-
PDF
- Split View
-
Views
-
Cite
Cite
Takeshi Kitazawa, Motomu Suito, Hiroyuki Nagaya, Blepharoptosis as a complication of percutaneous ethanol injection of thyroid cyst, Journal of Surgical Case Reports, Volume 2022, Issue 3, March 2022, rjac091, https://doi.org/10.1093/jscr/rjac091
Close - Share Icon Share
Abstract
Complications of percutaneous ethanol injection (PEI) for thyroid cyst are rare. Almost all complications reported have been transient, including Horner’s syndrome. We provide herein the first description of persistent blepharoptosis subsequent to PEI, necessitating surgical correction. A 54-year-old woman presented to our hospital with left blepharoptosis that had occurred the day after PEI for a thyroid cyst. She showed 2 mm of blepharoptosis and 1 mm of miosis in the left eye compared to the right eye. Magnetic resonance imaging of the brain demonstrated no abnormalities, and computed tomography detected no lesions in the neck or chest other than the already known cyst. Instillation of phenylephrine eye drops allowed elevation of the left upper eyelid. Considering these findings, we diagnosed the blepharoptosis as part of Horner’s syndrome. The ptosis was corrected by levator aponeurosis advancement. No recurrence has been observed as of 9 months postoperatively.
INTRODUCTION
Percutaneous ethanol injection (PEI) was originally used to treat neoplastic lesions in the liver and is also applied for thyroid cysts [1]. Based on its effectiveness and safety, current guidelines suggest PEI as a first-line treatment for cystic lesions of the thyroid [2, 3]. Relatively few adverse events have been reported in association with PEI, all of which appear to have been transient. We report herein a case of unilateral blepharoptosis due to Horner’s syndrome subsequent to PEI, in which the ptosis required surgical correction.
CASE PRESENTATION
A 54-year-old woman presented to our hospital with unilateral blepharoptosis. She showed 2 mm of blepharoptosis and 1 mm of miosis in the left eye compared to the right eye, but no enophthalmos, anhidrosis or vascular dilatation. Ocular movements were intact bilaterally and she did not complain of diplopia. Computed tomography detected no lesion in the neck or chest other than the already known thyroid cyst (Fig. 1). Magnetic resonance imaging of the brain revealed no abnormalities.
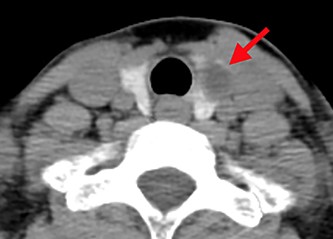
Computed tomography shows a low-density area in the left lobe of the thyroid (red arrow).
She had first noticed left blepharoptosis the day after undergoing PEI for a thyroid cyst, and the ptosis had not improved for 6 weeks.
According to the endocrinologists who treated the patient, she had complained of a noticeable neck mass, but no other symptoms related to thyroid disease. Thyroid ultrasonography on the first presentation to them had shown a cyst in the left lobe measuring 40 × 26 × 52 mm. Thyroid function tests had shown that thyroid-stimulating hormone, free T3, free T4, thyroglobulin antibody and thyroid peroxidase antibody were all within normal limits. Fine needle aspiration cytology of the cyst had shown no malignant cells. Aspiration of the cyst had been performed five times during 3 years of follow-up, but no marked or lasting shrinkage had been obtained.
PEI was performed under sonographic guidance using an 18-gauge needle. Eighteen milliliters of fluid was aspirated and 1 ml of 95% ethanol was injected into the cyst. The injected ethanol was left in place briefly, then aspirated. Another 1 ml of ethanol was then injected and left in the cyst without re-aspiration.
During three more months of observation by our department, left ptosis and miosis remained unchanged. Instillation of phenylephrine drops in the left eye enlarged the left palpebral fissure height (PFH) while simultaneously decreasing the PFH of the right eye (Fig. 2). We diagnosed left blepharoptosis as a symptom of Horner’s syndrome following PEI, accompanied by contralateral involutional ptosis masked by compensatory excessive contraction of the levator palpebrae superioris (LPS) muscle. Bilateral ptosis surgery was therefore planned.
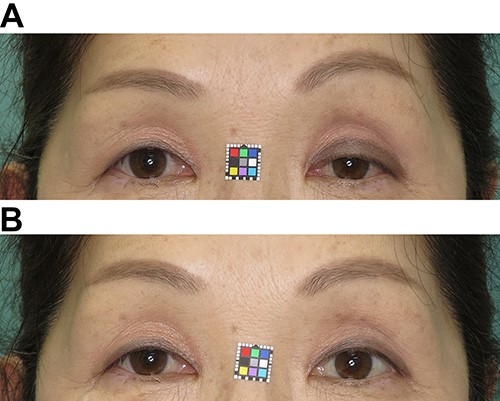
Photographs 5 months after PEI. (A) Left blepharoptosis with brow elevation caused by compensatory contraction of the frontalis muscle is observed. (B) Instillation of phenylephrine drops in the left eye improved ptosis and lowered the eyebrow that had been raised by frontalis muscle contraction.
The operation involved LPS advancement with excision of redundant eyelid skin under local anesthesia. First, skin and orbicularis oculi were excised, and the orbital septum was incised horizontally to open the LPS aponeurosis behind the preaponeurotic fat pad. Next, the aponeurosis was slightly pulled out and secured to the tarsus with two stiches of 6/0 polypropylene (Fig. 3).
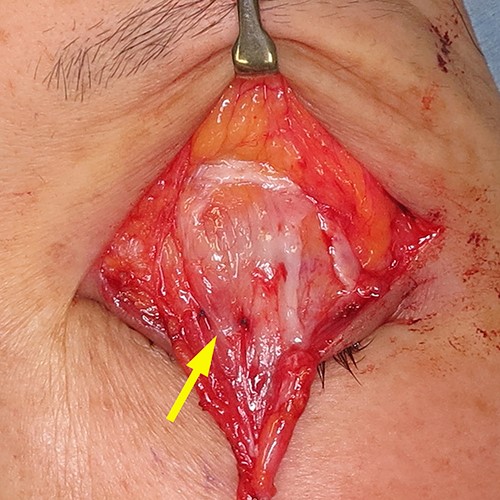
Surgical technique. The aponeurosis was slightly pulled out and secured to the tarsus with two stiches of 6/0 polypropylene (yellow arrow).
As of 9 months postoperatively, although left miosis has remained unchanged, blepharoptosis has remained improved without recurrence (Fig. 4).

DISCUSSION
The injection of 95–99% ethanol into a cyst cavity induces thrombosis of small vessels and coagulative necrosis surrounded by interstitial edema and granulomatous inflammation, followed by fibrosis, shrinkage and a reduction in the volume of the lesion [4]. PEI for thyroid cysts, as an alternative to surgery, is widely considered safe and effective. The recent literature has reported success rates for this procedure of 64–95%, with success defined as almost complete disappearance of the cyst or a marked reduction in volume (>50%) associated with symptom control [5].
The most frequent complication is mild transient pain at the site of injection. Halenka et al. [6] reported local pain after injection in 58 of 200 patients (29%). Kim et al. [7] noted mild-to-moderate pain in 19 of 60 patients (32%). In the largest cohort study, by Lee and Ahn [8], 32 of the 432 patients (7.9%) reported transient local pain.
However, severe complications appear rare. Of the 432 patients investigated by Lee and Ahn [8], only 3 patients (0.7%) experienced temporary unilateral vocal cord paralysis, with full recovery within 2 months in all cases [8]. Raggiunti et al. [1] reported two patients (1.8%) who suffered from transient dysphonia in a study of 110 patients. Dysphonia or vocal cord paralysis occurs when the recurrent nerve is damaged by ethanol that has leaked from the cyst [1].
In the present case, the cervical sympathetic chain might have been damaged by leaked ethanol. The cervical sympathetic chain is typically located posterolateral to the common carotid artery, but 12% of specimens show a middle cervical sympathetic ganglion located between the thyroid gland and common carotid artery [9]. Whether the present case corresponded to the latter type remains uncertain, but we can infer that a cervical sympathetic chain located near the thyroid is vulnerable to damage in therapeutic interventions.
While less than 30 cases of Horner’s syndrome following thyroid surgery have been reported in the literature [10, 11], only two other cases of Horner’s syndrome after PEI appear to have been reported [12, 13]. Symptoms in both of the previously reported cases resolved spontaneously. The present case may provide the first description of a persistent complication of PEI needing surgical repair.
The validity of advancing the LPS with Müller’s muscle kept intact as a treatment for the ptosis due to Horner’s syndrome was demonstrated by Matsuo [14, 15]. He successfully treated 11 patients of Horner’s syndrome by aponeurotic advancement procedures. He hypothesized that the mechanoreceptors for eye-opening presumably exist in the proximal part of Müller’s muscle, which is a serial kind of muscle spindle of the LPS muscle, and contraction of Müller’s muscle, which stretches the mechanoreceptor, evokes involuntary contraction of the LPS muscle. Paralyzed Müller’s muscle desensitizes the mechanoreceptor, but aponeurotic advancement procedures, which approximate and secure the proximal part of Müller’s muscle to the tarsus, resensitize the mechanoreceptors.
In conclusion, irreversible adverse effects are extremely rare but can be caused by PEI. However, persistent blepharoptosis due to Horner’s syndrome is treatable.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



