-
PDF
- Split View
-
Views
-
Cite
Cite
Anestis Charalampopoulos, George Bagias, Marcos Perdicaris, Panagiotis Latsonas, Savvas Papagrigoriadis, Dimitrios Papaconstantinou, Perineal sepsis and successful surgical treatment in supralevator and ischiorectal fossa abscess: a case report, Journal of Surgical Case Reports, Volume 2022, Issue 6, June 2022, rjac287, https://doi.org/10.1093/jscr/rjac287
Close - Share Icon Share
Abstract
A male 61-year-old patient presented to the emergency department with fever, leukocytosis and perineal pain. Macroscopic examination of anogluteal region demonstrated a bulky inflamed mass in the left ischiorectal fossa with a skin defect draining large amounts of pus. The suprapubic area was observed to be erythematous, with local tenderness and a palpable inflammatory mass under the skin. Computed tomography and magnetic resonance imaging revealed an abscess of the ischiorectal fossa and concomitant supralevator abscess. Examination under anesthesia revealed an internal fistula at the posterior dentate line, with pus emanating from the orifice. A bulging mass was found, protruding in the left lateral and inferior area of the rectal ampulla, a finding compatible with the supralevator abscess identified by imaging. Drainage of the abscess into ischiorectal fossa, supralevator space and suprapubic area was successful with a prompt improvement in the clinical and laboratory profile of the patient.
INTRODUCTION
Acute inflammatory anal conditions range from simple self-limited entities to severe sepsis with high morbidity and life-threatening sequelae if they are not correctly diagnosed and treated. Imaging modalities are central in recognizing the anatomical boundaries of anal abscess–fistula; magnetic resonance imaging (MRI) is useful in more chronic conditions, whereas in acute conditions computed tomography (CT) is the most commonly employed modality used to delineate the extent of the disease [1]. The establishment of the anal abscess is based in cryptoglandular theory of infected anal glands, an old theory with new current concepts in pathogenesis under study [2]. Anal abscess and fistula may be found in several of the anatomic subspaces of the perineum, described as superficial (perianal), inter-sphincteric, ischioanal/ischiorectal and supralevator. The last one is the more rare location of anorectal abscess, accounting no more than 7% in literature [3]. The present case report describes a rare case of anal sepsis, with double location of an abscess; in supralevator space with extraperitoneal extension, fistulized in the posterior dentate line and a second extension in the ischiorectal fossa fistulized to the peri-anal skin.
CASE REPORT
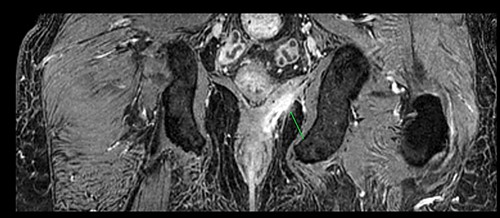
A 61-year-old diabetic patient was admitted from emergency department with septic signs; fever of 39°C, white blood cell count of 20.000/μl, C-reactive protein levels of 156 mg/l and blood glucose levels of 280 mg/dl. For the past 10 days, the patient has noted malodorous anorectal pus discharge, as well as anorectal and suprapubic pain. During macroscopic examination of the perineum, a left-sided abscess in the ischiorectal fossa was identified, with an opening lateral to the sphincteric anal system draining pus. Subsequent digital rectal examination of the anorectal canal could not be completed due to pain, but the initial effort revealed large amounts of pus discharged from anorectal canal. CT and MRI demonstrated an abscess situated in the left ischiorectal fossa and a large supralevator abscess extending cephalad in the extraperitoneal space with a long fistulous tract containing liquid (pus) and gas bubbles, up to the suprapubic area, where erythema with an undulating pus collection below the skin was noted; laterally the pus collection extended up to the left ilio-femoral vessel canal. CT (Fig. 1) and MRI (Fig. 2) were conclusive for the above entity, aptly demonstrating the presence of the two abscess cavities. Proctoscopy under general anesthesia revealed a protruding extra-rectal mass in the left lateral and inferior segment of the rectal ampulla. Finger pressure at this point was accompanied with pus exit from the posterior dentate line of the anal canal at 6 o’clock, through an opening of 1–2 mm in size. Surgery was addressed in three main locations of the pus collection with goal to drain completely the pus; the abscess of the left ischiorectal fossa was drained with enlargement of the external opening of fistula; after curettage, debridement and washing of abscess cavity, a probe was used to detect the internal opening exactly at the posterior dentate line at 6 o’clock. The fistula was characterized as full trans-sphincteric with an extra-sphincteric component in the ischiorectal fossa leading up to the skin. A non-cutting vessel loop drainage seton was then placed. The supralevator abscess was then easily drained from the opening in the posterior dentate line by finger pressure in the left rectal ampulla. A probe following the route of the internal opening upwards to supralevator space led to pus evacuation, allowing this space to be thoroughly washed with water saline solution, using a syringe with a vein catheter. Finally, the suprapubic area was drained with a small stab incision, followed by washing with normal saline. There was a prompt recovery postoperatively, tight control of blood glucose levels, whereas a CT performed 7 days postoperatively (Fig. 3), demonstrated an empty supralevator space with a fistulous tract still present, albeit with significant regression of inflammatory changes.
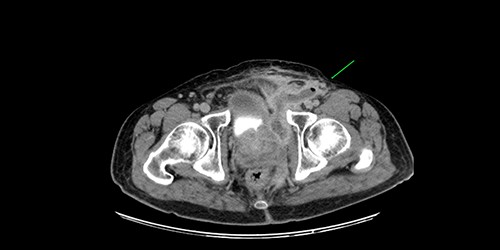
CT of the lower pelvis; supralevator abscess, with extension upward in touch with the left ilio-femoral vessels. The abscess cavity is shown approaching the skin with a long fistulous tract containing liquid (pus) and gas bubbles (green arrow).
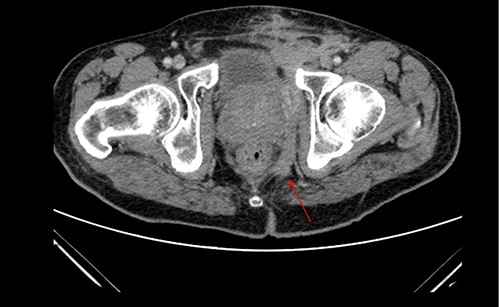
Postoperative CT of the lower pelvis, demonstrating a collapsed left supralevator space and superiorly expanding fistulous tract.
DISCUSSION
Supralevator abscesses are a rare form of anal abscess. The true incidence in a recent systematic reviews reportedly ranges from 3–7% in prospective studies and up to 27% in retrospective ones, with recurrent sepsis ranging from 0–53% in different reports [4]. The main therapy is timely and accurate surgical drain; however, debate exists about the optimal route of drainage [5]. In the present case report, CT and MRI accurately delineated the anatomic intricacies of the supralevator abscess and its extensions. The key point for the surgical drainage was the examination of anorectal canal under anesthesia; a low left lateral extra-rectal mass was easily drained through the anal canal. In higher locations of supralevator abscess a transrectal drain or drain under radiologic guidance may prove more advantageous. In our case, we refrained from draining the supralevator abscess through the left ischiorectal fossa to avoid the formation of a secondary fistulous tract in the extra-sphincteric space, which would lead to a type 3 fistula as classified by the modified Parks classification system for anal fistulas [6]. The presence of this type of fistula was ruled out during surgery, as washings of the supralevator space didn’t show any communication with the left ischiorectal fossa.
Antibiotic use was empiric using a single broad-spectrum agent (piperacillin–tazobactam). The second pus collection in the left ischiorectal fossa and the correspondent full thickness trans-sphincteric fistula was treated by curettage, washings and placement of a non-cutting drainage seton until healing and regression of the sepsis as per convention. Adequate pharmaceutical management of underlying diabetes is of extreme importance in promoting healing in the anorectal region [7].
In conclusion, supralevator abscesses are rare. Imaging data from CT and MRI are important to estimate the exact position of the abscess and help delineate the optimal drainage route. Recurrence rates are high, despite treatment, and a clinical and MRI follow-up is recommended.
AUTHORS’ CONTRIBUTIONS
All authors fulfill the four criteria of authorship according to the ICMJE recommendations and they approved the final submission.
FUNDING
None.
CONFLICT OF INTEREST STATEMENT
None declared.
CONSENT
Informed consent was obtained from the patient for publication of this work.



