-
PDF
- Split View
-
Views
-
Cite
Cite
Shuichiro Uchiyama, Naotaka Ikeda, Tomohiro Oyama, Mayumi Eguchi, Ayaka Ito, Rikiya Sato, Ryoichi Toyosaki, Masaki Kitazono, Toyokuni Suenaga, A case of post-operative stenosis caused by colonic ischemia after low anterior resection for rectal cancer, followed by delayed colo-anal anastomosis, Journal of Surgical Case Reports, Volume 2022, Issue 5, May 2022, rjac236, https://doi.org/10.1093/jscr/rjac236
Close - Share Icon Share
Abstract
Cases of delayed colo-anal anastomosis (DCAA) are currently reported instead of the colo-anal anastomosis with a protective loop ileostomy for rectal cancer. Post-operative colonic ischemia is considered as one of the serious complications of colorectal resection. Although indication of DCAA should be carefully selected, we experienced a case of post-operative stenosis caused by colonic ischemia after low anterior resection for rectal cancer, followed by this procedure.
INTRODUCTION
Post-operative colonic ischemia may be considered one of the more important complications of colorectal resection, and its incidence was reported as 0.83% of surgeries with high ligation (HL) of the inferior mesenteric artery (IMA) for sigmoid colon and rectal cancer [1]. Number of reports concerning cases of delayed colo-anal anastomosis (DCAA) instead of colo-anal anastomosis (CAA) with a protective loop ileostomy for rectal cancer is currently increasing. We herein report a case of post-operative stenosis caused by colonic ischemia after low anterior resection (LAR) for rectal cancer, followed by this procedure.
CASE REPORT
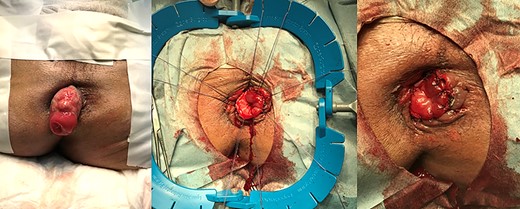
A 70-year-old man diagnosed with lower rectal cancer was admitted to our hospital for treatment. Colonoscopy revealed an uncirculated ulcerated tumor at the lower rectum. Tubular adenocarcinoma was diagnosed by histologic examination of the endoscopic biopsy specimen. Abdominal computed tomography showed limited thickening of the wall of the rectum, but there was no swelling of regional lymph nodes. No apparent distant metastasis including liver or lung metastasis was detected. Laparoscopic ultra-LAR and colorectal anastomosis (CRA) with protective loop ileostomy were performed. The intraabdominal drain and transanal drain were removed, and diet intake started 4 days after surgery. Massive diarrhea caused a rapid decrease in blood pressure, and vital signs stabilized immediately after treatment with infusion and vasopressor 11 days after surgery. Vancomycin was orally administered for the treatment of Clostridium difficile infection. The cause of shock turned out to be an ischemic change of the oral side of the anastomosis by endoscopic examination. Repeated endoscopic balloon dilatation for the stenotic portion for 5 months failed, and stoma care was firmly refused by the patient during this period (Fig. 1). Two ways of surgery were proposed for further treatment as the next step. One was permanent end colostomy, and the other was DCAA. Permanent stoma was refused and the latter one was selected. The operative procedure was performed as described in the following.

Endoscopic findings and gastrograffin enema 5 months after initial surgery.
First-stage operation
1. The patient was placed in a jackknife position, and transanal mucosectomy from the level of the dentate line to the oral side close to the anastomosis was performed, and transection of the previous anastomosis was completed.
2. After closure of the ileostomy, dissection of the middle colic artery and splenic flexure mobilization was performed laparoscopically in a reverse Trendelenburg and a semi-right lateral decubitus position.
3. Manual removal of the stenotic colon ~30 cm in length, including anastomosis, was performed after laparotomy.
4. The colonic stump was pulled through the anus, and ~5 cm of the distal colonic stump was left outside the anus.
Second-stage operation
Redundant colon was trimmed and hand-sewn anastomosis with interrupted absorbable sutures was performed in the lithotomy position 24 days after the first stage of surgery (Fig. 2).
The patient was discharged 17 days after the second-stage surgery. There was no anastomotic stenosis, and fecal soiling was hardly observed in our case. The patient remains satisfied more than 2 years after this surgery.
DISCUSSION
Although it is well accepted that a low anastomosis has a higher incidence of anastomotic leakage (AL), the mechanism remains unknown, and the hypothesis of the mechanism of AL is that the height of the anastomosis or the tumor location can reflect technical difficulties of LAR, resulting in local tissue trauma, increased tension or poor blood supply [2].
A fecal diversion is recommended as a selective tool to protect or ameliorate an anastomotic leak after a CRA in high-risk patients such as those with low colorectal anastomoses (<10 cm from the anal verge), CAAs, technically difficult resections, malnutrition and male patients [3]. Nurkin S et al. reviewed 525 cases of low rectal cancer having rectal resection with CAA, with or without a proximal stoma, and the results revealed that, in cases of CAA without fecal diversion, there was a significantly greater incidence of sepsis (P = 0.022), septic shock (P = 0.018) and need for reoperation (P = 0.0001) than those with diversion, and the length of hospital stay was significantly longer with CAA without diversion [4]. A diverting loop ileostomy is preferred to loop colostomy, and an ostomy should be used for a pelvic anastomosis <5–6 cm, including CAA and ileoanal pouch anastomosis [5]. DCAA, the so-called Turnbull and Cutait procedure was originally developed as an alternative to straight CRA in adult patients with mid-rectal cancer or rectal Chagas and children with Hirschsprung disease to avoid permanent stoma [6–8]. Portale G et al. reviewed the outcome of DCAA for eight observational studies and the results showed the benefits, including reduced risk of AL and pelvic sepsis and no need for protective ileostomy, with good functional and oncological outcomes [9]. Analysis of 92 patients revealed that DCAA can be considered as a valid alternative strategy that avoids a temporary stoma after a sphincteric-preserving ultra-LAR for low rectal cancer from the results of no different post-operative morbidity rate [10]. Post-operative colonic ischemia may be considered as one of the more important complications of colorectal resection [1] as well as AL. Hallet J et al. reported seven cases of anastomotic salvage, including one ischemic case, after rectal cancer resection using DCAA, and six of seven (85.7%) DCAA cases were completed except for one requiring an abdominoperineal resection with a permanent colostomy post-DCAA after extensive colonic ischemia. They concluded that this technique appeared to be a safe procedure and could be offered to patients with complex anastomotic complications [8]. We performed LAR with HL of the IMA with diverting loop ileostomy for low rectal cancer, but post-operative colonic ischemia caused the stenosis at the oral side of the anastomosis, although AL was not observed. There was no anastomotic stenosis after DCAA, and fecal soiling was hardly observed. Preservation of internal anal sphincter muscle at the initial rectal surgery may give favorable outcome, and the patient remains satisfied more than 2 years after surgery.
CONCLUSION
We experienced DCAA for the case of post-operative colonic ischemia after LAR. Although indication of DCAA for surgery should be carefully selected, this procedure can be one of the candidates for post-operative complicated cases.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



