-
PDF
- Split View
-
Views
-
Cite
Cite
Takuya Ohashi, Mitsumasa Kawago, Yoshimitsu Hirai, Megumi Kiyoi, Miwako Miyasaka, Yumi Yata, Mari Kawaji, Aya Fusamoto, Hideto Iguchi, Hitomi Nakanishi, Yoshiharu Nishimura, Pulmonary vein thrombosis following a right upper lobectomy preceding acute arterial occlusion: a case report, Journal of Surgical Case Reports, Volume 2022, Issue 5, May 2022, rjac168, https://doi.org/10.1093/jscr/rjac168
Close - Share Icon Share
Abstract
Our medical team observed a right upper lobe nodule in a 78-year-old man who was treated with warfarin for chronic atrial fibrillation. The nodule was diagnosed as adenocarcinoma via intraoperative frozen sectioning. We performed video-assisted right upper lobectomy and mediastinal lymph node dissection. Warfarin was discontinued in the perioperative period. However, unfractionated heparin was administered. Nonetheless, the patient developed acute arterial occlusion of the lower extremities on post-operative day 7. Contrast-enhanced computed tomography showed thrombosis in the right upper lobe pulmonary vein stump, which was considered to be the cause of the acute arterial occlusion. The patient underwent emergency thrombectomy following which his symptoms immediately improved. Herein, we report a rare case of pulmonary vein thrombosis occurring after a right upper lobectomy. Our findings may facilitate effective clinical decision-making.
INTRODUCTION
Pulmonary vein thrombosis (PVT) can be caused by lung transplantation, pneumonectomy, catheter ablation and trauma. Since the pulmonary vein directly flows into the systemic circulation without passing through the pulmonary circulation, PVT can cause serious thromboembolism (e.g. post-operative stroke). Recently, several reports of PVT occurring in the pulmonary vein stump (PVS) after lobectomy, particularly after left upper lobectomy, have attracted attention in the medical community [1, 2].
However, reports of PVT occurring in other PVSs have been extremely rare. Here, we report a case of PVT in the right superior PVS preceding and likely triggering acute arterial occlusion of the lower extremity following a right upper lobectomy.
CASE REPORT
A 78-year-old man was diagnosed with a 3.0-cm nodule in the right upper lung field on chest X-ray during a routine visit for the treatment of chronic atrial fibrillation (AF) and hypertension. Chest computed tomography (CT) showed a 3.0-cm-diameter nodule with a substantial component of pleural depression in the S3 segment of the right upper lobe (Fig. 1A).
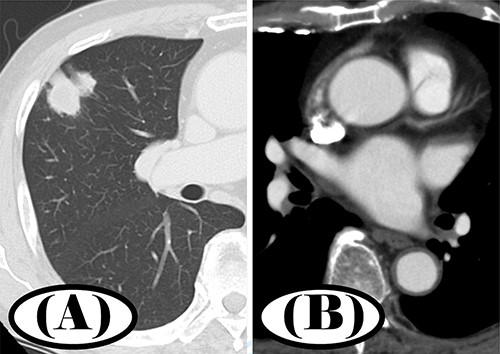
Preoperative chest CT; (A) a 3.0-cm nodule in S3 segment of the right upper lobe was found in pulmonary window setting; (B) contrast-enhanced CT showed no thrombus in the left atrium.
Fluorodeoxyglucose/positron emission tomography CT showed abnormal accumulation (maximum standardized uptake value [SUVmax] = 6.14) consistent with the lesion being located in the right upper lobe nodule. There were no other obvious abnormal findings. Contrast-enhanced CT revealed no obvious thrombus in the left atrium (Fig. 1B). Bronchoscopy was considered in the differential diagnosis. However, the patient had received warfarin for the treatment of chronic AF, and imaging findings were strongly suggestive of lung cancer.
We suggested a treatment course involving surgery, which the patient agreed to. The nodule was diagnosed as adenocarcinoma via intraoperative frozen sectioning following which we performed video-assisted thoracic surgery with a right upper lobectomy and mediastinal lymph node dissection. Warfarin was discontinued 5 days prior to the operation following which unfractionated heparin was administered intravenously (200 U/kg/day). Warfarin was resumed on post-operative day 2.
On post-operative day 7, the patient developed right lower extremity coldness as well as pain. Contrast-enhanced CT showed a thrombus in the right superior PVS (Fig. 2B). No vessels were depicted peripherally from the right popliteal artery (Fig. 2A). We diagnosed the patient with acute arterial occlusion of the right lower extremity. Emergency thrombectomy was performed and the patient’s symptoms quickly improved.
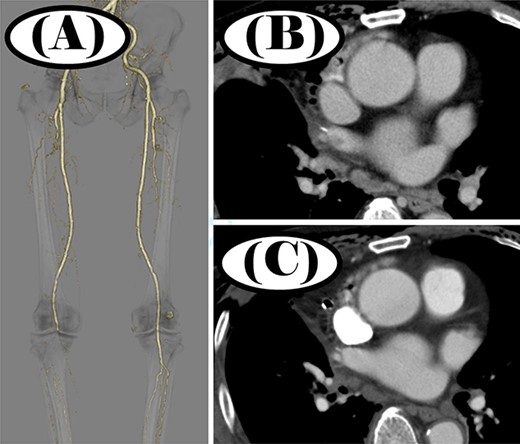
Contrast-enhanced CT before and after thrombectomy; (A) no peripheral vessels were depicted beyond the right popliteal artery before thrombectomy; (B) thrombus was seen in the right superior PVS before thrombectomy; (C) thrombus disappeared in the right superior PVS after thrombectomy.
After the thrombus was removed, the patient was started on oral clopidogrel (75 mg/day) and edoxaban (30 mg/day). One week later, a chest CT scan showed resolution of the thrombosis in the right superior pulmonary vein (Fig. 2C). He was discharged from the hospital 3 weeks after the surgery. Five years post-operatively, the patient has shown no signs of recurrence.
DISCUSSION
Recently, PVS as a potential complication of lobectomy has attracted increasing attention as a cause of PVT. In particular, the occurrence of PVT of the left upper PVS following left upper lobectomy has been reported in some case reports. Ohtaka et al. [2] reported that PVT occurred in 3.6% of patients who underwent lobectomy; all evaluated patients had undergone a left upper lung field resection. Moreover, these researchers reported an incidence of PVT of 13.5% (seven cases) following left upper lung field resection and reported that left upper lung field resection was a statistically significant risk factor for thrombosis formation.
A recent systematic review examined probable causes of PVT [1], which include mechanisms associated with stagnation of blood flow due to PVS as well PVT formation on the metal stapler used to dissect the pulmonary vein. Ohtaka et al. [3] noted that the cut end of the left superior pulmonary vein tended to be substantially longer than that of the other pulmonary veins (inferior left, superior right and inferior right). Blood stagnation at this long blind end may lead to thrombosis. In fact, Umehara et al. [4] analyzed changes in blood flow in the left atrium following lobectomy using 4D magnetic resonance imaging and confirmed that blood flow velocity decreased near the PVS.
With regard to preventing PVT, Nakano et al. [5] reported a method for dissecting the PV in the pericardial sac for shortening the PVS. However, cardiac tamponade has been reported as a serious complication of PV dissection in the pericardium. Moreover, vascularization of the pericardial sac is not a universal or common procedure within lobectomy. In terms of complications, this procedure likely cannot be considered the standard of care.
Although AF is a risk factor for thrombosis formation and paroxysmal AF is a well-known complication of lobectomy, heparin bridging is no longer used even when anticoagulants for AF are discontinued preoperatively. This is because many studies, including the BRIDGE trial [6, 7], have shown that heparin bridging is ineffective in preventing thrombosis and increases the risk of critical bleeding. As heparin bridging is not effective in perioperative thrombosis, it is unlikely to be effective as a prophylaxis against PVT. Thus, there is still no definitive effective and evidence-based approach for preventing PVT.
With the exception of our case, there have been few reports of PVT formation following non-left upper lobectomy. However, the number of such reports published has been relatively low to date [8, 9]. PVT is not a complication that occurs specifically after left upper lobectomy but is rather one that occurs when PVS is likely to be prolonged. Therefore, it may also occur in cases of non-left upper lobectomy, but currently, there are no effective preventive measures against PVT. Thus, we conclude that PVT should always be considered in patients at a high thrombotic risk even in cases other than that described in a previously published report of upper left PVT occurring after left upper lobectomy [2]. Herein, we present a rare report of lobectomy occurring in a location other than the left upper lobe. This novel finding is significant as PVT after lobectomy requires careful attention and meticulous follow-up. Our findings directly inform medical guidelines and effective clinical decision-making.
AUTHORS’ CONTRIBUTIONS
Takuya Ohashi and Mitsumasa Kawago were involved in the study design and wrote the manuscript as equal first authors. Yoshimitsu Hirai, Megumi Kiyoi, Miwako Miyasaka, Yumi Yata, Mari Kawaji, Aya Fusamoto, Hideto Iguchi, Hitomi Nakanishi and Yoshiharu Nishimura assisted in the writing of the manuscript. All authors critically revised the report, commented on drafts of the manuscript and approved the final report.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
We did not receive any external funding for this work.
ETHICS APPROVAL
The patient provided his written informed consent for these medical procedures as well as for the anonymized publication of his clinical findings and associated images.
REFERENCES
Author notes
T. Ohashi and M. Kawago are first authors
- warfarin
- thrombosis
- occlusion of artery
- computed tomography
- chronic atrial fibrillation
- adenocarcinoma
- amputation stumps
- intraoperative care
- pulmonary veins
- thrombectomy
- leg
- health care decision making
- unfractionated heparin
- right upper lung lobectomy
- perioperative period
- mediastinal lymph node dissection



