-
PDF
- Split View
-
Views
-
Cite
Cite
Muntashir Mahboob, Ansh Garg, Jesus De La Vi Na, Antonio Martin-Ucar, Seldinger chest drain guidewire retained in the pleural cavity—a never event complication, Journal of Surgical Case Reports, Volume 2022, Issue 5, May 2022, rjac250, https://doi.org/10.1093/jscr/rjac250
Close - Share Icon Share
Abstract
Intrapleural foreign body is an unusual complication. It most commonly occurs after the trauma but has been rarely seen after diagnostic or therapeutic procedures. We hereby, present an unusual occurrence of a retained guidewire after a chest drain insertion using a Seldinger technique in a patient with coronavirus disease of 2019 pneumonitis. Surgical removal of the guidewire has prevented this foreign body to cause further harm. We further discuss how to identify and prevent such a complication.
INTRODUCTION
Coronary virus (COVID-19) symptoms induced complications are pneumonia, acute respiratory distress syndrome, multi-organ failure, septic shock and death. COVID pneumonia can further complicate pleural effusion for which chest drains insertions are necessary to ease respiratory difficulties. Usually, ultrasound/computed tomography (CT) scan guided pigtail catheter, Seldinger drain and Routine chest tubes are inserted to drain out pleural effusions. Common chest drains complications involve chest tube clogging, hemorrhage, infections, pulmonary edema and injury to underlying organs. However, guidewire retained into the pleural cavity is always a never event complication and a serious incident that is entirely preventable.
CASE REPORT
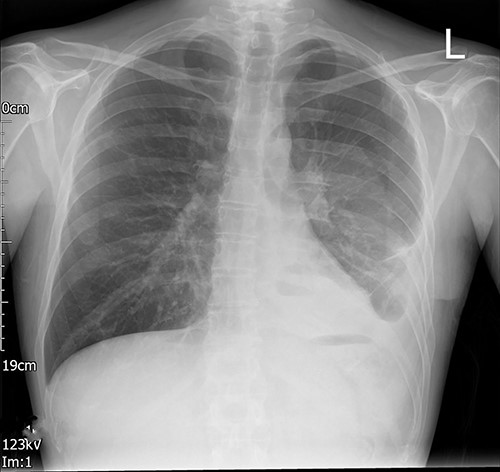
A young adult with a past medical history of asthma, depression and high alcohol intake was admitted with coronavirus (COVID) pneumonitis and type 2 respiratory failure. During his admission to the local hospital, he developed a left-sided pleural effusion. After confirming the diagnosis by a CT scan, an 18 French gauge (Fr) chest drain was inserted by the Seldinger technique (Fig. 1). The never event of a retained foreign body intrapleural was brought to light at the post-procedure X-ray (Fig. 2). The X-ray showed the retention of the guidewire in the thoracic cavity. The patient was referred to us for urgent retrieval of the guidewire. The patient was transferred, and a course of intravenous antibiotics for 10 days was completed, as per the advice of the infectious diseases colleagues; once the infection parameters were normal and the patient was COVID-19 negative, he underwent a left-sided video-assisted thoracoscopic surgery (VATS) for removal of the foreign body.


Posterior–anterior chest radiograph after chest drain insertion showing the retained guidewire in the left pleural cavity. In addition, left pleural effusion can be noted.
Left-sided uniportal VATS retrieval of the guidewire was done under general anesthesia (Video 1). The surgery was uneventful as was the post-operative recovery. The intercostal drain left in situ post-surgery was removed on a post-operative day (POD) 1 and the imaging done after the drain removal (Fig. 3) showed a significant decrease in pleural effusion with no guidewire in the chest cavity. He made a good recovery with an adequate physiotherapy assessment. The patient was discharged on a post-operative day (POD) 3. No follow-up was needed as he made a good recovery.
Left VATS post-operative posterior–anterior chest radiograph showing no guidewire in the left pleural cavity.
DISCUSSION
Foreign body retained in the body after a therapeutic or diagnostic procedure is a ‘never event’.
A recent report has reported the use of ultrasound to accurately pinpoint the location of a retained guidewire after a chest drain insertion [1]. They suggest the use of the technique in frail patients, who are not fit for general anesthesia and intubation, to assist in the removal of intrapleural foreign bodies under local anesthesia. VATS-guided surgery is an excellent, quick and safe technique to tackle the problem and can also deal effectively with the complications associated with the retention of a foreign body.
There is a high risk of incidence of retained foreign bodies in an emergency procedure, unplanned surgery, or in patients with a high body mass index [2]. The incidence of surgical instruments or swabs retained after surgery is maximum after abdominal operations (0.03–0.1%; [3]). Intrapleural foreign bodies are a rare occurrence and are rarely reported. Moreover, it was reported a total of 22 patients with intrapleural and intraparenchymal foreign bodies over 30 years from a single-center [4].
The risk factors for this iatrogenic never event are multifactorial.
A comprehensive review of the predisposing factors for surgery-related retention of foreign bodies stated that the recommendations for the prevention of the same, such as effective communication, good teamwork and the use of appropriate and timely imaging to diagnose the retention of a surgical instrument in a body cavity [5].
We present a unique case of a retained guidewire after drain insertion in a COVID infected patient. The drain was inserted into a critical care unit. The details of the events are not known but it was done as an emergency procedure in an uncooperative patient, which may have contributed to the occurrence of this event. Such iatrogenic phenomenon has medicolegal implications and hence it is the responsibility of the treating physician/surgeon to communicate with the patient regarding the event and the treatment necessary.
Seldinger intercostal chest drain is increasingly popular for chest drain insertion [6]. The technique should be carried out by practitioners who are trained and familiar with the equipment required for the procedure. Sticking to the guidelines set by the British Thoracic Society and correct insertion techniques will prevent such untoward and never event incidents of iatrogenic foreign body retaining into the chest cavity, which includes marking the appropriate site of insertion, introducing the needle into the chest wall followed by insertion of the guidewire, withdrawing the needle and passing a dilator over the guidewire, removing the dilator and inserting the drain by withdrawing the guidewire slowly till the tip is visible and then gently forcing the drain in as well as removing the guidewire till the drain is in place and finally securing the drain [7]. Should the guidewire be retained during the procedure then eliciting urgent action by radiology imaging and surgery should be instigated. Such never event incidents should be learned for patient safety.
Foreign bodies retained in the pleural space may have been underreported. An iatrogenic foreign body such as retained drain tip following intercostal drain (ICD) insertion has been reported and surgical removal is always performed [8]. Such avoidable incidents can be prevented by introducing Courses on chest drain insertion in acute hospital settings. Post-drain insertion X-ray is necessary to confirm the position of the tube and the degree of lung re-expansion and to exclude any complications.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



