-
PDF
- Split View
-
Views
-
Cite
Cite
Rafeh Saeed, Mekki Hassan, Fatima Tul-Zahra, Peter Neary, Ileo-ileal intussusception due to inflammatory fibroid polyp: a rare cause of small bowel obstruction in adults, Journal of Surgical Case Reports, Volume 2022, Issue 6, June 2022, rjac303, https://doi.org/10.1093/jscr/rjac303
Close - Share Icon Share
Abstract
Intussusception in adults is a relatively uncommon occurrence for a cause of bowel obstruction, which can present acutely, chronically or in an acute on chronic fashion. It is clinically concerning because of the possibility of cancer acting as a lead point. Small bowel tumours are rare, mostly detected incidentally with small bowel obstruction. Inflammatory fibroid polyp (IFP) is a rare benign tumour of the small bowel, either detected incidentally on imaging or endoscopy carried out for other reasons, or presents with acute features. We present a case of small bowel intussusception caused by IFP within the distal third of the ileum as a leading point. The patient presented acutely with small bowel obstruction, on a background of recurrent non-specific abdominal pain over the preceding month, and the computed tomography scan revealed an intussusception that was timely managed with a laparoscopy-assisted small bowel segmental resection.
INTRODUCTION
Intussusception is the invagination of a proximal portion of the intestine (intussusceptum) into an immediately distal segment (intussuscipiens) like a telescope [1]. It is usually benign, idiopathic and harmless in paediatric patients [2], but almost always pathological, with a lead point, in adults [1]. About 1% cases of adult bowel obstruction are caused by intussusception, and >90% have a distinct underlying cause related to bowel [3]. Inflammatory fibroid polyp (IFP) is a rare intraluminal benign tumour of the gastrointestinal (GI) tract that most commonly affects the stomach. Ileum is the most frequently affected site in the small bowel. Most common presentation is non-specific abdominal pain, followed by acute intestinal obstruction [4]. It is also referred to as ‘Vanek’s tumor’ because J. Vanek first described it in 1949 as a gastric granuloma with eosinophilic infiltration [5]. The cause of IFP is largely unknown, although infectious, autoimmune or allergic mechanisms have been hypothesized as probable causes [6]. Histologically IFP is characterized by submucosal spindle cell proliferation with mixed inflammatory infiltration but predominantly eosinophils [7]. We describe a case of small bowel obstruction in a 60 year-old lady caused by ileal intussusception where IFP acted as a pathological lead point.
CASE REPORT
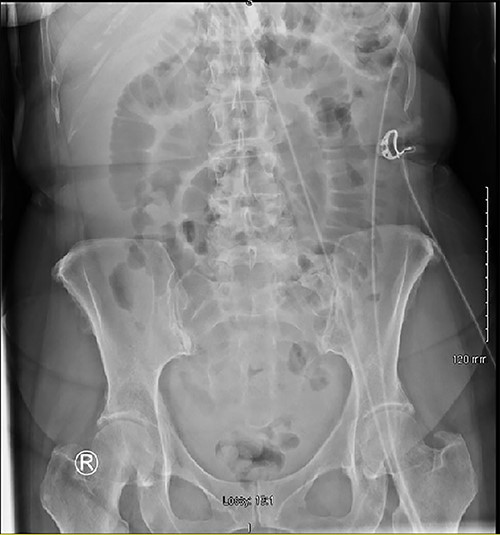
A 60 year-old female patient presented to the emergency department complaining of worsening central abdominal pain for last 4 days, associated with nausea and bilious vomiting, an episode of loose bowel motion and ‘general unwell feeling’ for last 5 weeks. She also presented 5 weeks ago with vague abdominal pain, which improved with Buscopan® and Solpadeine®; blood results were normal, so she was discharged home. She had a vague central abdominal tenderness on examination, a C-Reactive Protein (CRP) of 139, and the initial plain film abdomen showed dilated small bowel loops with paucity of air in the large bowel (Fig. 1).
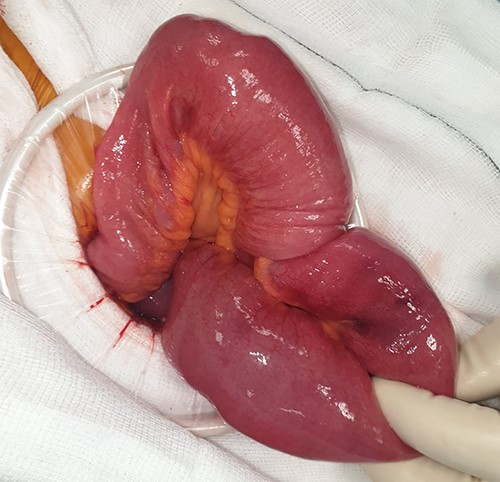
She had clinical features consistent with a sub-acute small bowel obstruction; so an urgent abdominal computed tomography (CT) scan was obtained. We inserted a wide bore nasogastric (NG) tube and commenced intravenous (IV) fluids. The CT scan reported small bowel obstruction due to ileo-ileal intussusception in its distal two-third segment (Fig. 2). After adequate resuscitation and detailed informed consent, she was brought to theatre for a laparoscopy-assisted small bowel resection. There was a 20-cm-long ileo-ileal intussusception with a lead point suggestive of a tumour-like growth (Figs 3–5). The tumour-like growth was a 30 × 25 × 20 mm polypoid mass arising from the bowel mucosa. Segmental ileal resection and stapled side to side primary anastomosis was done. She recovered well and went home 4 days later. A completion CT thorax was unremarkable. The histopathology returned as inflammatory myofibroblastic tumour (IMT) associated with intussusception of the small bowel (R0 resection). The case was discussed at our GI multidisciplinary meeting (MDM), a second histopathological opinion and surveillance CT thorax, abdomen and pelvis (TAP) in 6 months was recommended. She was followed up in clinic, developed a mild superficial surgical site infection (SSI) of the midline abdominal wound managed conservatively with regular dressings only, and later healed successfully by secondary intention. She was followed up in the clinic 6 months later, remained well and healthy to date and surveillance CT TAP did not show any metastasis or recurrence. The second pathological opinion concluded that the lesion is actually an IFP.
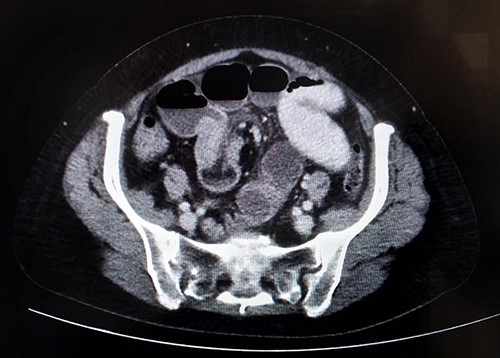
Axial section of abdominal CT scan showing bowel within bowel configuration with a layering effect indicating the site of ileal intussusception.

Ileal segment showing the site of intussusception at operation.
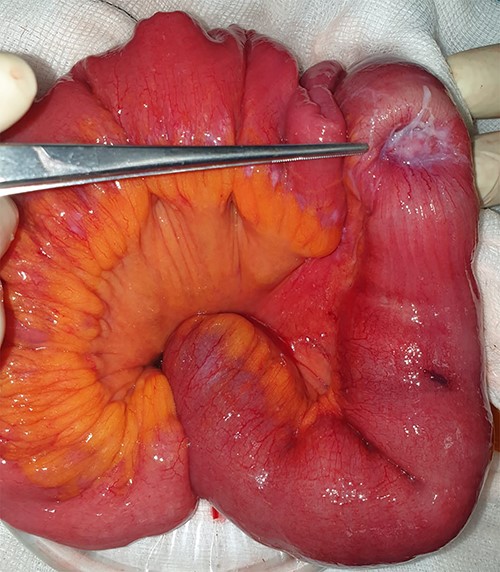
Tumour-like mass being shown at the lead point after reduction.
DISCUSSION
Intussusception is among uncommon causes of small bowel obstruction in adults accounting for only ~1% of all the cases of intestinal obstruction [3]. More than 90% cases of adult intussusception are secondary to a pathological lesion acting as a lead point. This pathological lesion can be a Meckel’s diverticulum, strictures, benign tumours or a carcinoma. There is at least 65% preoperative risk of associated malignancy in a lesion appearing to cause an adult bowel intussusception that, unlike paediatric intussusception, warrants a surgical intervention for definitive resection as the preferred treatment of choice [8]. IFP is one of the rare benign tumours affecting the small bowel, even rarer as a cause of ileal intussusception. Helwig and Ranier first coined the term IFP in 1953, before which several names like pseudo-tumour and submucosal fibroma had been used in literature [9]. PDGFRA proto-oncogene mutation has been described as possible genetic cause [10].
IFP most commonly originates in the stomach, followed by small bowel, colon and much rarely in the esophagus. Ileum is the most frequent site within the small bowel as well as the commonest site for an IFP to cause an intussusception [9]. IFP has a slight female predominance and occurs more frequently between fifth and sixth decade of life [9]. Gastric IFP more commonly presents as epigastric pain or overt GI bleeding [11]. IFP can present within a wide range of clinical spectrum, ranging from asymptomatic [12] incidental diagnosis at laparotomy or on imaging/endoscopy, non-specific chronic abdominal pain, to acute bowel obstruction due to intussusception [13].
Grossly, IFP mimics a pedunclated or sessile lesion, arising from sub-mucosa and projecting into the lumen causing ulceration of the overlying mucosa [9]. Microscopy is characterized by an onion skin appearance comprising of fibroblast-like spindle cells arranged concentrically around the vessels [12] and mixed inflammatory infiltrate mostly predominated by eosinophils [7].
CT scan is the investigation of choice, especially in a patient with obstructed small bowel. Several other diagnostic techniques like magnetic resonance-enterography, enteroclysis, endoscopic procedures (including enteroscopy [14]) or angiography are available but are more commonly used in elective settings only [9].
Although CT scan is up to 100% accurate in detecting a bowel intussusception [15], an IFP is usually not detected preoperatively probably because of the rare nature of the lesion itself, non-specific symptoms and difficult visualization within the involved bowel segment. Even if an endoluminal growth or mass is imaged preoperatively, it is commonly missed due to lack of distinctive radiological features on routine CT scans [12]. CT features of an intussusception include bull’s eye, target or sausage-shaped double-ringed lesions [15]. A bowel within bowel configuration is also suggestive of an intussusception [9]. Due to lack of a definite preoperative diagnosis, most cases are diagnosed after surgical exploration. The exact surgical treatment is controversial; however, most commonly employed treatment is segmental resection of the involved segment of bowel with sufficient margins to cater the possibility of a malignant lesion.
ACKNOWLEDGEMENTS
The authors are grateful to Ms Ann B. Prendergast, Secretary, Department of Colorectal surgery, Waterford, for her outstanding help in providing the relevant information to complete this case report.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



