-
PDF
- Split View
-
Views
-
Cite
Cite
Gitte Grunnet Raabe, Benedicte Schelde-Olesen, Thomas Bjørsum-Meyer, Idiopathic asymptomatic pneumoperitoneum in a patient with ureteric calculus and Crohn’s disease, Journal of Surgical Case Reports, Volume 2022, Issue 3, March 2022, rjac072, https://doi.org/10.1093/jscr/rjac072
Close - Share Icon Share
Abstract
A 46-year-old male referred to the Emergency Department with pain in the left flank. The patient suffered from Crohn’s disease. He had not experienced any fever, and a urine strip showed signs of blood. A ureteric calculus was suspected and a computed tomography scan was performed, which surprisingly showed free intraperitoneal air (FIA) located along the ascending colon. The patient had no signs indicative of peritonitis and the spontaneous pneumoperitoneum was suspected. Pneumoperitoneum is often associated with severe intraabdominal pathology, such as perforation of the gastrointestinal tract, requiring acute surgical intervention. In ~10% of all cases of FIA, the cause is related to conditions not requiring prompt surgical intervention. Doctors need to recognize the rare condition of spontaneous pneumoperitoneum and correlate these findings to patient complaints to be able to choose the correct conservative strategy and to avoid unnecessary surgical procedures and risks for the patient.
INTRODUCTION
Pneumoperitoneum refers to the presence of free air in the abdominal cavity and it is often a sign of severe intraabdominal pathology, such as perforation of abdominal viscus, that requires acute surgical intervention. In rare cases, the presence of pneumoperitoneum is observed in patients with intact viscus and this condition has been termed as idiopathic or non-surgical pneumoperitoneum and is considered to be a benign condition that can be managed conservatively [1].
Computed tomography (CT) of the abdomen is the preferred modality for hemodynamically stable patients with abdominal pain and unresolved condition. Free air in the peritoneal cavity may be present without relation to patient complaints or clinical findings. This may put the clinician in a dilemma. Is it reasonable to discharge the patients if no other findings require hospitalization? Are further examinations required, such as e.g. endoscopy or acute laparoscopy/laparotomy?
We present an unusual case in a patient presenting with acute left flank pain where subsequent CT is described with a left ureteric calculus, but surprisingly, also free intraperitoneal air (FIA) adjacent to the right colon.
CASE REPORT
A 46-year old male referred to the Emergency Department (ED) presented with pain in the left flank as the only symptom.
The pain arose acutely 24 hours before hospital admission and was only located in the left flank. He denied voiding difficulties and had not experienced any fever.
The patient suffered from Crohn’s disease and had a permanent colostomy after previous bowel resection but was otherwise healthy. Last abdominal surgery was 7 years ago.
Blood test on hospital admission: Hgb: 9.9 mmol/l (8.3–10–5), leucocytes: 9.57 × 109/l (3.5–8.8), creatinine: 107 μmol/l (60–105) and C-reactive protein: 24 mg/l (<6).
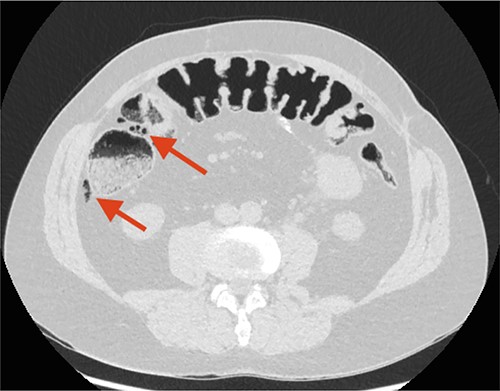
A non-contrast CT scan showed FIA located along the right colon flexure, calyceal calculi located in the left kidney and sequelae from former sigmoid colectomy with stoma formation (Fig. 1). There where no wall thickness of the colon indicating activity in the patient's Crohn's disease.

The initial CT scan. The arrow points at free intraperitoneal air (FIA) located along the right colon flexure.
The patient had pain in the left flank but was otherwise stable without symptoms of FIA. The tentative diagnosis was nephrolithiasis and an asymptomatic fistula from Crohn’s disease, and he was treated conservatively with two types of antibiotics for 5 days and discharged on the same day.
Two days later, the patient returned with intensified pain in the left flank, and a CT scan showed a calculi in the left ureter and progression in the free air located along the ascending colon (Fig. 2). The patient had no abdominal physical signs indicative of peritonitis, no fever and normal blood test.
CT scan performed 2 days after the first admission to the Emergency Department (ED). The arrow points at remaining FIA along the ascending colon/right flexure.
Three weeks later, a CT urography showed FIA, but the patient still had no symptoms indicative of peritonitis. Three months later, a CT scan showed progression of FIA and air bubbles in the wall of the ascending colon (Fig. 3).
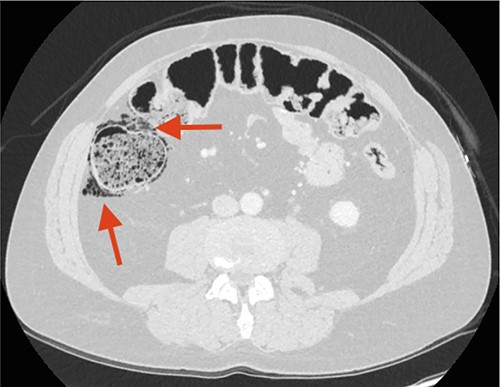
CT scan performed 3 months after the first admission to the ED. The arrow points at increased FIA and air bubbles in the colonic wall as signs of Pneumatosis cystoides Intestinalis, PCI.
Pneumatosis cystoides intestinalis (PCI) was suspected.
Retrospectively, the two initial CT scans were reviewed with an independent radiologist, and gas-filled cysts were located in the wall of the ascending colon, representing PCI on both CT scans.
DISCUSSION
Occasionally, a clinically stable patient with abdominal pain will surprisingly present with FIA. In the article by Mularski et al., they reported that in ~10% of all cases of FIA, the cause was related to conditions not requiring prompt surgical intervention [2]. This is often related to intrathoracic, intra-abdominal, gynecological or idiopathic causes as listed in the article by Mularski et al. [2] (Table 1). In a more recent article by Wataru et al., PCI was observed in 24.7% of cases, with non-iatrogenic extraluminal free air [3], indicating that PCI are relatively common. The observations made by Mularski et al. were mainly based on plain radiography, whereas the results from Wataru et al. were based on CT scans. The increased imaging detection of PCI could be related to the increased use of CT scans.
| Category . | Cause of pneumoperitoneum . |
|---|---|
| Post-operative | Retained air from open laparotomy Retained air from laparoscopy |
| Abdominal | PCI Endoscopic procedures Postpolypectomy syndrome Peritoneal dialysis Collagen vascular disease Pneumocholecystitis Jejunal and sigmoid diverticulitis Distended hollow viscus Subclinical perforated viscus |
| Thoracic | Intermittent positive-pressure ventilation Barotrauma Increased intrathoracic pressure—cough, etc. Asthma Bronchoscopy Cardiopulmonary resuscitation and mouth-to-mouth ventilation Adenotonsillectomy Pulmonary tuberculosis Blunt trauma Bronchopulmonary fistula Spontaneous rupture of pulmonary blebs |
| Gynecological | Vaginal insufflation Knee-chest exercises Pelvic inflammatory disease Coitus Gynecological examination procedures Vaginal douching |
| Idiopathic |
| Category . | Cause of pneumoperitoneum . |
|---|---|
| Post-operative | Retained air from open laparotomy Retained air from laparoscopy |
| Abdominal | PCI Endoscopic procedures Postpolypectomy syndrome Peritoneal dialysis Collagen vascular disease Pneumocholecystitis Jejunal and sigmoid diverticulitis Distended hollow viscus Subclinical perforated viscus |
| Thoracic | Intermittent positive-pressure ventilation Barotrauma Increased intrathoracic pressure—cough, etc. Asthma Bronchoscopy Cardiopulmonary resuscitation and mouth-to-mouth ventilation Adenotonsillectomy Pulmonary tuberculosis Blunt trauma Bronchopulmonary fistula Spontaneous rupture of pulmonary blebs |
| Gynecological | Vaginal insufflation Knee-chest exercises Pelvic inflammatory disease Coitus Gynecological examination procedures Vaginal douching |
| Idiopathic |
| Category . | Cause of pneumoperitoneum . |
|---|---|
| Post-operative | Retained air from open laparotomy Retained air from laparoscopy |
| Abdominal | PCI Endoscopic procedures Postpolypectomy syndrome Peritoneal dialysis Collagen vascular disease Pneumocholecystitis Jejunal and sigmoid diverticulitis Distended hollow viscus Subclinical perforated viscus |
| Thoracic | Intermittent positive-pressure ventilation Barotrauma Increased intrathoracic pressure—cough, etc. Asthma Bronchoscopy Cardiopulmonary resuscitation and mouth-to-mouth ventilation Adenotonsillectomy Pulmonary tuberculosis Blunt trauma Bronchopulmonary fistula Spontaneous rupture of pulmonary blebs |
| Gynecological | Vaginal insufflation Knee-chest exercises Pelvic inflammatory disease Coitus Gynecological examination procedures Vaginal douching |
| Idiopathic |
| Category . | Cause of pneumoperitoneum . |
|---|---|
| Post-operative | Retained air from open laparotomy Retained air from laparoscopy |
| Abdominal | PCI Endoscopic procedures Postpolypectomy syndrome Peritoneal dialysis Collagen vascular disease Pneumocholecystitis Jejunal and sigmoid diverticulitis Distended hollow viscus Subclinical perforated viscus |
| Thoracic | Intermittent positive-pressure ventilation Barotrauma Increased intrathoracic pressure—cough, etc. Asthma Bronchoscopy Cardiopulmonary resuscitation and mouth-to-mouth ventilation Adenotonsillectomy Pulmonary tuberculosis Blunt trauma Bronchopulmonary fistula Spontaneous rupture of pulmonary blebs |
| Gynecological | Vaginal insufflation Knee-chest exercises Pelvic inflammatory disease Coitus Gynecological examination procedures Vaginal douching |
| Idiopathic |
In this case, PCI was believed to be the underlying cause of pneumoperitoneum.
PCI refers to clinical or radiological finding of gas-filled cysts within the intestinal wall and is known to cause spontaneous pneumoperitoneum. Pneumoperitoneum can arise when one or more cysts rupture, releasing gas into the abdominal cavity without communication to the bowel lumen. Symptoms of PCI can vary greatly. A previous review of cases involving PCI reported the following symptoms in decreasing frequency: abdominal pain, nausea and vomiting, distended abdomen, rectal bleeding or bloody stool, diarrhea and constipation [4].
PCI is a low incidence disease and the etiology and pathogenesis are still unclear. PCI is thought to be related to an increase in intra-intestinal pressure and disruption in mucosal integrity [5, 6]. A combination of these factors can lead to accumulation of gas produced by aerogenic bacteria, creating cysts containing gas with high levels of hydrogen. The effect of treatment with antibiotics in patients with symptomatic PCI supports this theory [7–11].
Treatment with inspired oxygen is found to be beneficial [9, 12]. Maintaining a high arterial partial pressure of oxygen is believed to facilitate diffusion of non-oxygen gas from the cysts [6].
PCI is not a disease, but a radiological sign of underlying pathology, and its significance is directly related to the patients’ clinical status. Pneumoperitoneum is reported to be present in 9–19.8% of PCI cases. [13, 14]. The majority of cases with PCI are benign, and in patients where signs of peritonitis, fever and leucocytosis are absent, treatment is not indicated [2, 3].
Youran G. et al. report that PCI is a known but rare condition related to inflammatory bowel disease [5]. The patient in this case report was diagnosed with Crohn’s disease, and the CT scans all showed intramural gas in the colon characteristic for PCI.
In summation, obtaining a detailed anamnesis is important to identify the possible etiology of spontaneous pneumoperitoneum and it should contain prior surgical interventions and iatrogenic causes, such as gastrointestinal endoscopy or abdominal surgery within the last 30 days, considering that pneumoperitoneum can persist weeks after surgery [15]. Any other predisposing circumstances (Table 1) should be uncovered.
The clinical symptoms and signs determine the indication for acute surgical intervention [1]. Surgery is inevitable if the patient is hemodynamically unstable or presents with diffuse peritonitis, but if the patient is stable and there are no abdominal physical signs indicative of peritonitis, a conservative strategy is recommended [1].
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.
References
Adachi W, Matsushita T, Yashiro Y, Imura J, Shiozawa H, Kishimoto K.
Gao Y, Uffenheimer M, Ashamallah M, Grimaldi G, Swaminath A, Sultan K.
Koppikar S, Yu D, Ropeleski M, Robertson D.
Than VS, Nguyen MD, Gallon A, Pham MT, Nguyen DH, Boyer L, et al.
Park CS, Hwang S, Jung DH, Song GW, Moon DB, Ahn CS, et al.
Koysombat K, Capanna MV, Stafford N, Orchard T.
Chapman BC, McIntosh KE, Jones EL, Wells D, Stiegmann GV, Robinson TN.



