-
PDF
- Split View
-
Views
-
Cite
Cite
Tanya Odisho, Stephanie Joseph, Awni Shahait, Lydia Choi-Kim, Jessica McGee, Steve Kim, Potentially curative resection of an abdominal wall metastasis from pancreatic adenocarcinoma: a case report, Journal of Surgical Case Reports, Volume 2022, Issue 4, April 2022, rjac138, https://doi.org/10.1093/jscr/rjac138
Close - Share Icon Share
Abstract
Pancreatic cancer has a low survival rate even after ostensible complete resection, and treatment for recurrence is usually only palliative. However, rare solitary metastasis can occur and may be operable. In this report, we describe such a case and review the literature on metastasectomy for pancreatic adenocarcinoma. A 66-year-old female underwent Whipple procedure at our institution in 2014 for a pT3N0 pancreatic adenocarcinoma. A slowly growing umbilical mass was noted 6 years later with concomitant rise in her CA 19-9 levels. CT-guided biopsy of her abdominal wall mass confirmed a well-differentiated adenocarcinoma consistent with her primary pancreatic cancer. The patient underwent metastasectomy of the isolated abdominal wall mass, with negative margins. She received no further postoperative treatment. The patient remains disease and symptom-free over 18 months after resection of the metastasis. In highly selected cases of pancreatic adenocarcinoma, resection of solitary metastasis may be therapeutic.
INTRODUCTION
Despite advances in surgical care and adjuvant therapies, pancreatic cancer overall 5-year survival rate remains dismal [1]. Only 20% of patients are operable at the time of their diagnosis [2] and even after radical R0 surgical resection, recurrence rate remains as high as 80% and median survival is only 15–20 months [3].
Adjuvant chemotherapy with FOLFIRINOX [FOLinic acid, Fluorouracil (5FU), IRINotecan and OXaliplatin] regimen [4] or gemcitabine and nab-paclitaxel [5] has shown promise and is recommended after potentially curative resection, whereas adjuvant radiation has fallen out of favor [6]. In any case, postoperative prognosis remains guarded with median survival duration usually <2 years [7], regardless of the type of relapse. Median survival after local recurrence is only slightly better than after hepatic metastases (5–7 months vs. 3 months) [3]. For these reasons, the goal of treatment for pancreatic cancer relapse is generally palliative. Rarely, potentially curative surgery may be an option for solitary metastasis in selected subgroups of patients [8, 9]. This report describes a patient with an initial pT3N0 pancreatic adenocarcinoma who underwent resection of an isolated abdominal wall metastasis 6 years later. We review the treatment options for oligometastatic pancreatic cancer and the indications and outcomes for metastasectomy.
CASE REPORT
The patient presented with abdominal pain without jaundice or weight loss in 2014. Computerized tomography (CT) imaging showed a pancreatic head mass with no distant metastasis. Laboratory values were significant for elevated carbohydrate antigen (CA) 19-9 of 257 units/ml (normal <36 units/ml). Biopsy pathology showed multifocal pancreatic intraepithelial neoplasia-2 (PanIN-2) in a background of atrophic pancreatic parenchyma and fibrosis. No invasive disease was noted.
The patient underwent pancreaticoduodenectomy in July 2014. Pathology demonstrated a 6.4 × 4.0 × 3.9 cm moderately differentiated adenocarcinoma with 14 negative lymph nodes and no evidence of lymphovascular or perineural invasion. The pancreatic transection margin was negative for invasive disease but positive for grade 2/3 PIN (pancreatic intraepithelial neoplasia). She was staged as pT3 N0 M0 (Stage IIA). The patient underwent adjuvant chemotherapy with gemcitabine from January to June of 2015. She was then treated with capecitabine and radiation therapy.
Although on surveillance, she was noted to have slow rise in CA 19-9 (58.4 units/ml) in July 2018, but she remained asymptomatic and imaging at that time showed no evidence of recurrence. In May of 2020, her CA 19-9 had risen to 477 units/ml (Fig. 1), and CT scan at that point demonstrated an umbilical mass measuring 3.8 × 2.1 cm, which in retrospect had been slowly growing over the past 2 years. Biopsy of the mass confirmed well-differentiated adenocarcinoma. Subsequent positron emission tomography (PET) scan demonstrated no other sites of recurrent disease (Fig. 2). After discussion in the multidisciplinary tumor board, she was initially offered surgery. She refused and wished to proceed with percutaneous ablation instead. However, this was not possible due to proximity of the mass to bowel. She therefore agreed to proceed with resection and this was done in July 2020. At laparotomy, the tumor was noted to be growing within the fascia and muscle of the anterior abdominal wall, and en bloc resection was completed, with subsequent repair of the fascial defect with mesh (Fig. 3). Pathology confirmed metastatic adenocarcinoma with margins of resection free of tumor.
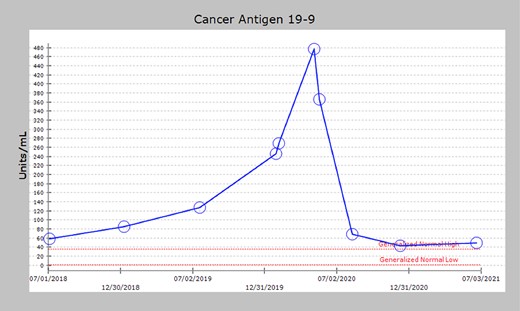
Serum CA 19-9 levels after primary pancreatic resection showing gradual elevation in CA 19-9 (58.4 units/ml) beginning in July 2018. In May of 2020, CA 19-9 had risen to 477 units/ml, corresponding to CT scan findings consistent with an umbilical mass. After recurrence resection, the initially elevated CA 19-9 levels significantly decreased (49 units/ml).
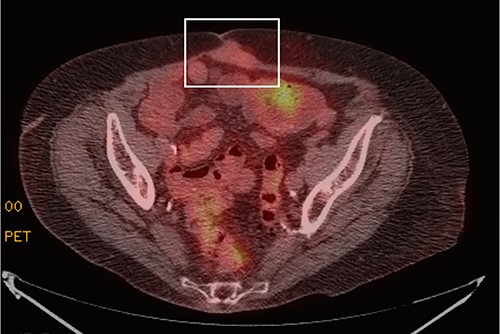
PET scan showing a focal area of mildly FDG avid soft tissue mass within the rectus musculature deep to umbilicus abutting the midline abdominal wall (white box), measuring 3.9 × 2.0 cm, a finding suggestive of a solitary site of metastatic disease. There was no evidence of other sites of metastasis.
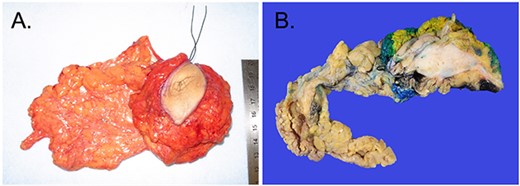
(A) Excised umbilical mass grossly measuring |$\sim$|8 × 6 × 3 cm in size. (B) Cross-section of the mass which appears as a gray-white, fibrotic and rubbery tumor, directly underlying the skin surface with a portion of omentum adherent to the posterior surface with puckering of the surface. There is no evidence of bowel adherence to the tumor.
The patient received no further systemic treatment after resection and was placed back on surveillance. Most recent repeat CT imaging 16 months after metastasectomy showed no evidence of recurrence or new sites of metastatic disease. Her most recent CA 19-9 is 49 units/ml (Fig. 1) and she remains clinically well and without symptoms.
DISCUSSION
Recurrence after resection of pancreatic adenocarcinoma is almost always associated with a poor prognosis [10]. Of note, our patient had an invasive intraductal papillary mucinous neoplasm (IPMN) with PIN grade 2 at the pancreatic transection margin; however, this did not result in local recurrence at over 7 years of follow-up. This is in accordance with data suggesting that noninvasive IPMN (PIN 1 or 2) at the pancreatic transection margin is not associated with locally recurrent disease [11]. When isolated local recurrence does occur, it is usually technically unresectable, whereas distant recurrences are usually diffuse and multifocal and hence, also inoperable. Solitary metastasis is rare but resection may be associated with survival benefit in selected cases [8, 9]. Although obviously subject to selection bias, a number of nonrandomized studies have shown that the survival of patients with isolated recurrence was longer after surgical versus non-surgical treatment [9, 12, 13]. In a study of 48 patients undergoing resection of recurrent pancreatic cancer, Kim et al [13] found that poorer survival was associated with elevated CA 19-9 level, disease-free interval from primary tumor resection of <10 months, large tumor size (> 3 cm), poorly differentiated tumors and node-positivity of the original primary tumor. These results are similar to data regarding prognostic factors associated with survival after hepatic metastasectomy for colorectal cancer, procedures that are much more commonly done. In a study of over 1000 such patients, Fong et al. [14] demonstrated that positive margin, extrahepatic disease, node-positive primary, disease-free interval < 12 months, increasing number of hepatic tumors, largest hepatic tumor >5 cm and carcinoembryonic antigen level > 200 ng/ml were all negative prognostic factors for survival. In our case, the patient had negative prognostic factors of high CA 19-9 level (477 u/ml) and tumor size of 4 cm; however, the original tumor was node-negative, and there was a long disease-free interval (6 years post pancreatectomy), and these may have contributed to the patient’s persistent remission at 18 months.
In conclusion, carefully selected patients with solitary site of pancreatic cancer recurrence may be amenable for resection. Paramount among the factors associated with favorable survival outcomes would be excellent performance status and a long disease-free interval. Options of resection +/− aggressive chemotherapy protocols such as FOLFIRINOX [4], as well as other nonsurgical local therapies like image-guided ablation or stereotactic body radiation therapy [15] should be discussed in a multidisciplinary setting to optimize survival for patients with this aggressive malignancy.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.
CONSENT FOR PUBLICATION
Written informed consent was obtained from the patient for the presentation of her case along with the associated medical imaging.



