-
PDF
- Split View
-
Views
-
Cite
Cite
Kei Takeda, Ikuya Miyamoto, Ryosuke Abe, Tadashi Kawai, Yu Ohashi, Hiroyuki Yamada, Tophaceous pseudogout of the temporomandibular joint extending into the cranium: a case report with literature review, Journal of Surgical Case Reports, Volume 2022, Issue 3, March 2022, rjac055, https://doi.org/10.1093/jscr/rjac055
Close - Share Icon Share
Abstract
Pseudogout is a disease characterized by calcium pyrophosphate crystal deposition. Involvement of the temporomandibular joint (TMJ) is rare. We herein report a case of tophaceous pseudogout of the TMJ with cranial extension. An 83-year-old woman was referred to our institution for treatment of right TMJ pain. The patient’s medical and family histories were unremarkable. Magnetic resonance imaging showed a mass of about 35 mm in diameter compressing the bottom of the right temporal lobe of the brain. Based on a clinical diagnosis of a right TMJ tumour, biopsy was performed under general anaesthesia. The histopathological diagnosis was pseudogout. Considering the risk of surgically induced brain damage, the patient’s advanced age and her relatively good quality of life, the treatment plan simply involved the observation of the lesion. Fourteen months after biopsy, the patient’s activities of daily living remained unchanged and she had no TMJ pain.
INTRODUCTION
Pseudogout is a disease characterized by calcium pyrophosphate crystal deposition, and it usually occurs in individuals older than 50 years. The most frequently involved joint is the knee, followed by the wrists, elbows, shoulders and ankles [1]. Involvement of the temporomandibular joint (TMJ) is rare; furthermore, only nine cases of pseudogout of the TMJ extending into the skull base have been reported in the English-language
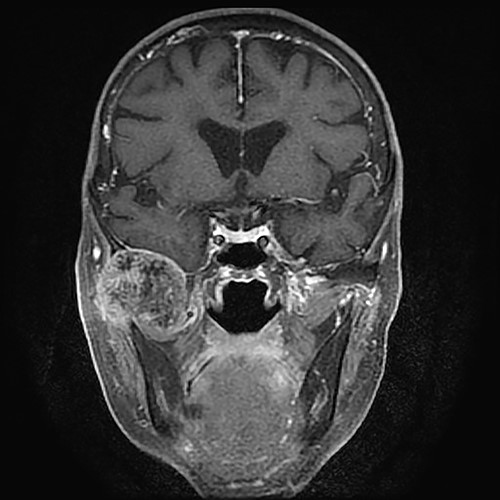
Gadolinium-enhanced T1-weighted magnetic resonance imaging showing the TMJ mass compressing the bottom of the right temporal lobe of the brain.
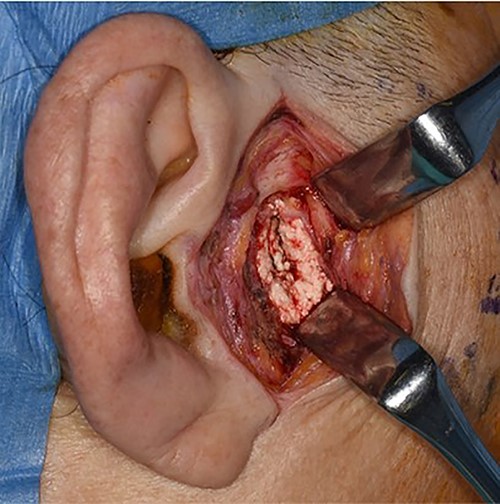
Intra-operative photograph showing a mass of white substance in the temporomandibular region.
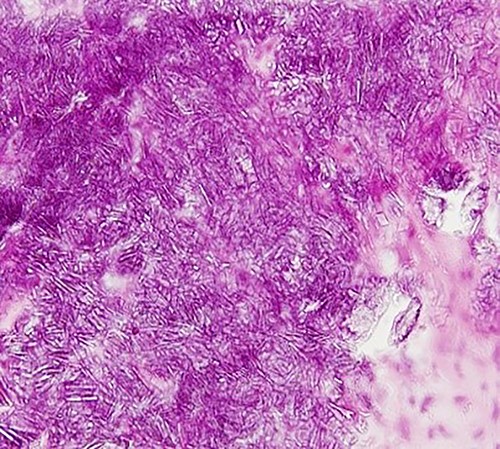
Photomicrograph showing lobular basophilic materials with variously sized rectangular or parallelogram-shaped crystals (haematoxylin–eosin stain, ×400).
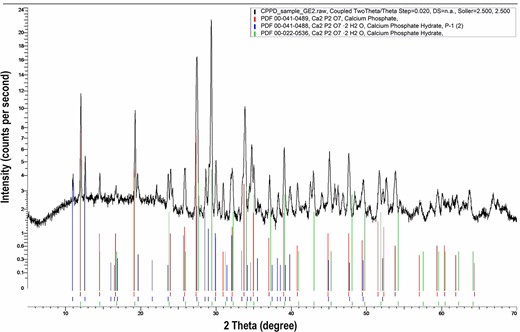
The result of X-ray diffraction analysis of the biopsy specimen showing the pattern of calcium pyrophosphate crystals.
literature [2–9]. Because of the rarity of this condition, the treatment outcome of such cases was not elucidated.
We herein report a case of large pseudogout of the TMJ with cranial extension and present a review of the literature.
CASE REPORT
An 83-year-old woman was referred to our institution for treatment of right TMJ pain. She had first noticed the pain ~3 years earlier. The patient’s medical and family histories were unremarkable. Intra-oral examination revealed no abnormal findings associated with the right TMJ pain. Occlusal deviation was not observed. The maximum mouth opening was 28 mm, and transient pain occurred during mouth opening. A hard protrusion was observed in the right TMJ region. There was no evidence of cranial nerve paralysis or cervical lymphadenopathy. On T1- and T2-weighted magnetic resonance coronal images, the mass showed low signal intensity and compressed the bottom of the right temporal lobe of the brain. The mass about 35 mm in diameter was inhomogeneously enhanced by gadolinium (Fig. 1). The patient’s calcium, phosphate and uric acid concentrations were within the reference range.
Based on a clinical diagnosis of a right TMJ tumour, biopsy was performed under general anaesthesia (Fig. 2). Histopathological examination revealed lobular basophilic materials surrounded by fibrous tissue. Variously sized rectangular or parallelogram-shaped crystals were irregularly present within the basophilic materials (Fig. 3). These crystals were identified under polarized light.
The result of X-ray diffraction analysis of the biopsy specimen was consistent with the pattern of calcium pyrophosphate crystals (Fig. 4).
The final diagnosis of tophaceous pseudogout of the right TMJ was made based on these findings. A neurosurgical consultation in our hospital was performed. Considering the risk of surgically induced brain damage, the patient’s advanced age and her relatively good quality of life, the treatment plan simply involved the observation of the lesion with pain control. Fourteen months after biopsy, the patient was pain-free and her activities of daily living had remained unchanged.
| No . | Author . | Year . | Age/sex . | Symptoms . | Size of the lesion (cm) . | Image findings relating to skull base . | Treatment . | Post-operative complications . | Follow-up periods . |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Grant [2] | 1999 | 65/F | Facial fullness, discomfort, pain, facial swelling | 4.8 × 5.6 × 6.5 | Extending into the middle cranial fossa | Surgery | Not documented | 6 w |
| 2 | Nicholas [3] | 2007 | 35/M | External auditory canal tenderness | NA | Eroding into the middle cranial fossa | Surgery (partial superficial parotidectomy + infratemporal fossa dissection) | Not documented | NA |
| 3 | Kudoh [4] | 2017 | 38/M | Mild pain in the chin and tip of the tongue, preauricular swelling | NA | Erosive bone resorption at the base of the skull | Observation after biopsy | No complication No change in size | 36 m |
| 4 | Hotokezaka [5] | 2020 | 59/F | Cheek swelling, pain, trismus | NA | Destroying the glenoid fossa | Surgery | No complication No mass recurrence | 168 m |
| 5 | Abou-Foul [6] | 2020 | 56/F | TMJ discomfort, swelling, trismus | 2 × 3 | Skull base erosion | Surgery (resection and total TMJ reconstruction) | No complication No mass recurrence | 24 m |
| 6 | Houghton [7] | 2020 | 55/F | Painless preauricular mass | 2 | Erosion into the middle cranial fossa | Surgery | No complication No mass recurrence | 12 m |
| 7 | Tnag [8] | 2021 | 46/F | Temporal swelling and pain, chewing discomfort | 2 × 2 | Destroying the glenoid fossa | Surgery (resection and arthroplasty) | No complication No mass recurrence | 1 w |
| 8 | Tnag [8] | 2021 | 52/M | Mass in the TMJ area pain and tinnitus | 4 × 4 | The mass infiltrated the middle cranial fossa | Surgery (resection and TMJ reconstruction) | No complication No mass recurrence | 12 m |
| 9 | Morita [9] | 2021 | 83/F | Cheek swelling | 5 × 6 | Erosion of mid-cranial fossa | Surgery | Conductive hearing loss | 4 m |
| 10 | Present case | 83/F | TMJ pain, trismus | 3.7 × 3.3 | The mass compressed the middle cranial fossa | Observation after biopsy | No complication slight increase in size | 14 m |
| No . | Author . | Year . | Age/sex . | Symptoms . | Size of the lesion (cm) . | Image findings relating to skull base . | Treatment . | Post-operative complications . | Follow-up periods . |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Grant [2] | 1999 | 65/F | Facial fullness, discomfort, pain, facial swelling | 4.8 × 5.6 × 6.5 | Extending into the middle cranial fossa | Surgery | Not documented | 6 w |
| 2 | Nicholas [3] | 2007 | 35/M | External auditory canal tenderness | NA | Eroding into the middle cranial fossa | Surgery (partial superficial parotidectomy + infratemporal fossa dissection) | Not documented | NA |
| 3 | Kudoh [4] | 2017 | 38/M | Mild pain in the chin and tip of the tongue, preauricular swelling | NA | Erosive bone resorption at the base of the skull | Observation after biopsy | No complication No change in size | 36 m |
| 4 | Hotokezaka [5] | 2020 | 59/F | Cheek swelling, pain, trismus | NA | Destroying the glenoid fossa | Surgery | No complication No mass recurrence | 168 m |
| 5 | Abou-Foul [6] | 2020 | 56/F | TMJ discomfort, swelling, trismus | 2 × 3 | Skull base erosion | Surgery (resection and total TMJ reconstruction) | No complication No mass recurrence | 24 m |
| 6 | Houghton [7] | 2020 | 55/F | Painless preauricular mass | 2 | Erosion into the middle cranial fossa | Surgery | No complication No mass recurrence | 12 m |
| 7 | Tnag [8] | 2021 | 46/F | Temporal swelling and pain, chewing discomfort | 2 × 2 | Destroying the glenoid fossa | Surgery (resection and arthroplasty) | No complication No mass recurrence | 1 w |
| 8 | Tnag [8] | 2021 | 52/M | Mass in the TMJ area pain and tinnitus | 4 × 4 | The mass infiltrated the middle cranial fossa | Surgery (resection and TMJ reconstruction) | No complication No mass recurrence | 12 m |
| 9 | Morita [9] | 2021 | 83/F | Cheek swelling | 5 × 6 | Erosion of mid-cranial fossa | Surgery | Conductive hearing loss | 4 m |
| 10 | Present case | 83/F | TMJ pain, trismus | 3.7 × 3.3 | The mass compressed the middle cranial fossa | Observation after biopsy | No complication slight increase in size | 14 m |
F: female, M: male, NA: not applicable, w: week, m: month.
| No . | Author . | Year . | Age/sex . | Symptoms . | Size of the lesion (cm) . | Image findings relating to skull base . | Treatment . | Post-operative complications . | Follow-up periods . |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Grant [2] | 1999 | 65/F | Facial fullness, discomfort, pain, facial swelling | 4.8 × 5.6 × 6.5 | Extending into the middle cranial fossa | Surgery | Not documented | 6 w |
| 2 | Nicholas [3] | 2007 | 35/M | External auditory canal tenderness | NA | Eroding into the middle cranial fossa | Surgery (partial superficial parotidectomy + infratemporal fossa dissection) | Not documented | NA |
| 3 | Kudoh [4] | 2017 | 38/M | Mild pain in the chin and tip of the tongue, preauricular swelling | NA | Erosive bone resorption at the base of the skull | Observation after biopsy | No complication No change in size | 36 m |
| 4 | Hotokezaka [5] | 2020 | 59/F | Cheek swelling, pain, trismus | NA | Destroying the glenoid fossa | Surgery | No complication No mass recurrence | 168 m |
| 5 | Abou-Foul [6] | 2020 | 56/F | TMJ discomfort, swelling, trismus | 2 × 3 | Skull base erosion | Surgery (resection and total TMJ reconstruction) | No complication No mass recurrence | 24 m |
| 6 | Houghton [7] | 2020 | 55/F | Painless preauricular mass | 2 | Erosion into the middle cranial fossa | Surgery | No complication No mass recurrence | 12 m |
| 7 | Tnag [8] | 2021 | 46/F | Temporal swelling and pain, chewing discomfort | 2 × 2 | Destroying the glenoid fossa | Surgery (resection and arthroplasty) | No complication No mass recurrence | 1 w |
| 8 | Tnag [8] | 2021 | 52/M | Mass in the TMJ area pain and tinnitus | 4 × 4 | The mass infiltrated the middle cranial fossa | Surgery (resection and TMJ reconstruction) | No complication No mass recurrence | 12 m |
| 9 | Morita [9] | 2021 | 83/F | Cheek swelling | 5 × 6 | Erosion of mid-cranial fossa | Surgery | Conductive hearing loss | 4 m |
| 10 | Present case | 83/F | TMJ pain, trismus | 3.7 × 3.3 | The mass compressed the middle cranial fossa | Observation after biopsy | No complication slight increase in size | 14 m |
| No . | Author . | Year . | Age/sex . | Symptoms . | Size of the lesion (cm) . | Image findings relating to skull base . | Treatment . | Post-operative complications . | Follow-up periods . |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Grant [2] | 1999 | 65/F | Facial fullness, discomfort, pain, facial swelling | 4.8 × 5.6 × 6.5 | Extending into the middle cranial fossa | Surgery | Not documented | 6 w |
| 2 | Nicholas [3] | 2007 | 35/M | External auditory canal tenderness | NA | Eroding into the middle cranial fossa | Surgery (partial superficial parotidectomy + infratemporal fossa dissection) | Not documented | NA |
| 3 | Kudoh [4] | 2017 | 38/M | Mild pain in the chin and tip of the tongue, preauricular swelling | NA | Erosive bone resorption at the base of the skull | Observation after biopsy | No complication No change in size | 36 m |
| 4 | Hotokezaka [5] | 2020 | 59/F | Cheek swelling, pain, trismus | NA | Destroying the glenoid fossa | Surgery | No complication No mass recurrence | 168 m |
| 5 | Abou-Foul [6] | 2020 | 56/F | TMJ discomfort, swelling, trismus | 2 × 3 | Skull base erosion | Surgery (resection and total TMJ reconstruction) | No complication No mass recurrence | 24 m |
| 6 | Houghton [7] | 2020 | 55/F | Painless preauricular mass | 2 | Erosion into the middle cranial fossa | Surgery | No complication No mass recurrence | 12 m |
| 7 | Tnag [8] | 2021 | 46/F | Temporal swelling and pain, chewing discomfort | 2 × 2 | Destroying the glenoid fossa | Surgery (resection and arthroplasty) | No complication No mass recurrence | 1 w |
| 8 | Tnag [8] | 2021 | 52/M | Mass in the TMJ area pain and tinnitus | 4 × 4 | The mass infiltrated the middle cranial fossa | Surgery (resection and TMJ reconstruction) | No complication No mass recurrence | 12 m |
| 9 | Morita [9] | 2021 | 83/F | Cheek swelling | 5 × 6 | Erosion of mid-cranial fossa | Surgery | Conductive hearing loss | 4 m |
| 10 | Present case | 83/F | TMJ pain, trismus | 3.7 × 3.3 | The mass compressed the middle cranial fossa | Observation after biopsy | No complication slight increase in size | 14 m |
F: female, M: male, NA: not applicable, w: week, m: month.
DISCUSSION
To the best of our knowledge, 10 cases (including the present case) of pseudogout of TMJ extending into the skull base have been reported in the English-language literature (Table 1). The most frequent clinical symptoms in these cases were swelling and pain in five patients and trismus in three patients. No patients had symptoms related to a central nervous system disorder. Pseudogout was pre-operatively diagnosed in 8 of the 10 patients. The remaining two patients were diagnosed with a neoplastic lesion or synovial osteochondromatosis [5] and synovial chondromatosis [7], respectively. General treatment of pseudogout is supportive to minimize symptoms [1]; however, tophaceous pseudogout that destroys surrounding structures sometimes requires surgery. Surgery was performed in six (75%) of the eight reported cases correctly diagnosed as pseudogout pre-operatively. Cerebrospinal fluid leakage occurred as an intra-operative complication in one patient [8]. Exposure of the dura mater was overlaid using a flap of temporal muscle [2, 5, 9], temporalis fascia [7], harvested fat [2] and bone wax [8]. No patients developed brain damage as a post-operative complication. However, conductive hearing loss was reported in one 83-year-old patient [9]. To avoid possible surgically induced complications, observation was selected in two patients, including ours. These patients experienced no deterioration of clinical symptoms within the follow-up period [4]. Because our patient’s oral dysfunction in daily life was mild, observation with pain control was selected.
ACKNOWLEDGEMENT
We thank Professor Yasunori Takeda from the Division of Clinical Pathology, Department of Oral and Maxillofacial Reconstructive Surgery, School of Dentistry, Iwate Medical University for assisting with the pathological diagnosis of this case. We also thank Angela Morben, DVM, ELS, from Edanz (https://jp.edanz.com/ac), for editing a draft of this manuscript.
CONFLICT OF INTEREST STATEMENT
None.
ETHICS STATEMENT/CONFIRMATION OF PATIENT’S PERMISSION
Ethics approval was not required. Written consent was obtained by patient for use of the photographs in this report.



