-
PDF
- Split View
-
Views
-
Cite
Cite
Leen Omar Hijazi, Mohammed Asiri, Mohammed Jihad Al Mahdi, Majed Pharaon, Pyogenic granuloma of the larynx, Journal of Surgical Case Reports, Volume 2022, Issue 7, July 2022, rjac299, https://doi.org/10.1093/jscr/rjac299
Close - Share Icon Share
Abstract
Pyogenic granulomas are benign, typically painless, vascular tumors of the skin and mucosal surface. Recently the term ‘lobular capillary hemangioma’ has been introduced to describe the histological appearance more accurately. Major locations for pyogenic granuloma are in the head and neck region, but larynx localization is rare. In this case report, we present a case of a 36-year-old male with lobular capillary hemangioma of the larynx and discuss the related literature.
INTRODUCTION
Pyogenic granuloma is a benign, typically painless, vascular tumor of the skin and mucosal surfaces. It appears in all age groups with higher incidence in the second and third decades of life [1]. The term pyogenic granuloma is a misnomer; it is neither induced by bacterial infection nor does it represent a granuloma histologically. The term ‘lobular capillary hemangioma’ was introduced to describe these lesions’ characteristic appearance more accurately [2]. To date, the exact etiology of pyogenic granuloma remains unknown; however, reported triggering factors include minor repetitive trauma, infections and hormonal influences.
It is more common in adult women in childbearing age than in men, classically arising in pregnancy [3]. Pyogenic granuloma can appear intra-orally or extra-orally, where the most common intra-oral site being the gingival mucosa. Other intra-oral sites include lips, tongue, palate and buccal mucosa [4]. Although extremely rare, larynx localization has been previously reported as well [5].
In this study we report a case of laryngeal pyogenic granuloma with its clinical features, radiological appearance, histopathological diagnosis and management.
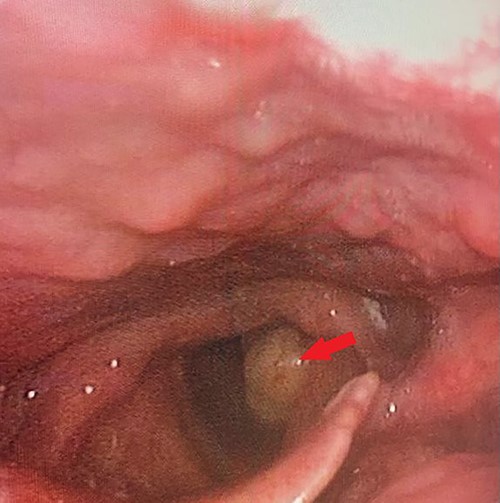
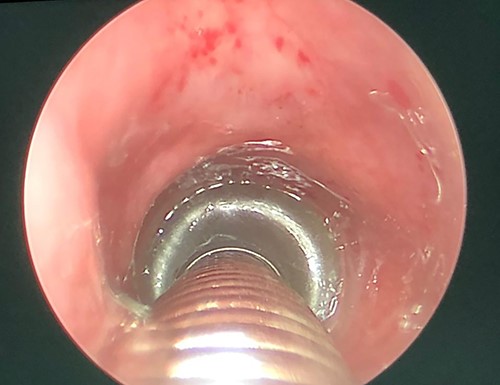
Flexible laryngoscopic examination of the larynx, showing left sided polypoidal mass.
CASE REPORT
A 36-year-old male pilot presented to the otorhinolaryngology clinic complaining of progressive hoarseness and dysphonia for 3 weeks. The patient denied dyspnea, dysphagia, shortness of breath or weight loss. He was medically and surgically free with history of smoking electronic cigarettes.
A thorough otorhinolaryngology examination was done and revealed clear oral cavity as well as normal dental health condition. On flexible laryngoscopic examination, a 2 × 1-cm yellowish polypoidal mass covering left vocal cord was found with mild signs of reflux (Fig. 1).
Computed tomography (CT) scan with contrast was ordered and showed an ill-defined heterogeneous enhancing left glottic versus supraglottic mass minimally extending to the laryngeal ventricle associated with sclerosis of the left arytenoid cartilage. It measures 2 × 0.5 × 1 cm in craniocaudal, transverse and anterior–posterior dimensions (Fig. 2). However, there was no associated invasion into the subglottic space nor paraglottic space. No pathologically enlarged cervical nor supraclavicular lymph nodes were seen.
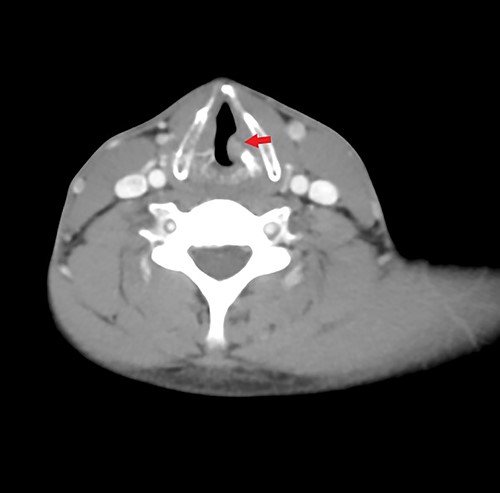
Axial contrasted CT image of larynx, showing left sided glottic versus supraglottic mass.
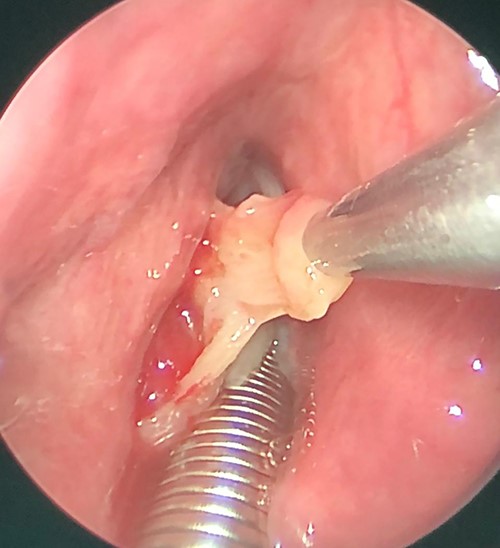
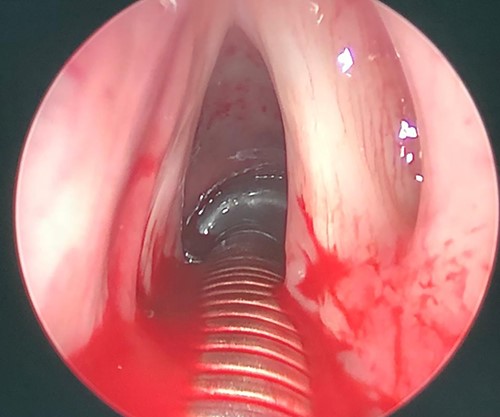
Patient was booked for direct laryngobronchoscopy with left false vocal cord mass excisional biopsy using Co2 laser. Examination under general anesthesia showed the mass extending from the left false vocal cord to the left ventricle (Figs 3 and 4). It measured 2 × 0.5 × 1 cm. The subglottic area was patent with no masses seen (Fig. 5). The mass was excised completely using Co2 laser aiding in patent airway (Fig. 6). Specimen was sent for histopathology.
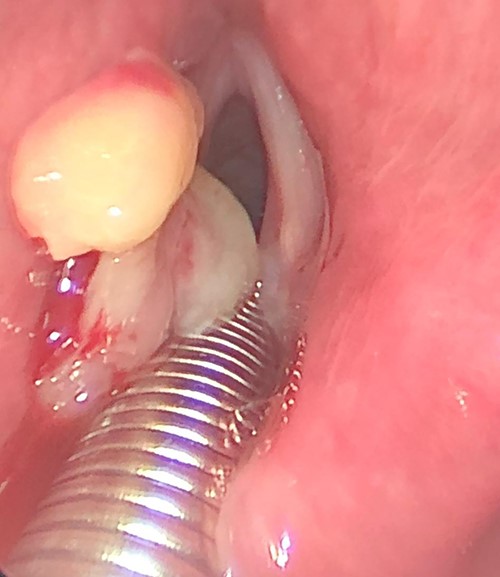
Intraoperative picture, showing left sided mass originated from left false vocal fold.
The post-operative course was uneventful, and the patient was discharged the same day with analgesics and anti-reflux medications. The patient was given appointment for follow in otolaryngology clinic one week after discharge for pathology review and reassessment. Pathology report revealed lobular capillary hemangioma with no evidence of malignancy. Histologic sections showed polypoidal squamous mucosa with associated superficial ulceration and fibrinoid necrosis (Figs 7 and 8). Submucosally, there was proliferation of small blood vessels arranged as lobules with surrounding granulation tissue and chronic inflammatory cells (Fig. 9). The endothelial cells were bland, spindled and lack dysplastic features. No atypical mitotic figures were identified. The squamous epithelium adjacent to the ulceration showed hyperplastic changes. After 2 months patient was re-evaluated again and reported improvement of his symptoms. Examination showed normal larynx with no signs of recurrence.
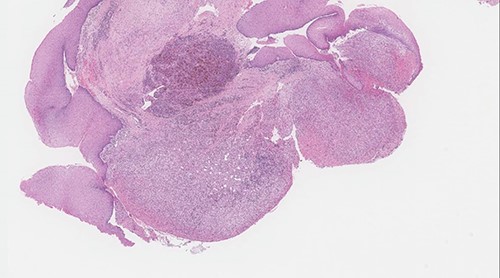
Polypoid squamous mucosa with ulceration and peripheral hyperplastic changes (original magnification: X40, H&E stain).

Surface ulceration with prominent fibrinoid necrosis (original magnification: X40, H&E stain).
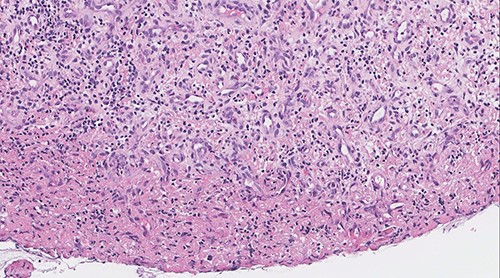
Vascular proliferation arranged as lobules with adjacent chronic inflammation (original magnification: X200, H&E stain).
DISCUSSION
Clinically, pyogenic granuloma appears as red lobulated exophytic mass on a pedunculated or sometimes sessile base, which is usually hemorrhagic [6]. In a review performed at Federal University of Rio Grande do Norte, between the years of 1970 and 2008, 9300 vascular lesions of the oral cavity were analyzed [7]. Of these, 293 cases were diagnosed as pyogenic granulomas based on biopsy findings, with the most common sites being the gingiva (83%), followed by the lip (5.3%) and tongue (5.3%), palate (4.5%) and buccal mucosa (0.8%). None of the lesions diagnosed as pyogenic granuloma were found in the larynx [7].
Although pyogenic granuloma is considered rare in the larynx, several cases have been reported in the literature. One study reported a 60-year-old male with left vocal fold pyogenic granuloma [8]. Also, another study presented an 80-year-old female with lesion on the right false vocal fold confirmed to be pyogenic granuloma on histopathology [9]. Sataloff et al. reported a case where the lesion was found to be attached to the right vocal process and posterior glottis [10]. Yakirevitch et al. reports a case of a 12-year-old female presenting with recurrent hemoptysis. Under examination, she was found to have a mass on a narrow pedicle from the right vallecula which was later confirmed to be a pyogenic granuloma [11]. Reported incidences of pyogenic granuloma occurring in the airway have been associated with antecedent traumatic injury, which includes intubation, previous surgery or laryngopharyngeal reflux [12]. In one case report, a 20-year-old woman presented to the clinic with hoarseness, shortness of breath and cough after she sustained a traumatic injury to her throat. Examination under general anesthesia showed a lesion that entirely obstructed the supraglottic area and had tethered off the superior aspect of the right arytenoid vocal process [13]. Egilmez et al., reports a case of a male patient found to have a pyogenic granuloma originating from the posterior aspect of the left vocal fold and obstructing the Rima glottis. Their patient had history of intubation prior to this diagnosis [5]. Notably, our patient did not have an antecedent intubation or trauma to the larynx.
Pyogenic granuloma is also believed to arise from hormonal changes, particularly during pregnancy. Hanick et al. reports a case of female in her third trimester presenting to the emergency department with frank hemoptysis [3]. Upon examination, she was found to have a pedunculated mass that was anchored on the medial right arytenoid mucosa by a stalk [3]. Histopathologic examination confirmed the diagnosis of pyogenic granuloma in this case [3].
In conclusion, pyogenic granuloma occurs rarely in the larynx. Symptoms include hoarseness, shortness of breath or hemoptysis. Several hypotheses have been proposed to explain the etiology of pyogenic granuloma; however, the exact cause is not yet known. Although pyogenic granuloma is a non-neoplastic growth, proper diagnosis, prevention and management of these lesions is crucial to prevent complications.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
This research did not receive any funding.



