-
PDF
- Split View
-
Views
-
Cite
Cite
Sabina Patel, Trisha Suji, Graeme Pang, Varinder S Alg, Ravindran Visagan, Zita Reisz, Jose P Lavrador, Ahilan Kailaya-Vasan, Gordan Grahovac, Spinal myxomas: review of a rare entity, Journal of Surgical Case Reports, Volume 2022, Issue 5, May 2022, rjac221, https://doi.org/10.1093/jscr/rjac221
Close - Share Icon Share
Abstract
Intramuscular myxomas are rare, benign mesenchymal tumours, occurring predominantly in large skeletal muscles as large, slow-growing and painless masses. Spinal occurrence is rare, and may present incidentally, or diagnosed via localized symptoms secondary to local infiltration of surrounding structures. Differential diagnosis based on imaging includes sarcomas, meningiomas and lipomas. We discuss two contrasting cases presenting with well-circumscribed cystic paraspinal lesions indicative of an infiltrative tumour and discuss the radiological and histological differences that distinguish myxomas from similar tumours. Surgical resection of the tumour was performed in both cases, however one patient required surgical fixation due to bony erosion secondary to tumour infiltration. Immuno-histopathological analysis confirmed the diagnosis of a cellular myxoma. Follow up imaging at 6 months confirmed no symptomatic or tumour recurrence in both cases. Histological analysis is the definitive means for diagnosis to differentiate myxomas from other tumours. Recurrence is rare if full resection is achieved.
INTRODUCTION
Intramuscular myxomas are rare, benign soft tissue tumours, commonly occurring in muscles such as the thigh, buttocks and upper arm/ shoulder [1]. First described in 1965 by Enzinger and Weiss [2], intramuscular tumours represent a subgroup of all myxomas, presenting as deep seated, slow growing masses confined within skeletal muscle [3, 4]. Although many intramuscular myxomas are asymptomatic and discovered incidentally, a small subset can cause localized symptoms, because of their ability to infiltrate into adjacent muscles and soft tissue, made possible by a lack of a true capsule [2, 3, 5]. The few reported cases of spinal intramuscular myxomas describe the lesions to be benign yet locally invasive [6], and characteristically occur in the adult stages of life, with a higher preponderance towards females. We present two cases and review the available literature and diagnostic criteria.
CASE SERIES
Case one
A 77-year-old female was reviewed in the spinal clinic with an incidental finding of a cervical mass, discovered on radiological imaging following a fall. The patient described a pressure type sensation in the head, neck and left arm when bending down. The symptoms were aggravated on arm movement. There were no associated motor or sensory deficits, no new bladder or bowel dysfunction and no new gait disturbance. Examination confirmed intact power and reflexes in all four limbs.
Pre-operative spinal imaging showed a well-circumscribed, cystic parasagittal spinal mass eroding through the lamina and pushing the thecal sac and largely indicative of a paraspinal myxoma (Fig. 1). The patient underwent a biopsy in the first instance to guide diagnosis and subsequently proceeded to resection of the tumour.
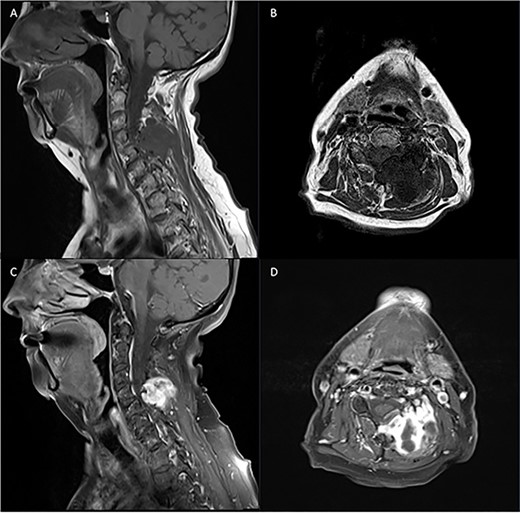
Pre-operative T1 and T2 weighted MRI: left-sided extra-axial mass at C4/5 hypointense on T1 and hyperintense on T2.
Tumour resection was performed through a posterior midline cervical incision. Muscle dissection revealed the tumour plane over the left paraspinal region with associated bony erosion secondary to the tumour at C4/5. The tumour was removed with good thecal decompression at the end of the procedure, with additional placement of lateral mass screws due to the bony erosion.
Histological analysis one main large fragment of soft tissue infiltrated by a multinodular tumour with gelatinous consistency.
Histological sections showed multiple large pieces of a myxoid tumour separated by a pseudocapsule from the surrounding fibro-adipose tissue, skeletal muscle and peripheral nerve fascicles. The neoplastic cells were relatively uniform and composed of elongated hyperchromatic nuclei with long eosinophilic cytoplasmic processes. There are focal cystic changes. Mitotic figures were inconspicuous and there was no evidence of necrosis. Immunohistochemistry showed that many but not all tumour cells were reactive to smooth muscle actin (SMA), negative for S100 protein, desmin, MNF116 and NF and equivocal focally for epithelial membrane antigen (EMA) and CD34.
The initial overall features were those of a myxoid/microcystic mesenchymal tumour with no hypercellularity or significant cytological atypia, mitotic activity or necrosis. According to the localization, morphological features and immunohistochemical characteristics, the differential diagnosis included a benign peripheral nerve sheath tumour or an intramuscular myxoma, although other myxoid mesenchymal tumours could not be entirely excluded.
On further immunohistochemistry analysis, the sample showed negativity for EMA, claudin-1, GLUT1, MUC4, SOX10 and D2-40. Insufficient atypia ruled out a diagnosis of myxofibrosarcoma, and the negative MUC4 helped to exclude low-grade fibromyxoid sarcoma. Other nerve sheath tumours appear to be excluded by the immunohistochemistry.
Given the radiological, morphological and immunohistochemistry features, the overall features were suggestive of a low-grade myxoid tumour, most in keeping with an intramuscular myxoma (Fig. 2A and B).
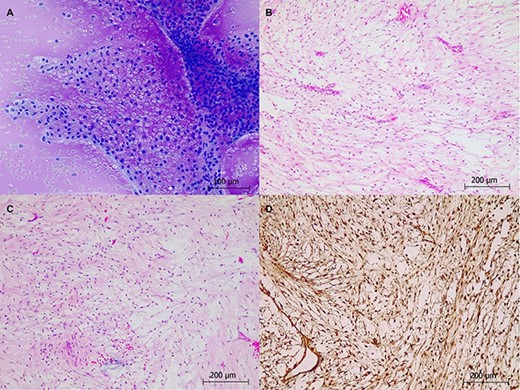
Histological staining of intraoperative tumour smears: (A) intraoperative smear Toluidine blue stained slide. (B): H&E ×10. (C): H&E ×10. (D): vimentin IHC ×10.
Pre-operative T1 post Gadolinium and T2 weighted MRI: left-sided extra-axial mass at C5/6 with heterogenous enhancement on T1 and hyperintense on T2. Moderate compression of the spinal cord and invasion into surrounding soft tissue.
Post-operatively, the patient made a full recovery with no new motor or sensory disturbances. She was discharged home with no further therapy input required. Follow up imaging at 3 months showed normal post-operative changes at the site of surgery with no evidence of tumour recurrence.
Case two
A 72-year-old, right-handed female was admitted emergently with a 5-week history of left sided shoulder pain, radiating to the neck and upper arm in a C5 distribution, reduced manual dexterity as well paraesthesia in all four extremities and loss of balance. The patient denied any bowel or bladder symptoms.
Pre-operative examination confirmed Medical Research Council (MRC) grade 4/5 power in the left upper limb and 5/5 power in all other limbs. Reflexes were intact bilaterally, and Hoffman’s sign was not elicited.
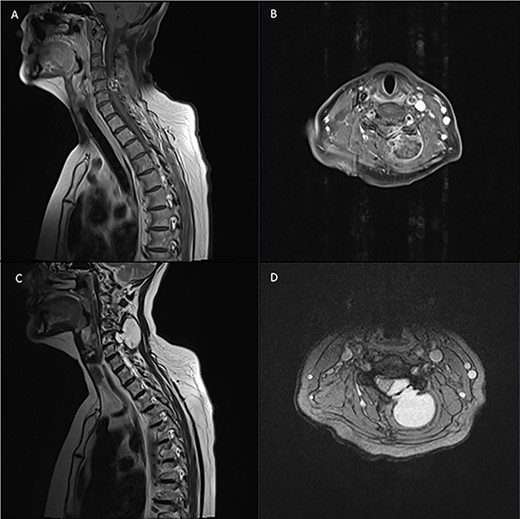
Diagnostic spinal imaging showed a large mixed cystic solid destructive bony lesion arising from the bony elements at C5 with heterogenous enhancement (Fig. 3). A chest/abdomen/pelvic CT did not identify any further lesions.
The patient underwent surgical resection through a unilateral left sided incision. A tumour capsule was identified in the surrounding muscle and soft tissue and subsequently dissected. C5/6 partial laminectomies were performed, which identified an intracanalicular component of the tumour. The tumour was removed en bloc, with relaxed theca at the end of the procedure (Fig. 4).

Tumour specimen resected en bloc. Solitary, relatively well-delineated nodule covered by a thick capsule measuring 30 × 25 × 20 mm.
Gross examination of the tumour showed a solitary, relatively well-delineated nodule covered by a thick capsule. The parenchyma was relatively homogeneous with cystic areas, evidence of adjacent soft tissue and fresh haemorrhage.
Histological staining showed a relatively encapsulated hypocellular tumour adjacent to skeletal muscle, fibroadipose tissue and some entrapped peripheral nerve fascicles. The tumour was surrounded by variably collagenised capsule, which separated the main lesion into smaller tumoural nodules. The neoplastic cells were relatively monomorphic, with spindle to stellate morphology, small oval hyperchromatic nuclei, loose myxoid background and areas of cystic changes. Mildly increased cellularity and occasional macrophages were also visible. No significant nuclear pleomorphism, mitoses or necrosis was evident.
Immunohistochemistry showed reactivity to SMA, vimentin and EMA. S100 was expressed in a lesser proportion of cells, particularly in those with stellate morphology. Additional immunohistochemistry was negative for MUC4 and X10. Overall, the morphological and immunohistochemical features were most suggestive of an intramuscular myxoma (Fig. 2 C and D).
Post-operatively, the patient showed improved left upper limb power to MRC grade 4+/5. Sensory examination showed reduced sensation in C7 and C8 bilaterally and normal sensation in all other dermatomes. Proprioception was reduced in the upper limbs and remained intact in the lower limbs. The patient was subsequently discharged home with community therapy follow up.
Follow up imaging at 3 months did not show any evidence of tumour recurrence.
DISCUSSION
The incidence of intramuscular myxomas is estimated at 1/1 000 000 with <20 cases reported in the spine [2, 3, 6].
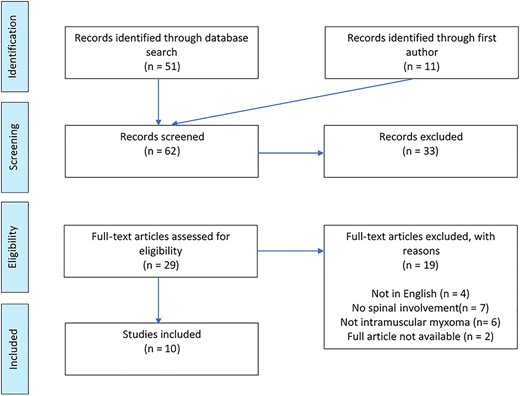
A PubMed literature search for ‘[spinal] AND [myxoma]’ combined with ‘[case] OR [record]] OR [history] OR [documented] OR [patient] OR [report] OR [file]’ revealed 10 reports available for review (Tables 1 and 2; Fig. 5).
Radiating pain with or without neurological deficits was the chief presenting complaint in many reported cases, spanning a timescale from days to years. Findings of a palpable mass were also reported in some of the cases, however little reference was made as to whether these were painful or painless [1, 7, 8]. The strong history of pain in paraspinal myxomas differs in comparison to intramuscular myxomas in other regions, which are more likely to be asymptomatic and discovered via a slow growing painless mass [9].
| Title . | Age/ Gender . | Vertebral Level . | Symptoms . | Palpable Mass . | Radiological Findings . | Tumour Dimensions . | Treatment . | Operative Findings . | Histological Findings . | Diagnosis . | Recurrence at Follow-Up . |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Patel et al, 2021 | 72F | C5 | Paraesthesia in all limbs | Yes | Heterogenously enhancing mixed cystic solid lesion | 38 mm × 30 mm | Laminectomy and tumour resection | Capsulated tumour invading muscle and soft tissue | SMA +ive S100 +ive No mitotic figures or necrosis | Intramuscular Myxoma | Symptomatic improvement, no recurrence at 3 months |
| Patel et al, 2021 | 77F | C4-5 | N | No | Cystic mass | - | Biopsy, tumour resection, and spinal fixation | - | SMA +ive S100 -ive No atypica, mitotic figures, or necrosis | Intramuscular Myxoma | No recurrence at 3 months |
| Tahmouresie et al, 1981[8] | 50M | T11-T12 | Lower limb motor and sensory disturbance | Y | Extradural | - | Lamnectomy and tumour Resection | Gelatinous tumour with bony erosion Spinal cord compression, no infiltration | Alcian blue positive Mucicarmine stain: faint pink | Myxoma | Symptomatic improvement – no recurrence |
| Bell, W.O et al, 1983[4] | 60M | L3-L4 | Unilateral reduced sensation on right plantar surface | No | epidural | 1 × 2 × 0.5 cm | Laminectomy and tumour Resection | Firm epidural mass, compressive and adherent to dura | Hypocellular, avascular tumour Oval-spindle shaped nuclei No mitotic figures, atypia, necrosis | Myxoma | No tumour recurrence |
| Pasaoglu et al, 1988[16] | 18th Month old Male | C3-T1 | UL weakness | No | Intramedullary tumour | 4 × 1.5 × 1 cm | Laminectomy and tumour resection | Gelatinous tumour with poor vascularisation Adhered to surrounding cord | Hypocellular Stellate and spindle shaped cells Alcian blue +ive Absent necrosis and mitotic figures | Myxoma | No recurrence |
| Kamoun et al, 1997[14] | 54F | L3-L4 | Sciatica, Back pain and neurological signs | - | - | - | Needle biopsy and surgical excision | - | - | Intramuscular Myxoma | 3 years – No recurrence |
| Guppy et al, 2001[15] | 80F | L5-S1 | Lower back pain and radiculopathy. | Y | Paraspinal mass invading L-5 vertebral body and leaving foramen of L5-S1 Second cystic lesion inferiorly. | 70 mm | Laminotomy and tumour resection | Mass protrudes through paraspinal muscle into L5 pedicle and vertebral body. Second mass opened releasing clear viscous fluid, lining of cyst removed. | S100: - EMA: - No mitotic activity, haemorrhage, or necrosis. Monotonous spindle cells, with cytologically bland stellate and bipolar fibroblasts | Intramuscular Myxoma | 3 months – No recurrence |
| Stinchcombe et al, 2010[12] | 80F | L2-S1 | Pain, no deficits | N | T2 hyperintensity | 40 × 40 × 30 mm | Biopsy with paraspinal debridement and drainage | gelatinous mass, containing loculated material | Hypocellular Stellate cells No mitotic figures, no necrosis | Intramuscular Myxoma | Not commented |
| Taggarshe et al, 2010[12] | 52F | Lumbar | No | Y | T1 hypointense T2 hyperintense Contrast enhancing | 12.5 × 6.2 × 3.5 cm | Paraspinal resection | Mucinous cystic spaces, thin sheath of surrounding soft tissue | S-100 -ve Spindle shaped, myxoid appearance, moderately cellular/vascular | Myxoma | Symptomatic improvement at 3 months |
| Ohla et al, 2013[10] | 57F | L5 | N | N | T1 hypointense T2 hyperintense Contrast enhancing | 3.0 × 3.0 × 3.5 cm | Paraspinal resection | Well encapsulated, deep in paraspinal muscles, adherent to periosteum of L5 and S1 | Myxoid spindle cell tumor without significant atypia. no mitotic activity, necrosis, or increase in nuclear atypia Increased cellularity and vascularity S100 -ive | Myxoma | No recurrence |
| Manoharan et al, 2014[1] | 63F | C4-C5 | N | Y | - | 2.7 × 1.6 × 3.8 cm | Tumour resection | Tumour is primarily well circumscribed, encapsulated, and firm, extending into spinal canal | S100: + Vimentin: + CD34: + | Infiltrative Intramuscular Myxoma | No recurrence at 18 months |
| Choi et al, 2015[5] | 62F | L4-L5 | LBP No deficits | Y | T1 Hypointensity T2 hyperintensity | 4 × 3.5 × 6.5 cm | Paraspinal resection | Enscapulated tumour, no evidence of local invasion or infiltration | Spindle-stellate cells No mitotic activity, haemorrhage, or necrosis | Myxoid tumour | - |
| Title . | Age/ Gender . | Vertebral Level . | Symptoms . | Palpable Mass . | Radiological Findings . | Tumour Dimensions . | Treatment . | Operative Findings . | Histological Findings . | Diagnosis . | Recurrence at Follow-Up . |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Patel et al, 2021 | 72F | C5 | Paraesthesia in all limbs | Yes | Heterogenously enhancing mixed cystic solid lesion | 38 mm × 30 mm | Laminectomy and tumour resection | Capsulated tumour invading muscle and soft tissue | SMA +ive S100 +ive No mitotic figures or necrosis | Intramuscular Myxoma | Symptomatic improvement, no recurrence at 3 months |
| Patel et al, 2021 | 77F | C4-5 | N | No | Cystic mass | - | Biopsy, tumour resection, and spinal fixation | - | SMA +ive S100 -ive No atypica, mitotic figures, or necrosis | Intramuscular Myxoma | No recurrence at 3 months |
| Tahmouresie et al, 1981[8] | 50M | T11-T12 | Lower limb motor and sensory disturbance | Y | Extradural | - | Lamnectomy and tumour Resection | Gelatinous tumour with bony erosion Spinal cord compression, no infiltration | Alcian blue positive Mucicarmine stain: faint pink | Myxoma | Symptomatic improvement – no recurrence |
| Bell, W.O et al, 1983[4] | 60M | L3-L4 | Unilateral reduced sensation on right plantar surface | No | epidural | 1 × 2 × 0.5 cm | Laminectomy and tumour Resection | Firm epidural mass, compressive and adherent to dura | Hypocellular, avascular tumour Oval-spindle shaped nuclei No mitotic figures, atypia, necrosis | Myxoma | No tumour recurrence |
| Pasaoglu et al, 1988[16] | 18th Month old Male | C3-T1 | UL weakness | No | Intramedullary tumour | 4 × 1.5 × 1 cm | Laminectomy and tumour resection | Gelatinous tumour with poor vascularisation Adhered to surrounding cord | Hypocellular Stellate and spindle shaped cells Alcian blue +ive Absent necrosis and mitotic figures | Myxoma | No recurrence |
| Kamoun et al, 1997[14] | 54F | L3-L4 | Sciatica, Back pain and neurological signs | - | - | - | Needle biopsy and surgical excision | - | - | Intramuscular Myxoma | 3 years – No recurrence |
| Guppy et al, 2001[15] | 80F | L5-S1 | Lower back pain and radiculopathy. | Y | Paraspinal mass invading L-5 vertebral body and leaving foramen of L5-S1 Second cystic lesion inferiorly. | 70 mm | Laminotomy and tumour resection | Mass protrudes through paraspinal muscle into L5 pedicle and vertebral body. Second mass opened releasing clear viscous fluid, lining of cyst removed. | S100: - EMA: - No mitotic activity, haemorrhage, or necrosis. Monotonous spindle cells, with cytologically bland stellate and bipolar fibroblasts | Intramuscular Myxoma | 3 months – No recurrence |
| Stinchcombe et al, 2010[12] | 80F | L2-S1 | Pain, no deficits | N | T2 hyperintensity | 40 × 40 × 30 mm | Biopsy with paraspinal debridement and drainage | gelatinous mass, containing loculated material | Hypocellular Stellate cells No mitotic figures, no necrosis | Intramuscular Myxoma | Not commented |
| Taggarshe et al, 2010[12] | 52F | Lumbar | No | Y | T1 hypointense T2 hyperintense Contrast enhancing | 12.5 × 6.2 × 3.5 cm | Paraspinal resection | Mucinous cystic spaces, thin sheath of surrounding soft tissue | S-100 -ve Spindle shaped, myxoid appearance, moderately cellular/vascular | Myxoma | Symptomatic improvement at 3 months |
| Ohla et al, 2013[10] | 57F | L5 | N | N | T1 hypointense T2 hyperintense Contrast enhancing | 3.0 × 3.0 × 3.5 cm | Paraspinal resection | Well encapsulated, deep in paraspinal muscles, adherent to periosteum of L5 and S1 | Myxoid spindle cell tumor without significant atypia. no mitotic activity, necrosis, or increase in nuclear atypia Increased cellularity and vascularity S100 -ive | Myxoma | No recurrence |
| Manoharan et al, 2014[1] | 63F | C4-C5 | N | Y | - | 2.7 × 1.6 × 3.8 cm | Tumour resection | Tumour is primarily well circumscribed, encapsulated, and firm, extending into spinal canal | S100: + Vimentin: + CD34: + | Infiltrative Intramuscular Myxoma | No recurrence at 18 months |
| Choi et al, 2015[5] | 62F | L4-L5 | LBP No deficits | Y | T1 Hypointensity T2 hyperintensity | 4 × 3.5 × 6.5 cm | Paraspinal resection | Enscapulated tumour, no evidence of local invasion or infiltration | Spindle-stellate cells No mitotic activity, haemorrhage, or necrosis | Myxoid tumour | - |
| Title . | Age/ Gender . | Vertebral Level . | Symptoms . | Palpable Mass . | Radiological Findings . | Tumour Dimensions . | Treatment . | Operative Findings . | Histological Findings . | Diagnosis . | Recurrence at Follow-Up . |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Patel et al, 2021 | 72F | C5 | Paraesthesia in all limbs | Yes | Heterogenously enhancing mixed cystic solid lesion | 38 mm × 30 mm | Laminectomy and tumour resection | Capsulated tumour invading muscle and soft tissue | SMA +ive S100 +ive No mitotic figures or necrosis | Intramuscular Myxoma | Symptomatic improvement, no recurrence at 3 months |
| Patel et al, 2021 | 77F | C4-5 | N | No | Cystic mass | - | Biopsy, tumour resection, and spinal fixation | - | SMA +ive S100 -ive No atypica, mitotic figures, or necrosis | Intramuscular Myxoma | No recurrence at 3 months |
| Tahmouresie et al, 1981[8] | 50M | T11-T12 | Lower limb motor and sensory disturbance | Y | Extradural | - | Lamnectomy and tumour Resection | Gelatinous tumour with bony erosion Spinal cord compression, no infiltration | Alcian blue positive Mucicarmine stain: faint pink | Myxoma | Symptomatic improvement – no recurrence |
| Bell, W.O et al, 1983[4] | 60M | L3-L4 | Unilateral reduced sensation on right plantar surface | No | epidural | 1 × 2 × 0.5 cm | Laminectomy and tumour Resection | Firm epidural mass, compressive and adherent to dura | Hypocellular, avascular tumour Oval-spindle shaped nuclei No mitotic figures, atypia, necrosis | Myxoma | No tumour recurrence |
| Pasaoglu et al, 1988[16] | 18th Month old Male | C3-T1 | UL weakness | No | Intramedullary tumour | 4 × 1.5 × 1 cm | Laminectomy and tumour resection | Gelatinous tumour with poor vascularisation Adhered to surrounding cord | Hypocellular Stellate and spindle shaped cells Alcian blue +ive Absent necrosis and mitotic figures | Myxoma | No recurrence |
| Kamoun et al, 1997[14] | 54F | L3-L4 | Sciatica, Back pain and neurological signs | - | - | - | Needle biopsy and surgical excision | - | - | Intramuscular Myxoma | 3 years – No recurrence |
| Guppy et al, 2001[15] | 80F | L5-S1 | Lower back pain and radiculopathy. | Y | Paraspinal mass invading L-5 vertebral body and leaving foramen of L5-S1 Second cystic lesion inferiorly. | 70 mm | Laminotomy and tumour resection | Mass protrudes through paraspinal muscle into L5 pedicle and vertebral body. Second mass opened releasing clear viscous fluid, lining of cyst removed. | S100: - EMA: - No mitotic activity, haemorrhage, or necrosis. Monotonous spindle cells, with cytologically bland stellate and bipolar fibroblasts | Intramuscular Myxoma | 3 months – No recurrence |
| Stinchcombe et al, 2010[12] | 80F | L2-S1 | Pain, no deficits | N | T2 hyperintensity | 40 × 40 × 30 mm | Biopsy with paraspinal debridement and drainage | gelatinous mass, containing loculated material | Hypocellular Stellate cells No mitotic figures, no necrosis | Intramuscular Myxoma | Not commented |
| Taggarshe et al, 2010[12] | 52F | Lumbar | No | Y | T1 hypointense T2 hyperintense Contrast enhancing | 12.5 × 6.2 × 3.5 cm | Paraspinal resection | Mucinous cystic spaces, thin sheath of surrounding soft tissue | S-100 -ve Spindle shaped, myxoid appearance, moderately cellular/vascular | Myxoma | Symptomatic improvement at 3 months |
| Ohla et al, 2013[10] | 57F | L5 | N | N | T1 hypointense T2 hyperintense Contrast enhancing | 3.0 × 3.0 × 3.5 cm | Paraspinal resection | Well encapsulated, deep in paraspinal muscles, adherent to periosteum of L5 and S1 | Myxoid spindle cell tumor without significant atypia. no mitotic activity, necrosis, or increase in nuclear atypia Increased cellularity and vascularity S100 -ive | Myxoma | No recurrence |
| Manoharan et al, 2014[1] | 63F | C4-C5 | N | Y | - | 2.7 × 1.6 × 3.8 cm | Tumour resection | Tumour is primarily well circumscribed, encapsulated, and firm, extending into spinal canal | S100: + Vimentin: + CD34: + | Infiltrative Intramuscular Myxoma | No recurrence at 18 months |
| Choi et al, 2015[5] | 62F | L4-L5 | LBP No deficits | Y | T1 Hypointensity T2 hyperintensity | 4 × 3.5 × 6.5 cm | Paraspinal resection | Enscapulated tumour, no evidence of local invasion or infiltration | Spindle-stellate cells No mitotic activity, haemorrhage, or necrosis | Myxoid tumour | - |
| Title . | Age/ Gender . | Vertebral Level . | Symptoms . | Palpable Mass . | Radiological Findings . | Tumour Dimensions . | Treatment . | Operative Findings . | Histological Findings . | Diagnosis . | Recurrence at Follow-Up . |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Patel et al, 2021 | 72F | C5 | Paraesthesia in all limbs | Yes | Heterogenously enhancing mixed cystic solid lesion | 38 mm × 30 mm | Laminectomy and tumour resection | Capsulated tumour invading muscle and soft tissue | SMA +ive S100 +ive No mitotic figures or necrosis | Intramuscular Myxoma | Symptomatic improvement, no recurrence at 3 months |
| Patel et al, 2021 | 77F | C4-5 | N | No | Cystic mass | - | Biopsy, tumour resection, and spinal fixation | - | SMA +ive S100 -ive No atypica, mitotic figures, or necrosis | Intramuscular Myxoma | No recurrence at 3 months |
| Tahmouresie et al, 1981[8] | 50M | T11-T12 | Lower limb motor and sensory disturbance | Y | Extradural | - | Lamnectomy and tumour Resection | Gelatinous tumour with bony erosion Spinal cord compression, no infiltration | Alcian blue positive Mucicarmine stain: faint pink | Myxoma | Symptomatic improvement – no recurrence |
| Bell, W.O et al, 1983[4] | 60M | L3-L4 | Unilateral reduced sensation on right plantar surface | No | epidural | 1 × 2 × 0.5 cm | Laminectomy and tumour Resection | Firm epidural mass, compressive and adherent to dura | Hypocellular, avascular tumour Oval-spindle shaped nuclei No mitotic figures, atypia, necrosis | Myxoma | No tumour recurrence |
| Pasaoglu et al, 1988[16] | 18th Month old Male | C3-T1 | UL weakness | No | Intramedullary tumour | 4 × 1.5 × 1 cm | Laminectomy and tumour resection | Gelatinous tumour with poor vascularisation Adhered to surrounding cord | Hypocellular Stellate and spindle shaped cells Alcian blue +ive Absent necrosis and mitotic figures | Myxoma | No recurrence |
| Kamoun et al, 1997[14] | 54F | L3-L4 | Sciatica, Back pain and neurological signs | - | - | - | Needle biopsy and surgical excision | - | - | Intramuscular Myxoma | 3 years – No recurrence |
| Guppy et al, 2001[15] | 80F | L5-S1 | Lower back pain and radiculopathy. | Y | Paraspinal mass invading L-5 vertebral body and leaving foramen of L5-S1 Second cystic lesion inferiorly. | 70 mm | Laminotomy and tumour resection | Mass protrudes through paraspinal muscle into L5 pedicle and vertebral body. Second mass opened releasing clear viscous fluid, lining of cyst removed. | S100: - EMA: - No mitotic activity, haemorrhage, or necrosis. Monotonous spindle cells, with cytologically bland stellate and bipolar fibroblasts | Intramuscular Myxoma | 3 months – No recurrence |
| Stinchcombe et al, 2010[12] | 80F | L2-S1 | Pain, no deficits | N | T2 hyperintensity | 40 × 40 × 30 mm | Biopsy with paraspinal debridement and drainage | gelatinous mass, containing loculated material | Hypocellular Stellate cells No mitotic figures, no necrosis | Intramuscular Myxoma | Not commented |
| Taggarshe et al, 2010[12] | 52F | Lumbar | No | Y | T1 hypointense T2 hyperintense Contrast enhancing | 12.5 × 6.2 × 3.5 cm | Paraspinal resection | Mucinous cystic spaces, thin sheath of surrounding soft tissue | S-100 -ve Spindle shaped, myxoid appearance, moderately cellular/vascular | Myxoma | Symptomatic improvement at 3 months |
| Ohla et al, 2013[10] | 57F | L5 | N | N | T1 hypointense T2 hyperintense Contrast enhancing | 3.0 × 3.0 × 3.5 cm | Paraspinal resection | Well encapsulated, deep in paraspinal muscles, adherent to periosteum of L5 and S1 | Myxoid spindle cell tumor without significant atypia. no mitotic activity, necrosis, or increase in nuclear atypia Increased cellularity and vascularity S100 -ive | Myxoma | No recurrence |
| Manoharan et al, 2014[1] | 63F | C4-C5 | N | Y | - | 2.7 × 1.6 × 3.8 cm | Tumour resection | Tumour is primarily well circumscribed, encapsulated, and firm, extending into spinal canal | S100: + Vimentin: + CD34: + | Infiltrative Intramuscular Myxoma | No recurrence at 18 months |
| Choi et al, 2015[5] | 62F | L4-L5 | LBP No deficits | Y | T1 Hypointensity T2 hyperintensity | 4 × 3.5 × 6.5 cm | Paraspinal resection | Enscapulated tumour, no evidence of local invasion or infiltration | Spindle-stellate cells No mitotic activity, haemorrhage, or necrosis | Myxoid tumour | - |
| Demographics (n=10) . | n . | |
|---|---|---|
| Gender | Male | 3 |
| Female | 7 | |
| Age | 0-20 | 1 |
| 20-40 | 0 | |
| 40-60 | 5 | |
| >61 | 4 | |
| Spinal Level | Cervical Spine | 2 |
| Thoracic Spine | 1 | |
| Lumbar/Sacral Spine | 7 | |
| Symptomatic | Pain | 3 |
| Neurological deficits | 5 | |
| Palpable mass | 5 | |
| Treatment | Surgical excision | 10 |
| Conservative management | 0 | |
| Follow up | Symptomatic improvement | 10 |
| Tumour recurrence at follow up | 0 | |
| Demographics (n=10) . | n . | |
|---|---|---|
| Gender | Male | 3 |
| Female | 7 | |
| Age | 0-20 | 1 |
| 20-40 | 0 | |
| 40-60 | 5 | |
| >61 | 4 | |
| Spinal Level | Cervical Spine | 2 |
| Thoracic Spine | 1 | |
| Lumbar/Sacral Spine | 7 | |
| Symptomatic | Pain | 3 |
| Neurological deficits | 5 | |
| Palpable mass | 5 | |
| Treatment | Surgical excision | 10 |
| Conservative management | 0 | |
| Follow up | Symptomatic improvement | 10 |
| Tumour recurrence at follow up | 0 | |
| Demographics (n=10) . | n . | |
|---|---|---|
| Gender | Male | 3 |
| Female | 7 | |
| Age | 0-20 | 1 |
| 20-40 | 0 | |
| 40-60 | 5 | |
| >61 | 4 | |
| Spinal Level | Cervical Spine | 2 |
| Thoracic Spine | 1 | |
| Lumbar/Sacral Spine | 7 | |
| Symptomatic | Pain | 3 |
| Neurological deficits | 5 | |
| Palpable mass | 5 | |
| Treatment | Surgical excision | 10 |
| Conservative management | 0 | |
| Follow up | Symptomatic improvement | 10 |
| Tumour recurrence at follow up | 0 | |
| Demographics (n=10) . | n . | |
|---|---|---|
| Gender | Male | 3 |
| Female | 7 | |
| Age | 0-20 | 1 |
| 20-40 | 0 | |
| 40-60 | 5 | |
| >61 | 4 | |
| Spinal Level | Cervical Spine | 2 |
| Thoracic Spine | 1 | |
| Lumbar/Sacral Spine | 7 | |
| Symptomatic | Pain | 3 |
| Neurological deficits | 5 | |
| Palpable mass | 5 | |
| Treatment | Surgical excision | 10 |
| Conservative management | 0 | |
| Follow up | Symptomatic improvement | 10 |
| Tumour recurrence at follow up | 0 | |
Radiologically, intramuscular myxomas appear as well-defined, contrast enhancing, homogenous lesions on magnetic resonance imaging (MRI), with low intensity signal on T1 weighted imaging and high intensity signal on T2 weighted imaging. Differential diagnoses include schwannomas, lipomas, liposarcomas, meningiomas, neurofibromas, paragangliomas and leptomeningeal spread [10, 11].
The definitive means of diagnosis is tissue sampling through surgical intervention. Intraoperative findings typically demonstrate poorly circumscribed infiltrative borders, cystic components and mucoid, gelatinous masses. A simple laminectomy appears to be the preferred surgical intervention of choice, particularly in cases of bony involvement [8]. However, surgical intervention can be limited to skin and muscle incisions in the cases where the masses are confined to soft tissue elements only [5, 10–16]. In our series, one patient underwent spinal fixation due to concerns of the integrity of the bone secondary to tumour infiltration, which has not been previously reported.
Stout first outlined histological diagnostic criteria for intramuscular myxomas in 1948, as ‘a mesenchymal non-metastatic neoplasm composed solely of undifferentiated stellate cells, surrounded by a loose mucoid stroma’ [6]. In addition, intramuscular myxomas characteristically lack nuclear atypia, necrosis and prominent mitotic activity, differentiating them from other myxoid lesions, whereas the absence of vascularity distinguishes these tumours from sarcoma [3, 5]. Although the immunophenotype for myxomas is generally non-specific, many display positive staining for Vimentin and occasionally for SMA and CD34, but negative for S-100, which is more likely to point towards a diagnosis of myxoid neurofibromas and low-grade malignant peripheral nerve sheath tumours [3, 17–19]. Interestingly, one case in our series and several cases in the literature review showed mild positivity for S-100.
Intramuscular myxomas carry a good prognosis due to a low metastatic rate, and surgical resection is the preferred treatment option to avoid local recurrence [11]. As was the case in our patient group, post-operative recovery can be almost immediate, with low likelihood of tumour recurrence on follow up imaging.
CONCLUSION
Paraspinal myxomas are benign tumours, arising from paraspinal musculature that can present incidentally or with neurological deficits secondary to local infiltration. Diagnosis is one of exclusion, based on location, radiological appearances and histological staining, which differentiates paraspinal myxomas from similar tumours such as sarcomas and other myxoid tumours. Tumour recurrence is rare and complete resection provides high scope for complete post-operative recovery.
DATA AVAILABILITY
The authors confirm that the data supporting the findings of this study are available within the article and its supplementary materials.
AUTHORS’ CONTRIBUTIONS
All authors contributed equally to the drafting and revision of this paper.
CONFLICT OF INTEREST STATEMENT
All authors declare that they have no conflict of interest.
FUNDING
No funding was received for this research.
ETHICAL APPROVAL
This article does not contain any studies with human participants or animals performed by any of the authors.



