-
PDF
- Split View
-
Views
-
Cite
Cite
Martina Spazzapan, Momen Sid Ahmed, Ali Tasleem, Nkwam Nkwam, Prostate cancer metastasis mimicking a primary urothelial carcinoma of the bladder, Journal of Surgical Case Reports, Volume 2022, Issue 6, June 2022, rjac275, https://doi.org/10.1093/jscr/rjac275
Close - Share Icon Share
Abstract
We report on a 79-year-old male patient who presented with asymptomatic elevation of prostate-specific antigen and a concurrent papillary lesion, which raised the suspicion of synchronous bladder and prostatic malignancies. He underwent a trans-perineal prostate biopsy as well as transurethral resection of bladder tumour, which revealed a Gleason 9 adenocarcinoma of prostatic origin. While synchronous bladder and prostate cancer is a possibility, differential diagnosis in a patient presenting with lesions of the bladder neck should include advanced prostate cancer.
INTRODUCTION
Although rare, patients affected by prostate cancer can be found to have a simultaneous bladder malignancy. Patients may present with symptoms of one cancer and found to have the other during their oncological work-up [1–3]. A different, even rarer scenario is that of advanced prostate cancer spreading to the bladder, forming lesions detectable on cystoscopy—estimated at less than 0.01% of malignant bladder tumours [4].
Given the possibility of different presentations, the diagnosis of bladder lesions in patients affected by prostate cancer can be a challenge, and misdiagnosis is a possibility. We report the case of a patient presenting with an elevated prostate-specific antigen (PSA) and a papillary lesion in his bladder, which on histology was found to be a prostatic adenocarcinoma.
CASE REPORT
A 79-year-old gentleman with no prior medical history and a ECOG Performance Status of 0 was referred to the urology 2-week-wait prostate cancer clinic due to a raised PSA of 29.9 ng/mL. He had undergone asymptomatic testing as he had a family history of prostate and breast cancer—both risk factors for prostate cancer [5, 6]. During clinic review, he reported some storage lower urinary tract symptoms but denied any visible haematuria or other red flag symptoms. Digital rectal examination revealed a firm irregularity in the left prostatic lobe.
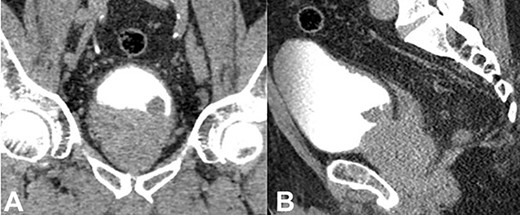
He underwent a bone single-photon emission computed tomography (SPECT) scan, which showed a focus of uptake suspicious for a left pubic tubercle metastasis, as well an area of focus in the left posterolateral side of the bladder. He later underwent a complete staging Computed tomography (CT) scan of the chest, abdomen and pelvis (Fig. 1A, B), which demonstrated prostatic enlargement, a mixed sclerotic lesion on the left pubis in keeping with metastatic disease, a polypoid mass on the left side of the bladder, highly suspicious for a primary bladder tumour, and left external iliac lymph nodes, the largest measuring 16 mm. Based on the above findings, the patient had a flexible cystoscopy that revealed an enlarged occlusive prostate, and a calcified lesion at the bladder neck of possible prostatic or bladder origin. Urine cytology was not sent at the time.
As bladder malignancy could not be ruled out, the patient was booked for simultaneous transurethral resection of bladder tumour (TURBT) + trans-perineal biopsy. Intraoperatively, digital rectal examination of the prostate revealed a firm left lobe. A 2–3 cm calcified mixed solid-papillary growth sitting in front but not involving the left ureteric orifice was seen and completely resected (Fig. 2A, B)—this was thought to be a bladder malignancy. Importantly, it was not in direct continuity with the prostate lobes so was in fact a distinct entity in itself. The bladder neck was very high with a prominent median lobe, so a limited TURP was performed to resect the base of the growth. Another nodule was seen and resected on the left inter-ureteric bar. The left ureteric orifice was preserved but, given it was very close to the resection site, a ureteric stent was inserted (Fig. 2C). Trans-perineal biopsies were obtained in the same sitting.
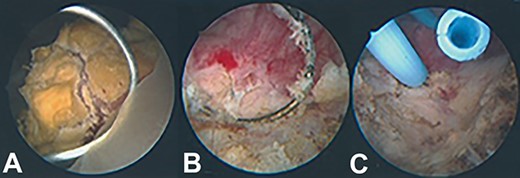
Intraoperative appearance of bladder lesion. (A) Prior to resection; (B) following resection; (C) following ureteric stent insertion.
Histological analysis revealed that all samples taken from both the bladder and the prostate were compatible with advanced prostate cancer, specifically ductal and acinar adenocarcinoma. Immunohistochemistry showed strong positive staining with PSAP, focal patchy staining with PSA and negative GATA3 staining. There was some perineural invasion, as well as invasion of the detrusor and bladder stroma.
He was discussed in our Uro-oncology MDT where his histology and diagnosis of metastatic prostate cancer was confirmed, with final pre-treatment staging of Gleason 4 + 5 = 9, T4N1M1b. He was immediately commenced on androgen deprivation therapy (ADT) and referred to the Medical Oncology team. There he was started on Enzalutamide hormonal therapy with the options of offering Docetaxel chemotherapy should his disease progress. His ureteric stent was removed 7 weeks after the operation.
DISCUSSION
Challenges in differentiating between prostate and bladder cancer have been documented. A case series from China looked at patients diagnosed with prostate malignancy [7]. The authors report that up to 3% were initially misdiagnosed as bladder malignancy due to their cancers originating from the prostate base and intruding into the bladder. Okubo et al, instead, report of a patient who had previously undergone androgen deprivation therapy for prostate cancer and represented with visible haematuria [8]. A lesion mimicking bladder malignancy was identified on cystoscopy, which on biopsy was found to be a recurrence of prostate cancer.
At histological level too, there may be challenges in distinguishing between the two malignancies [9–11]. In tissues that have previously undergone radiation therapy, biopsies may show poorly differentiated carcinomas that are difficult to characterize. The location of the mass may not correlate with the tissue of origin, increasing the risk of misdiagnosis. It is therefore important that immunohistochemistry staining of such samples includes both prostatic and urothelial markers if the history or any intraoperative findings are equivocal.
Our case report highlights the need to consider basal prostate cancer as a differential diagnosis in patients presenting with lesions of the neck or base of bladder. Considering that treatment algorithms for bladder and prostate malignancy are very different, it is crucial to be aware of and minimize the risk of misdiagnosis. Synchronous urothelial malignancy and advanced prostate cancer should both be kept as differential diagnoses and formally investigated.
We recommend that in such patients a PSA and rectal examination are always performed. Clear details of the macroscopic features and location of the lesions should be provided by surgeons to the histopathologists analyzing the biopsies, so that they can select appropriate markers for analysis. In conclusion, we report the rare case of a patient with prostate cancer metastasis masquerading as a primary urothelial carcinoma of the bladder.
CONFLICT OF INTEREST STATEMENT
No conflicts of interest to declare.
FUNDING STATEMENT
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.



