-
PDF
- Split View
-
Views
-
Cite
Cite
Daniele Macchini, Vittoria Perano, Valentina Celoria, Emilio Bombardieri, Orlando Goletti, Robotic-assisted resection of pelvic mesorectum lipoma during the COVID-19 pandemic: a case report, Journal of Surgical Case Reports, Volume 2022, Issue 6, June 2022, rjac113, https://doi.org/10.1093/jscr/rjac113
Close - Share Icon Share
Abstract
Mesorectal lipoma is a rare, usually asymptomatic tumor. The best treatment is R0 resection but the previous literature reports different approaches. Robotic surgery allows for an accurate intervention, with a faster postoperative course, less risk of infection and need for transfusions, a faster return to normal daily activities and the best esthetic result. We describe a case of a 43-year-old female with a large lipoma with dislocation of the vagina, rectum and distal sigmoid colon, potentially malignant, successfully treated by robotic excision, which was safe, effective and well tolerated by the patient.
INTRODUCTION
Mesorectal lipoma is a rare tumor, with <10 cases reported in the literature. The real incidence is unknown and maybe higher than reported due to the absence of symptoms.
Lipomas are benign tumors of mesenchymal origin composed of dedifferentiated adipocytes, while liposarcomas are the most common malignant soft tissue neoplasm in adults, accounting for 16–18% of all soft tissue tumors [1]. Currently, the classification of liposarcoma includes five subtypes: myxoid, pleomorphic, dedifferentiated, round cell and well-differentiated liposarcoma.
Surgical treatment is recommended when liposarcoma is suspected and/or symptoms occur. Giant pelvic lipomas are treated differently: open surgery, transgluteal and para-sacral approaches, and a laparoscopic approach [2–5]. We describe successful robotic resection of a large mesorectal lipoma suspected for malignancy during the coronavirus disease 2019 (COVID-19) pandemic.
CASE REPORT
A 43-year-old female came to our attention at the department of general surgery of the private hospital due to constipation, sense of pelvic bulk, recurrent low back pain, stress incontinence, urinary retention and nocturia. Physical examination showed distension of the abdominal wall. Rectal exploration revealed an extraparietal soft and elastic mass covered by normal mucosa.
The patient has no history of previous surgery or comorbidities. Family history was negative for neoplasia.
Ultrasonography detected a large pelvic mass which was confirmed by computed tomography (CT) and magnetic resonance imaging (MRI) (Fig. 1), and identified as an 8 × 5.5 cm lipoma with dislocation of the vagina, rectum and distal sigmoid colon.
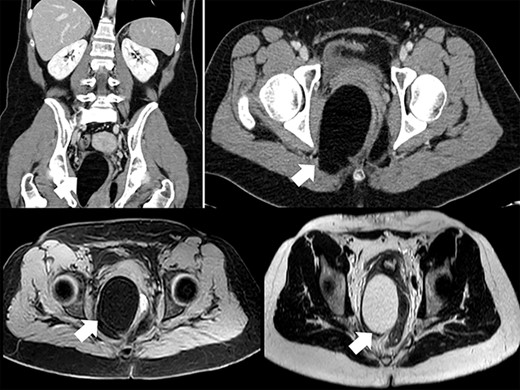
MRI and CT showed no evidence of pathological nodes and the mesorectal mass was described as an asymmetrical representation of adipose tissue of the ischiorectal fossas, prevalent on the right, with dislocation to the left of the vagina, rectum and distal sigma and scarce free fluid in the pouch of Douglas. No evidence of ureteral dilation was reported at the CT-scan and renal function was not impaired (serum creatinine was 0.71 mg/dl and estimated glomerular filtration rate was 119 ml/min).
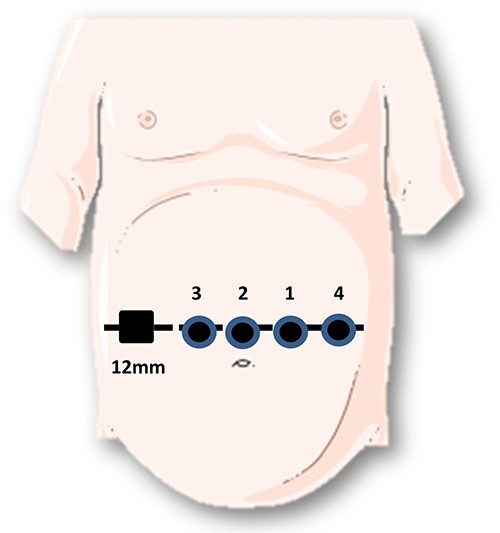
Considering the potential malignancy of the mass, the patient was addressed to robotic surgery. She underwent all current tests to exclude COVID-19 infection and positivity was excluded. She was positioned in a 15° Trendelenburg supine position. We performed a supra-umbilical open laparoscopy with introduction of 8 mm robotic trocar. Further three 8-mm-trocars and an additional 12-mm-trocar at the right flank were placed, as shown in Fig. 2. Finally, the Da-Vinci Xi system was docked while Cadiere forceps, bipolar forceps and monopolar scissors were inserted into trocar 4, 1 and 3, respectively.
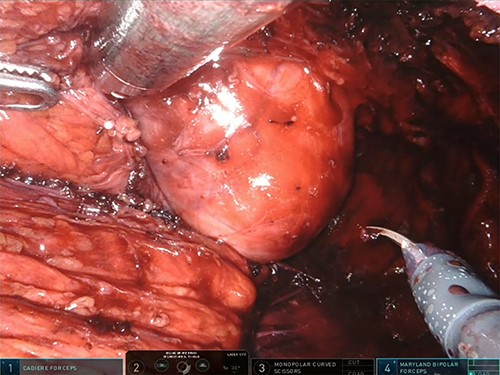
After uterus suspension and opening the presacral plane, a large mesorectal lipoma arising into the right posterolateral rectal wall was visualized (Fig. 3). Modest citrine free fluid in the Douglas pouch was collected and addressed to cytology, which was negative for malignant tumor cells. The muscolaris propria and mucosa were not involved by the lesion. The high precision of robotic surgery allows to move nimbly in the pelvis and avoid rupture of the lipoma capsule. Specimen extraction by an endoscopic bag from a Pfannenstiel scar was performed and the reported weight of the tumor was 600 g.
Rectal integrity was demonstrated by a hydro-pneumatic test, which did not show any leak.
Total console time was 2 h and 16 min and the principal operator was a general surgeon with high experience of laparoscopic and robotic surgery, particularly regarding colonic and rectal resection. The postoperative course was regular and the patient was discharged after 6 days. Histological examination confirmed the lipomatous nature of the tumor and demonstrated the absence of malignancy. MDM2 and CDK4 FISH amplification were negative.
DISCUSSION
Retroperitoneal lipomas usually affect 40-to-60-year-old patients and occur twice as often in women than in men [6]. Obesity, diabetes mellitus, hypercholesterolemia, history of traumatic injury and familial tendency are the most common risk factors [7]. Well-differentiated liposarcomas contain high-level amplification of 12q14-15 sequences, including the MDM2 and CDK4 genes, while lipomas are characterized by simple structural chromosome aberrations often involving HMGA2 at 12q15 [8].
The mechanisms of malignant transformation of a benign lipoma are still unknown [9].
By definition, giant lipomas are at least 10 cm in diameter, or weigh a minimum of 1000 g [10].
The 5-year overall survival of patients radically resected for lipomas is 100%, but recurrence occurs in 2–5% if resection is not radical [2]. Liposarcoma local recurrence after surgery is 40%; metastases are described in 17% of cases and 28% of patients will not survive the tumor [11].
The symptoms of mesorectal lipomas depend on their location and size [12]. Symptoms such as sciatica, tenesmus, diarrhea, thrombophlebitis, lower limb edema, suprapubic and perineal pain, dysuria, polyuria and hematuria, nocturia, urgency, urinary retention and incontinence may often be present [2]. On physical examination, abdominal tenderness or palpable mass, arterial hypertension and edema of lower extremities can be observed [2].
No management guidelines are currently available. CT and MRI are the gold standard for diagnosis. CT can show a homogeneously iso-intense mass with fat and no enhancement after intravenous contrast administration. MRI also enables precise diagnosis of the tumor and visualization of adjacent anatomic structures. Fat tissue demonstrates a short T1 and a relatively long T2 relaxation appearing hyperintense on T1-weighted images. Differential diagnosis between a benign and malignant lesion is not always possible without histological examination, but preoperative eco-guided biopsy has the risk of seeding the tumor. The more centrally and deeper a fatty mass is located, the more it is likely to be malignant [2]. The most indicative CT findings for malignancy are thick intralesional septa (>2 mm), rapid growth and solid components [13, 14]. Positron emission tomography has been proposed to differentiate liposarcoma, although it seems to be inadequate for differential diagnosis [2].
Scarce previous literature says that the treatment of choice is R0 surgical resection, which may be technically demanding [2]. Conservative approaches such as corticosteroids, nephrostomy, ureterostomy and even radiotherapy have not been shown to be efficacious. Intact excision of the mass through a wound protector is recommended, as well as avoiding any rupture of the capsule in order to minimize the risk of recurrence. Different treatment approaches are reported in the literature: a lesion cranially located to S3 can be managed with anterior, laparoscopic or combined en-bloc resection, while a caudal lesion to S3 can be managed with a transperineal approach [15].
We chose robotic surgery due to optimal visualization and easier debulking of the mass despite its anatomical location and proximity to vital structures [3]. Moreover, the robotic approach allowed shortening the duration of hospitalization and faster discharge of the patient, which is relevant during a period when surgical departments had to face many organizational limitations due to the COVID-19 pandemic.
The literature reports only one case of giant mesorectum lipoma resected by a robotic approach [15]. Our experience confirms that this technique may offer short hospital stay, and reduced postoperative pain, risk of infection and bleeding with a good esthetic result, while maintaining an R0 resection. In conclusion, large mesorectal lipoma can be successfully resected through a robotic approach, which in our hands was safe, effective and well-tolerated.
ACKNOWLEDGMENTS
This paper has been partially supported by the Fondazione Humanitas per la Ricerca and by a private donation from Antonella Manera in memory of her parents Mariuccia and Giovanni.
CONFLICT OF INTEREST STATEMENT
None declared.



