTRODUCTION
Intussusception is the telescoping of proximal loop of the bowel within distal loop resulting in obliteration of the lumen [1]. While it most commonly occurs in children, intussusception in adults is rare (two cases/100 000 population/year) [1]. Although most common cause of intestinal obstruction in children, it is an uncommon cause of acute intestinal obstruction in adults [2, 5]. Adult intussusceptions make up for only ~5% of all intussusceptions and 1–5% of bowel obstructions [3]. Intussusception rarely occurs in the colon and when an adult colonic intussusception occurs, it usually is from a malignant lead point [4, 5].Lipoma of large intestine is rare accounting for 5% of all gastrointestinal tumors [3] and when it is present, it can serve as a benign lead point for colonic intussusception [3, 5]. Therefore, intussusception presenting in an adult, in the colon, and from a benign lead point is very unusual and we are describing one such case in this report.
CASE REPORT
A 79-year-old male, with a medical history of hypertension, hyperlipidemia and coronary artery disease on Atorvastatin and Metoprolol, presented to the emergency department with complaints of fatigue, anorexia, nausea, vomiting, abdominal distension and obstipation for 5 days. The patient denied having any surgeries in the past, and there was no history of having colonoscopy. His family history and social history were not significant.
On presentation, the patient was afebrile with stable vital signs. Physical exam was significant for a markedly distended abdomen with generalized tenderness, worse on the left side with resonance on percussion. There were no abdominal hernias. The digital rectal examination revealed no lesions. The rectal tone was good and there was no stool in the vault. Laboratory evaluation showed hypokalemia (3 mmol/L) and mild anemia (hemoglobin 13.1 g/dl).A computed tomography (CT) scan of abdomen and pelvis was performed and showed colonic intussusception in the descending colon with a possible lipoma/ fat containing lesion associated with the wall of the distal left colon and proximal sigmoid colon measuring 4.2 cm × 4.3 cm (Figs 1–3). There was marked distended right colon and transverse colon but no sign of bowel perforation or free air seen. There is mucosal thickening of the left colon with pericolic stranding. Developing ischemia of the left colon could not be ruled out. With the findings on imaging, it was determined that the patient would undergo an exploratory laparotomy with left hemicolectomy to remove the intussuscepted bowel.
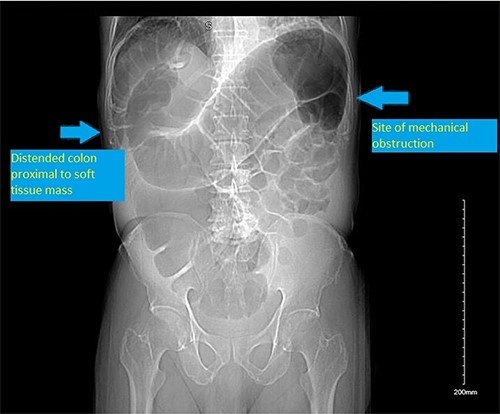
CT scan scout showing distended colon proximal to a soft tissue mass/ shadow at the splenic flexure.
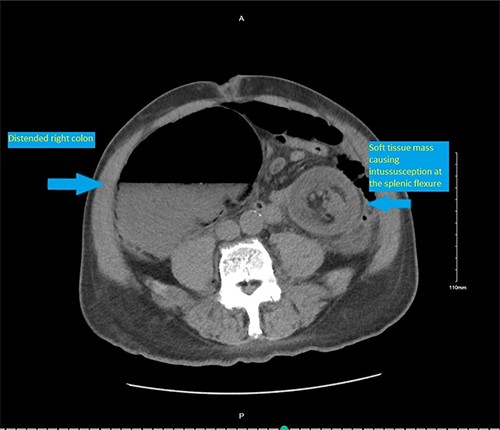
CT scan pelvis (axial cut) showing a soft tissue lesion in the left colon, with surrounding fat stranding and distended right colon.

CT scan pelvis (axial and coronal cuts) showing a soft tissue lesion in the left colon, with surrounding fat stranding and distended right and transverse colon.
The patient was taken to the operating room where he had an exploratory laparotomy. Upon entering the abdomen, clear straw-colored fluid was suctioned out and markedly dilated ascending and transverse colon was found with decompressed descending and sigmoid. The transition point was at the splenic flexure which had a soft intraluminal colonic mass, lipomatous in consistency causing the intussusception. A left hemicolectomy was performed with a side to side colo-colic anastomosis. Pathology of the specimen revealed a 4.7 cm submucosal lipoma with foci of edema of the mucosa in the wall of the left colon (Fig. 4).
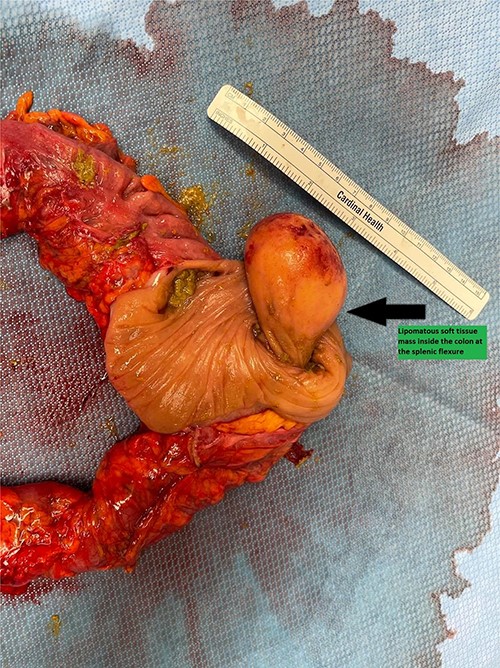
The left hemicolectomy specimen opened to show the intraluminal lipomatous lesion causing the mechanical obstruction at the splenic flexure.
DISCUSSION
Adult intussusception is rare and usually occurs in small intestine with mostly (70–75%) from benign lesions [3–5]. It is uncommon for adult intussusception to occur in colon (17%) [5] and when it does, it mostly (60–65%) is from a malignant lead point [6]. Lipomas of the gastrointestinal tract are also rare which usually present in the sixth or seventh decade, more commonly in females [3].As such, adult benign lead point colonic intussusception in a male as presented in our case is a rare occurrence. Although a rare clinical entity, adult intussusception has potential for severe complications if not promptly recognized and treated.
Adults with intussusception pose diagnostic challenges as they present with nonspecific symptoms, most commonly with abdominal pain (71–100%), followed by nausea and vomiting (40–60%), and in some cases, rectal bleeding (4–33%) [5, 7]. In contrast to pediatric intussusception, where obstruction is more common, only ~1% of adult intussusception cases have obstruction [5]. Given the rare prevalence of adult intussusception and the confusing clinical picture, diagnosis of adult intussusception requires high level of suspicion. The most useful diagnostic tool for adult intussusception is the CT scan and it has a sensitivity of 71.4–87.5% and a specificity of nearly 100% [5].The CT scan not only aids in diagnosis, but also helps in identifying underlying pathology [5, 8].
Lipoma is a benign tumor of mesenchymal origin and is the second most common benign tumor of the gastrointestinal tract, after adenomatous polyp [5, 9]. A lipoma that is >4 cm is referred to as a giant and is more likely to develop symptoms such as abdominal pain, changes in bowel habits, weight loss and, less often, intentional obstruction or a lead point of intussusception [5]. However, most of the gastrointestinal lipomas are asymptomatic [3, 5, 6 and 8]. Although lipoma is a benign lesion and rare cause of intussusception, removal of the lipoma is suggested in situations such as having a diameter of >4 cm, having a sessile appearance or limited pedicle, having an unclear preoperative diagnosis, having symptoms of intussusception, having involvement of the muscularis or serosa or having a lesion that cannot be resected completely by colonoscopy [10].
The treatment for adult intussusception is surgery. In most cases of adult colonic intussusception, especially in those who are >60 years of age as in our case, primary resection without reduction should be performed due to a higher risk of malignancy. In cases of small bowel intussusception reduction before resection should be carried out only if there is a definitive preoperative benign etiology, viable bowel or massive lengths of small bowel resection is needed with the risk of short gut syndrome [2].
Adult intussusception involving colon is very rare and it is even more unusual for it being from a large lipoma. A high index of suspicion and prompt diagnosis with the CT scan of abdomen will identify patients requiring emergency surgery and prevent serious complications such as obstruction, gangrene and perforation of the bowel.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



