-
PDF
- Split View
-
Views
-
Cite
Cite
Teagan Fink, Siddhartha Deb, David Clouston, Chantel Thornton, Anannya Chakrabarti, Novel case of a granular cell tumour mimicking breast malignancy and a metachronous axillary skin lesion, Journal of Surgical Case Reports, Volume 2022, Issue 3, March 2022, rjac140, https://doi.org/10.1093/jscr/rjac140
Close - Share Icon Share
Abstract
A 51-year-old woman presented with an asymptomatic screen-detected lesion of the right breast. The core biopsy showed a granular cell tumour (GCT). Twelve months later the woman presented with an incidental finding of a skin lesion in the left axillary fold during her annual breast surveillance review. Histopathology confirmed a second metachronous GCT. GCTs are an uncommon benign tumour of Schwann cell origin that can infrequently be multifocal. Due to the non-specific clinical presentation and radiological features, the gold standard of diagnosis relies on histologic assessment. We describe a novel case of metachronous GCT within the breast tissue mimicking a breast malignancy as a mammography screen-detected lesion, followed by a second GCT mimicking a scar lesion on the contralateral axillary fold.
INTRODUCTION
Granular cell tumours (GCT) are an uncommon low-grade tumour of Schwann cell origin, found in multiple locations including skin, soft tissue; and oral, gastrointestinal tract and respiratory tract mucosal surfaces [1–3]. Approximately 8% of GCTs are found in the stromal or skin tissue of breast, and 14% of all cases may be multifocal. GCTs of the axilla are extremely rare [4]. Less than 2% of GCTs show malignant behaviour [1, 5, 6]. We present figures from the first published case of metachronous GCTs of the right breast and contralateral axillary fold, discuss the pathological findings of GCT and summarize the salient take home messages for surgeons who may encounter multifocal lesions.
CASE REPORT
A 51-year-old woman presented with a screen-detected non-palpable painless lesion in the right upper inner quadrant of the breast. She had no overlying skin changes or nipple symptoms. Her risk factors for malignancy included smoking and age, with no family history of breast cancer. Mammogram showed a complex mass. Ultrasound demonstrated a 9 mm complex cyst 2 o’clock and 3 cm from the nipple. Core biopsy found a GCT with sheets of large cells, with granular cytoplasm and S100 immunopositivity. The patient underwent a hookwire guided diagnostic excision of the right breast lesion. Histopathology confirmed a GCT, with no atypical high-grade features, excised with clear margins.
Twelve months later, the patient presented with an incidental finding of a 5 cm firm, tethered, painless skin lesion in the left lateral axillary fold during her annual breast surveillance review (Fig. 1a). The patient was uncertain as to the timeline of this lesion although reported no new breast or nipple symptoms. Her surveillance mammogram and ultrasound detected no abnormality. Under local anaesthetic, the axillary lesion was excised en bloc and directly closed. The histology showed a GCT of 30 mm (Fig. 1b and c), with no evidence of necrosis, with no heightened nuclear pleomorphism and with one mitosis per 10 high power fields. The lesion was re-excised with clear margins.
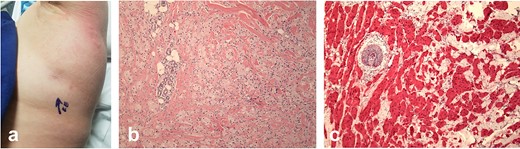
Tethered area of skin in the left axillary fold (a). Histology of the axillary fold GCT (H&E ×200)(b), with S100 immunohistochemical staining (c).
DISCUSSION
GCTs typically present as a painless solitary nodule in the skin and subcutaneous tissues and can mimic malignant breast disease. Lesions can present as a mixed density, irregular and spiculated mass on mammogram. Ultrasonographic findings include a poorly circumscribed, spiculated hetero-echoic mass with posterior acoustic shadowing and lying nonparallel to the chest wall [7]. Due to the non-specific clinical presentation and radiological features, the gold standard of diagnosis relies on histologic assessment. GCTs are typically composed of sheets and nests of large round and polygonal cells, containing small nuclei, profuse eosinophilic cytoplasm, with positive staining for S100. Caution when interpreting histopathology reports for these tumours is required, as perineural and vascular invasion is common in benign GCTs [2].
Although most cases are of single lesions, the approach to multifocal GCTs is challenging, as the limited data suggests up to 12%–13% of cases may be of malignant disease which shows poor mortality (40% at 5 years) [1]. Fanburg-Smith et al. published six histological criteria for GCTs to delineate malignant from benign cases—spindling cells, increased nuclear:cytoplasmic ratio; vesicular nuclei with large nucleoli; pleomorphic nuclei; necrosis and increased mitotic activity [1]. This was found in a series of 46 multicentric tumours, of which only six were clinically benign. Malignant behaviour was also associated with female propensity, a median age of 40–47 years old and a median tumour size of 4 cm–5.5 cm in malignant GCTs [1].
However, not all lesions with malignant histologic features have been shown to progress and some lesions with ascribed benign features have shown malignant behaviour [3, 8]. Although consensus recommendations are not currently present, authors of larger series have suggested all patients with GCTs should be monitored closely. Surveillance imaging and surgical excision of all lesions with clear margins is the main stay of treatment [2, 3, 6, 8, 9]. The efficacy of both radiotherapy and chemotherapeutic treatment is unknown with no recommendations present.
CONCLUSION
We present a case of a 51-year-old lady presenting with multifocal granular cell tumour, an uncommon soft tissue tumour usually of low malignant potential but with high mortality when malignant behaviour is present. To our knowledge this is the first case of metachronous tumours of the breast and axillary fold. When histomorphological markers present are suggestive of malignant behaviour, close clinical and radiological surveillance is recommended, in addition to surgical excision of lesions with clear margins. Rarely, multifocal lesions may be associated with conditions such as Noonan syndrome and LEOPARD syndrome [10, 11]. We have described the first case published in the literature of metachronous GCT within the breast tissue and axillary skin.



