-
PDF
- Split View
-
Views
-
Cite
Cite
Tristan Tham, Matthew I Saleem, McKenna Hawthorne, Alexandros Georgolios, Practicing functional nasal surgery in the non-urban setting: experience from a single center, Journal of Surgical Case Reports, Volume 2022, Issue 4, April 2022, rjac119, https://doi.org/10.1093/jscr/rjac119
Close - Share Icon Share
Abstract
Nasal airway obstruction is a prevalent chief complaint in the contemporary facial plastic surgery practice. Studies report an asymmetric distribution of plastic surgeons across the United States with a disproportionately high concentration of surgeons practicing in urban areas. The lack of elective specialist care creates unique challenges for these patients who may need to travel and dedicate time to reach a nasal surgery expert. We conducted a retrospective chart review to report our experience from practicing functional nasal surgery in such a non-urban setting in the United States. A total of 103 patients underwent functional nasal surgery (FNS) between May 2015 and August 2021 including septoplasty, inferior turbinate reduction, septorhinoplasty and nasal valve procedures. We present the epidemiological characteristics, surgical techniques used and postoperative complications and illuminate the unique characteristics of practicing FNS in the non-urban setting.
INTRODUCTION
Nasal airway obstruction (NAO) is a prevalent chief complaint in the contemporary facial plastic surgery practice. Studies report an asymmetric distribution of plastic surgeons across the United States: a disproportionately high concentration of surgeons practice in urban areas [1]. Li et al. [2] identified urban location as an independent risk factor for subsequent septorhinoplasty following initial nasal bone fracture. This reflects the lack of elective specialist care access for these patients who may need to travel and dedicate time to reach a nasal surgery expert.
CASE SERIES / METHODS
We conducted a retrospective chart review with the approval of the Ethics Committee of our institution. A total of 103 patients underwent functional nasal surgery (FNS) between May 2015 and August 2021 including septoplasty, inferior turbinate reduction, septorhinoplasty and nasal valve procedures (CPT codes 30 520, 30 802, 30 420, 30 465). All patients had failed previous management with at least 6 weeks of intranasal steroids. All surgical procedures were performed by the lead author.
CASE SERIES/RESULTS
Sixty-four patients self-identified as males (62.1%) and 39 as females (37.9%). Ages ranged from 16 to 78 years (mean 38.05). Fifty-two patients (50.5%) reported a history of nasal trauma. Seven patients (6.8%) had previous FNS (reported septoplasty and/or inferior turbinate reduction) and 94 (91.2%) reported no previous nasal procedures. Forty-three patients (41.7%) were never smokers, 42 patients (40.8%) were active smokers and 18 patients (17.5%) reported past smoking history. Eighteen patients (17.5%) had a diagnosis of diabetes at the time of surgery (Table 1).
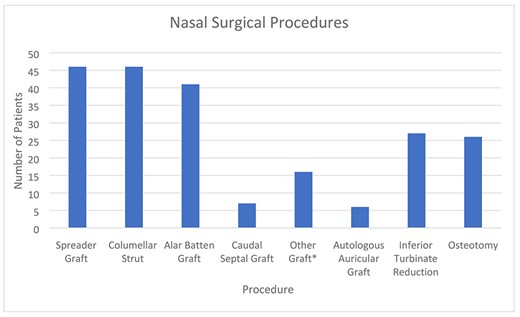
Spreader grafts were used at 46 patients (44.7%), columellar struts at 46 patients (44.7%), alar batten grafts at 41 patients (39.8%), caudal septal grafts at 7 patients (6.8%), other grafts reported at 16 patients (15.5%), autologous auricular graft harvested at 6 patients (5.8%) and inferior turbinate reduction performed at 27 (26.2%). Osteotomies were required in 26 patients (25.2%). Caudal septal grafts were reported when the L-strut required replacement (anterior septal reconstruction/extracorporeal septoplasty). Other grafts included on-lay grafts, alar rim grafts and lateral crura strut grafts (Fig. 1).
| Characteristic . | Percentage . |
|---|---|
| Gender | |
| Male | 62.1 |
| Female | 37.9 |
| Surgical history | |
| Previous nasal trauma | 50.5 |
| Previous nasal surgery | 6.8 |
| No previous nasal surgery | 91.2 |
| Smoking history | |
| Never smoker | 41.7 |
| Past smoking history | 17.5 |
| Active smoker | 40.8 |
| Type 2 diabetes mellitus | 17.5 |
| Characteristic . | Percentage . |
|---|---|
| Gender | |
| Male | 62.1 |
| Female | 37.9 |
| Surgical history | |
| Previous nasal trauma | 50.5 |
| Previous nasal surgery | 6.8 |
| No previous nasal surgery | 91.2 |
| Smoking history | |
| Never smoker | 41.7 |
| Past smoking history | 17.5 |
| Active smoker | 40.8 |
| Type 2 diabetes mellitus | 17.5 |
| Characteristic . | Percentage . |
|---|---|
| Gender | |
| Male | 62.1 |
| Female | 37.9 |
| Surgical history | |
| Previous nasal trauma | 50.5 |
| Previous nasal surgery | 6.8 |
| No previous nasal surgery | 91.2 |
| Smoking history | |
| Never smoker | 41.7 |
| Past smoking history | 17.5 |
| Active smoker | 40.8 |
| Type 2 diabetes mellitus | 17.5 |
| Characteristic . | Percentage . |
|---|---|
| Gender | |
| Male | 62.1 |
| Female | 37.9 |
| Surgical history | |
| Previous nasal trauma | 50.5 |
| Previous nasal surgery | 6.8 |
| No previous nasal surgery | 91.2 |
| Smoking history | |
| Never smoker | 41.7 |
| Past smoking history | 17.5 |
| Active smoker | 40.8 |
| Type 2 diabetes mellitus | 17.5 |
Six postoperative complications (5.8%) were reported in four patients (3.9%). These included three posterior septal perforations, two cases of severe postoperative bleeding, one infection and one case of minimal persistent bleeding that required medical attention. All septal perforations were asymptomatic. The infection manifested with minimal drainage in the mid-columellar incision and resolved with a course of antibiotics. The minimal postoperative bleeding occurred in a patient who was managed only with inferior turbinate reduction.
DISCUSSION
Limited by the relatively small size, we report our experience from FNS in a non-urban center. About 50.4% of our patients reported history of nasal fracture, making post-traumatic FNS a major part of our practice; 40.7% of our patients were active smokers, and 17.4% reported past smoking history, numbers unparalleled to any rhinoplasty studies. A tertiary center study reported 11% active smokers and 30% previous smokers among patients undergoing nasoseptal surgery [3]. This difference may reflect higher incidence of tobacco use in our area compared with the national incidence of smoking in adults (14% in 2019) [4]. Our complication rate was 5.8%, similar to previously reviewed (bleeding-related complications 0.2–6.7%, infection 0–4%, septal perforations 0–2.9%) [5]. Two patients had a complicated postoperative course including both postoperative bleeding and subsequent septal perforations. Only 6.7% were revision cases, perhaps indicating the hardship in reaching expert care.
CONCLUSION
Our results illuminate the unique characteristics of practicing FNS in the non-urban setting. Solid clinical expertise is required to manage these challenging patients.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



