-
PDF
- Split View
-
Views
-
Cite
Cite
Shamendra Anand Sahu, Jiten Kumar Mishra, Bikram Keshari Kar, R Manju, Moumita De, Adamantinoma of tibia: excision and reconstruction with free vascularized fibula flap: a case report and review of literature, Journal of Surgical Case Reports, Volume 2022, Issue 4, April 2022, rjac165, https://doi.org/10.1093/jscr/rjac165
Close - Share Icon Share
Abstract
Adamantinoma is a rare malignant tumour usually affecting the diaphysis of long bones. The tumour most commonly affects the tibia. Conventional management involves excision with a wide margin, reconstruction and sometimes amputation. Multiple options are available, but reconstruction depends upon the size of the bony defect and available resources. None has proved to be the favourable one. We have analysed the advantages and shortcomings of various methods used. In our case, a 33-year-old male patient presented with a large adamantinoma of the midtibial region of the left leg, which was managed with excision and reconstruction of long segment bony defect with free vascularized osteocutaneous fibula flap. There are osseointegration and hypertrophy of the vascularized bone with good functional gain in long term follow-up. Autologous bone reconstruction after adamantinoma excision with microvascular free fibula flap in large bone segment defects salvage the limb with satisfactory functional outcome.
INTRODUCTION
Adamantinoma is a rare low-grade malignant tumour of the long bones that can metastasize to distant locations, including lung, bone, lymph nodes, pericardium and liver [1]. It presents as a slow-growing, locally aggressive mass with or without pain in the affected limb in young adults. Adamantinoma commonly involves anterior cortex of tibial diaphysis [2]. Wide local excision of the tumour often results in a large bone gap necessitating reconstruction for limb salvage. We describe a case of adamantinoma tibia in which post tumour excision; 16-cm long bone defect reconstructed with osteocutaneous free fibula flap with good evidence of bone union and satisfactory functional outcome on long term follow-up.
CASE SUMMARY
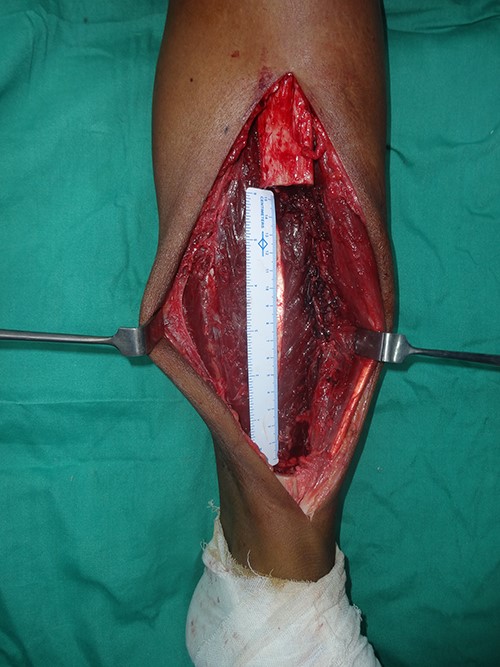
A 33-year-old gentleman presented with slow-growing swelling over the anteromedial aspect of the midshaft of left leg with dull aching pain for 2 years. The swelling was bony hard, 10 cm long and was fixed to the underlying tibia (Fig. 1). Anterior and posterior tibial arteries, sensory and motor functions of the affected legs were intact. Preoperative incisional biopsy report shows multiple epithelial-like cells in a background of fibrous dysplasia, suggestive of adamantinoma. X-ray suggested lytic expansile lesion with multiple septa and sclerotic margins involving the tibia’s diaphysis (Fig. 2). Computed tomography scan showed a cystic expansile lesion with a sclerotic margin obliterating the medullary cavity. Chest X-ray and abdominal ultrasound were normal. The bony defect in the tibia after wide excision of the tumour was 16 cm (Fig. 3) reconstructed with free fibula flap harvested from the opposite leg (Fig. 4). The bone flap was fixed to the tibia with a dynamic compression plate and bicortical screws (Fig. 4). The fibula flap pedicle, peroneal artery and one venae comitantes were anastomosed with the posterior tibial artery and great saphenous vein, respectively. Post-operatively, the flap, flap donor site and recipient’s leg wound healed without complications. Histopathological examination of excised lesion confirmed the diagnosis of classic adamantinoma with margins free of tumour (Fig. 5). After 1 year, there was radiological bone union, evidenced by uninterrupted bony borders between the fibula and recipient tibia bone, obscured osteotomy line at both the junctions and hypertrophy of the transferred fibula as per the bone union criteria by Hsu et al. [3]. The patient started partial weight-bearing in the operated limb after 6 months without any displacement or fracture of the vascularized bone graft. Three years post-surgery follow-up showed good evidence of bony integration and hypertrophy of the bone of the fibula flap, gradually accepting the shape of the tibia without any local recurrence or distant metastasis (Fig. 6). Patient is completely bearing weight on the affected lower limb with good function (Fig. 7).


Roentogram suggestive of a lytic expansible lesion in midtibial lesion.
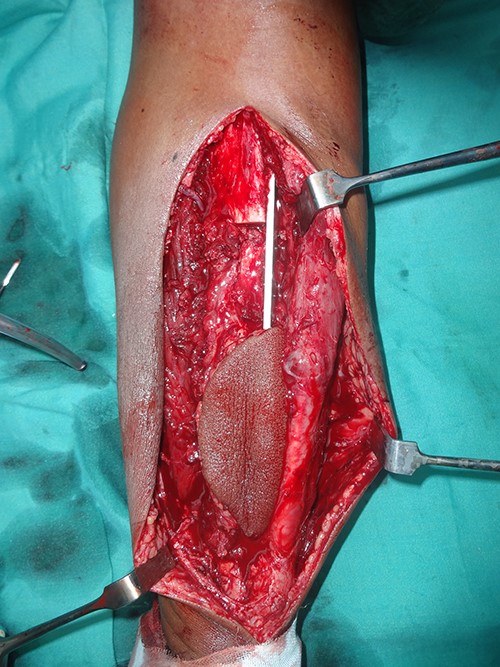
Intraoperative image with bone defect bridged with vascularized free fibula fixed with dynamic compression plate.



DISCUSSION
Despite these multiple modalities, the definitive diagnosis of adamantinoma is established only after histopathological examination. It is because of a close resemblance of osteofibrous dysplasia to adamantinoma in histological, radiological appearance and its location in the tibia. Osteofibrous dysplasia is a benign condition, whereas adamantinoma has a recurrence rate as high as 30–35% and mortality rate of 6–18% [4].
Standard treatment of adamantinoma tibia is wide excision of the tumour with reconstruction for limb salvage. Options used to reconstruct the bony defect include endoprosthesis, non-vascularized autograft, vascularized autograft or intramedullary implant. Radiotherapy or chemotherapy plays no role.
In a multicentre retrospective review of 70 cases of adamantinoma, 91% of patients had limb salvage procedure performed. Half of the patients received intercalary allograft reconstruction [4]. With allograft, the process of revascularization is slow. Autogenous non-vascularized grafts provide cells capable of new bone formation but are unsuitable for reconstructing defects >6–8 cm in length. In allograft and non-vascularized autograft, osteogenesis occurs by creeping substitution—a simultaneous process of resorption and deposition, which weakens the grafts and leads to delayed union, non-union, infection, fatigue fracture and resorption.
A vascularized fibula autograft provides a viable autogenous bone, which participates in the healing process. Healing takes place by the primary union. Its ability to undergo hypertrophy results in increased strength. It takes around 18 months for hypertrophy to occur. The strength of a vascularized fibular flap may be insufficient until hypertrophy occurs [5].
A.F. Mavrogenis et al. reported a case of adamantinoma of the tibia in which bony defect of 16 cm was reconstructed with an intramedullary implant [6]. The advantage of the prosthesis includes immediate stability, early ambulation and weight-bearing. Author’s follow-up was uneventful for 26 months, but implants are prone to mechanical failure, bone or implant fracture, infection, dislocation and loosening.
In other series of seven cases of adamantinoma, allograft reconstruction was done in five patients, and in two cases, endoprosthesis was used. One of the endoprostheses got infected. Two out of seven required amputation later [7].
In an interesting series of reconstructions in four cases of adamantinoma, reconstruction of mean tibial defect of 23 cm (17.5–26) and was done by distraction osteogenesis. It required multiple surgeries with long mean external fixation time of 8.5 months [8]. The significant complications reported were osteomyelitis, requirement of repeated debridement, use of negative pressure dressing, fracture of the regenerated segment and premature consolidation.
Tibialization of the fibula of the affected leg is also a technically feasible procedure for long segment tibial bony defect. The concern of using this technique in our case was: maximum hypertrophy of the fibula occurs in children, and it takes 2–4 years for optimum hypertrophy. Our patient is middle-aged, so the chance of stress fracture of only supporting bone of the affected limb is high, when the patient’s build is good.
CONCLUSION
Reconstruction depends on the size of the bone defect after excision. Small segment bone defects up to 6 cm can be reconstructed with implants, intercalary bone graft, avascular bone graft and Ilizarov technique. Reconstruction of >6–8 cm segment bone defect should be done with autologous fibula flap to avoid long-term complications of other reconstruction methods. Free fibula flap is a reliable option, especially in adults, for reconstruction with long-term satisfactory functional outcomes.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



