-
PDF
- Split View
-
Views
-
Cite
Cite
Tohru Ishimine, Takahiro Ishigami, Kohei Chida, Naoki Taniguchi, Toshiho Tengan, Hidemitsu Mototake, Aortic injury repair in a patient with situs inversus totalis and dextrocardia, Journal of Surgical Case Reports, Volume 2022, Issue 4, April 2022, rjac173, https://doi.org/10.1093/jscr/rjac173
Close - Share Icon Share
Abstract
Situs inversus totalis (SIT) with dextrocardia is a rare autosomal recessive disorder. We herein describe a blunt thoracic aortic injury (BTAI) in a patient with SIT and dextrocardia. An 18-year-old girl who was injured by a fall presented to our hospital. Computed tomography (CT) revealed a traumatic pseudoaneurysm at the aortic isthmus. Open aortic repair was performed through a right thoracotomy. No abnormal findings were observed on CT 1 year after the surgery. Open aortic repair of BTAI can be safely performed through a right thoracotomy in patients with SIT and dextrocardia.
INTRODUCTION
Situs inversus totalis (SIT) with dextrocardia is a very rare autosomal recessive disorder and is defined as a mirror image location of the thoracoabdominal organs. SIT has an incidence of 1/10 000 [1]. Although the coexistence of SIT with dextrocardia and blunt thoracic aortic injury (BTAI) is rare, some cases that were repaired via right thoracotomy or treated with thoracic endovascular aortic repair (TEVAR) have been reported [2, 3]. We herein describe a rare case of BTAI in a patient with SIT and dextrocardia, which was successfully subjected to open repair through a right thoracotomy.
CASE REPORT
An 18-year-old girl was injured by a fall from the fourth floor of a building because of a suicide attempt and was brought to our hospital. She had a history of depression and SIT with dextrocardia.
On examination, she was hypotensive (blood pressure, 60 mmHg; heart rate, 110 bpm) with a Glasgow Coma Scale score of 6 (E1V2M3), and she responded to fluid resuscitation. A chest radiograph showed a right-sided heart, indicating dextrocardia and widening of the upper mediastinum (Fig. 1).
Laboratory investigation results revealed anemia (hemoglobin level: 7.3 g/dl).
Contrast-enhanced computed tomography (CT) of the chest revealed SIT with dextrocardia and a saccular pseudoaneurysm at the aortic isthmus with a mediastinal hematoma (Figs 2a and b). Abdominal CT showed intraperitoneal fluid and free air, while CT of the head revealed multiple facial fractures. Radiographs of the limbs showed a right humeral fracture.
We immediately performed aortic repair and exploratory laparotomy. TEVAR was not indicated because of certain anatomical features of the aorta, namely a small diameter of 14 mm and steep angulation of the aortic arch.
During laparotomy, a gastric perforation measuring 2 cm at the pylorus was found and was closed in two layers.
Open aortic repair was performed through a right thoracotomy due to SIT with dextrocardia. A partial cardiopulmonary bypass was established through the right femoral artery and vein. We found a pseudoaneurysm involving 50% of the total aortic circumference at the aortic isthmus. Resection of the ruptured portion of the aorta and replacement with a 15-mm J Graft SHIELD NEO (Junken Medical Co, Ltd, Tokyo, Japan) was performed.
Surgeries for multiple facial fractures and right humeral fracture were performed in hospital days 13, 24 and 18. CT scan after surgery showed no abnormal findings at the part of graft replacement. The patient recovered well from the aortic and other operations and was discharged on hospital day 46. Although the graft and anastomosis demonstrated no abnormal findings on a CT scan obtained 1 year after the surgery, the patient died of non-aorta-related cause 2 years after surgery.
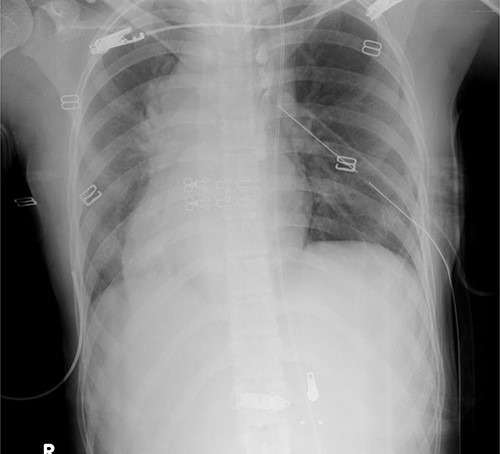
Chest radiograph showing a right-sided heart and widening of the upper mediastinum.
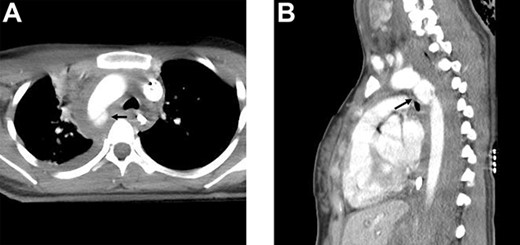
Contrast-enhanced CT scan showing a saccular pseudoaneurysm at the aortic isthmus (arrow) with a mediastinal hematoma; (a) transverse view and (b) lateral view.
DISCUSSION
BTAI accounts for ~1% of adult trauma admissions, with a high pre-hospital mortality rate ranging from 2 to 85%, according to autopsy results [4]. The BTAI is caused by the shearing force at the time of impact. The most common location of aortic tear is the aortic isthmus, where the mobile thoracic aorta is fixed by the ligamentum arteriosum, as was the case in our patient.
Traditionally, BTAI is repaired through a left thoracotomy, and the segment of the injured aorta is replaced using cardiopulmonary bypass. Recently, however, TEVAR has been preferred for treating BTAI because it is less invasive than open aortic repair.
Conversely, TEVAR is sometimes not indicated for the treatment of BTAI in adolescents because of the anatomical features of the aorta, such as a small diameter and steep angulation of the aortic arch [5], which is the case of our patient.
To the best of our knowledge, only two cases of SIT and dextrocardia coexisting with BTAI at the aortic isthmus have been reported [2, 3]. One patient was successfully treated with open repair, and the other was treated with TEVAR. In their case of SIT and dextrocardia coexisting with BTAI which was treated with open repair via right thoracotomy, Kulick et al. reported that, although care was taken to avoid injury to the recurrent nerve as in the case of a left open thoracotomy in patients with normal anatomy, the procedure could be performed without major problems [2]. In addition, their patient was operated using left heart bypass [2], while our patient was operated with partial cardiopulmonary bypass. We believe that partial cardiopulmonary bypass, which is established through the right femoral artery and vein, is simpler compared to left heart bypass, which is established with blood inflow obtained from a cannula placed in the morphologically left atrial appendage and arterial flow delivered through a cannula placed in the descending thoracic aorta, particularly in patients with SIT and dextrocardia.
In addition, in their case of SIT and dextrocardia coexisting with BTAI which was treated with TEVAR, Bilello et al. reported that the anomalous anatomy of their patient did not hinder TEVAR and that the preoperative planning differed only with regard to the placement of the arterial catheter in the left wrist instead of the right [3].
In conclusion, we present an extremely rare case of BTAI in a patient with SIT and dextrocardia. Open aortic repair of BTAI can be safely performed through right thoracotomy using partial cardiopulmonary bypass in patients with SIT and dextrocardia.
ACKNOWLEDGEMENTS
We would like to thank Editage (www.eitage.jp) for English language editing.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.



