-
PDF
- Split View
-
Views
-
Cite
Cite
M T Sampiev, N V Zagorodniy, I S Lysenko, I P Dubinin, K H M CHemurzieva, Two-stage treatment of idiopathic scoliosis using the LSZ growing system with a 10-year follow-up: a case report, Journal of Surgical Case Reports, Volume 2022, Issue 3, March 2022, rjac087, https://doi.org/10.1093/jscr/rjac087
Close - Share Icon Share
Abstract
A clinical case of an 11-year-old patient with idiopathic scoliosis treatment using the LSZ growing system. The main thoracic curve was 88°, with a lumbar curve of 52°. The patient was at Risser stage 3. At the first stage, posterior correction and instrumentation (T1-L5) of the deformity using the LSZ growing system were performed. Residual deformity of the spine was 15°. At a follow-up, the spine grew by 5 cm. As the second stage of surgical treatment, this system was removed and replaced with selective instrumentation at T4-T12. The patient was followed up for 10 years. On the control radiographs of the spine in the standing position in 2021, adequate correction is preserved. That described technique allowed to ultimately perform selective definitive instrumentation, preserving near full range of movement in the lumbar spine. Further studies are needed to determine the effectiveness of the described approach.
INTRODUCTION
Treatment of scoliosis in patients who have not reached skeletal maturity is challenging because this population is heterogeneous, the patients often have concomitant somatic diseases and their treatment requires several stages of correction. Patients with early onset deformities often present with impaired lung function due to high risk of spinal deformity progression and reduced chest volume during the critical period of lung development [1].
The goals of surgical treatment of scoliosis in patients who have not reached skeletal maturity are to preserve the growth potential of the spine and to correct and control spinal deformity to promote normal development of the lungs and spine [2].
The LSZ growing system, which includes uniquely designed hooks that are fixed to the lamina and two rectangular (on cross-section) plates that do not interfere with free movement of the hooks relative to the plates, has been developed and put into use at our center (Fig. 1).
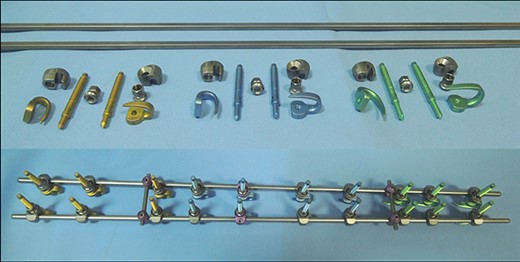
Photos of the LSZ growing system. The upper photo demonstrates a disassembled system. The bottom photo demonstrates an assembled system.
The patients and their families were informed that data from the research would be submitted for publication, and gave their consent.
CASE REPORT
The patient was referred to our center in 2006 at the age of 11 with a right-sided thoracic curve and a left-sided lumbar curve. The patient’s sitting height was 71 cm and weight was 45 kg. There were no neurological symptoms. Diagnosis at presentation: adolescent thoracic idiopathic scoliosis with deformity angle of 43° (Fig. 2a). The patient’s parents refused surgical treatment in favor of bracing. The treatment was ineffective and deformity progressed within a year. At a follow-up examination at the age of 12, the main thoracic curve deformity angle progressed to 88°, with a lumbar curve of 52°. At that time, the patient was a Risser 2 (Fig. 2b).
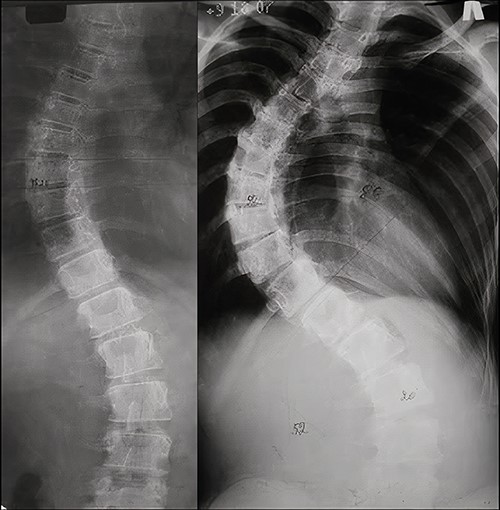
AP X-rays of the patient’s spine. (a) At 11 years old in standing position. A 43° main thoracic curve is visualized. (b) At a 1-year follow-up (12 years old, standing position). A main thoracic curve of 88° and a lumbar curve of 52° are visualized.
Due to rapid deformity progression and incomplete skeletal maturity, 2-stage surgical treatment was elected. At the first stage, posterior correction and T1-L5 instrumentation using the LSZ growing system were performed. The intervention lasted 125 min. Blood loss amounted to 240 ml. The postoperative period was uneventful. Radiographs on postoperative Day 5 demonstrated 83% correction (Fig. 3a). The immediate postoperative sitting height was 75 cm.
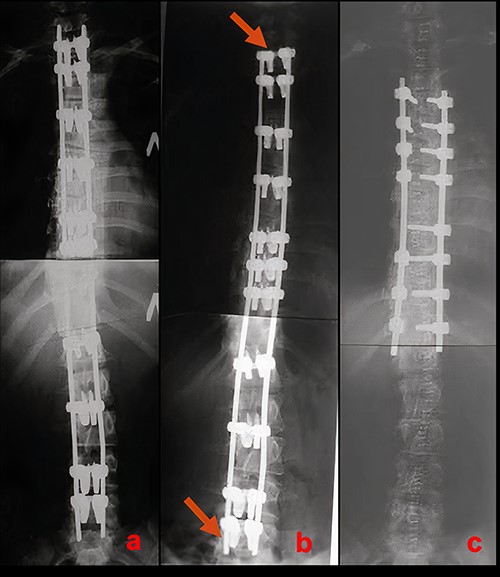
Radiographic results of surgical treatment. (a) AP X-rays of the patient’s spine in standing position after the 1st stage of surgical treatment on the 5th day after surgery. Residual deformity of the spine was 15°. (b) AP X-ray of the patient’s spine in a standing position 4 years after surgery. Growth of the spine and the associated shortening of the free upper and lower ends of the plates can be observed (red arrows). (c) AP X-ray of the patient’s spine after the 2nd stage of surgical treatment. The angle of residual deformity is < 5°.
At a 4-year follow-up at the age of 16, the spine grew by 5 cm. The patient’s sitting height was 80 cm. Shortening of the free ends of the plates at the upper and lower ends of instrumentation, associated with the continued growth of the spine could be clearly visualized (Fig. 3b).
As the second stage of surgical treatment, the LSZ system was removed and definitive T4-T12 instrumentation was performed. The duration of the surgery was 203 min. Blood loss amounted to 450 ml. Postoperative radiographs demonstrated 94% deformity correction (compared with deformity before index surgery) (Fig. 3c). The patient was mobilized on Day 2.
On 10-year follow-up, radiographs of the spine in the standing position in 2021 adequate correction are preserved with a slight asymptomatic increase of lumbar deformity (Figs 4 and 5).

X-rays of the patient’s spine at a 10-year follow-up. (a) AP X-ray of the spine in standing position. There is a slight increase in the lumbar curve. (b) Lateral X-ray of the spine in standing position.
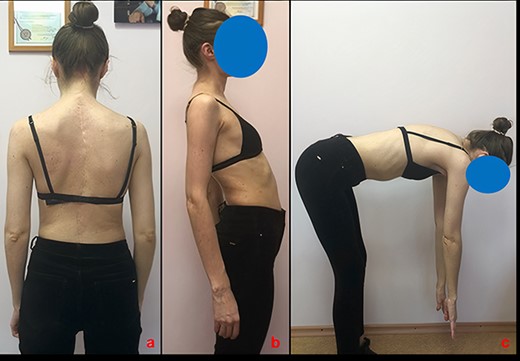
Appearance of the patient and the range of motion in the spine at a 10-year follow-up. (a) View from the back. (b) Side view in spinal extension. (c) Side view in spinal flexion.
DISCUSSION
Traditional growing rods (TGR) have been the gold standard of treatment of scoliosis with early progression, allowing for gradual correction and continued spinal growth in young patients. TGR treatment requires open surgical distraction every 6 months to achieve optimal correction of the deformity and facilitate the growth of the spine [3, 4]. A number of authors [5, 6] have determined the force and length of distraction observed in patients undergoing TGR treatment. These authors describe the effect of sequentially reducing potential of further spine growth during staged lengthening interventions, in which the distraction forces increased, whereas the length of distraction decreased with each successive stage of distraction [5, 6]. Staged interventions inevitably cause soft tissue damage, and coupled with excessive distraction forces applied to the spine at each distraction lead to a decrease in the flexibility of the spine due to scar tissue formation and/or spontaneous fusion in 89% of patients, significantly limiting total correction potential at final fusion [7].
Chewing et al. [8] proposed a method for performing repeated distractions of the spine without limiting spine lengthening potential using magnetic growing rods (MGRs). The average coronal deformity Cobb angle improved from 56.9° to 29.8° after surgery and was maintained thereafter. The average increase in T1-S1 length was 3.9 mm during the first 6 months and 10.6 mm during the following 6 months. These authors demonstrate that with correct MGR use, it is possible to achieve spine deformity correction without limiting the lengthening potential of the implants. It should be noted that the maximum technically possible lengthening of the magnetic rods is 48 mm and is usually achieved by the 2-year postoperative mark, following which definitive fusion is usually required [8].
Recent studies continue to indicate that the most common clinical problem associated with MGR treatment is failure of the distraction mechanism, which leads to revision surgeries and implant replacement [9]. In the largest series, Rushton et al. analyzed 99 explanted magnetic rods from 53 patients. The spinal distraction rate negatively correlated with the duration the implants remained within the patients (r = −0.47, P = 0.004). In total, 34 out of 55 rods were non-functional at the time of removal [10].
The LSZ growing system does not require staged surgical interventions, bony structure integrity of the spine is not violated during correction and pedicle screws are not used, which does not violate growth zones of vertebrae and significantly limit surgical morbidity, as the placement of LSZ hooks only requires exposure of the base of the spinous processes, in turn significantly reducing the potential for spontaneous fusion. The advantages of this novel growing system include the possibility of preserving the growth potential of the spinal column, its relatively low cost, ease of installation and the possibility of achieving substantial correction at the initial stage of surgical treatment.
At the time of initial presentation, the patient could have undergone definitive posterior instrumentation, which would have required a longer construct and consequently limited mobility of the lumbar spine. Using the described technique made it possible to ultimately perform selective definitive instrumentation, which allowed to preserve near full range of movement in the lumbar spine and positively affected the patient’s quality of life.



