-
PDF
- Split View
-
Views
-
Cite
Cite
Mirwais Khan Hotak, Mike He, Trichoblastic fibroma mimicking sarcoma, Journal of Surgical Case Reports, Volume 2022, Issue 2, February 2022, rjac042, https://doi.org/10.1093/jscr/rjac042
Close - Share Icon Share
Abstract
Trichoblastic fibroma (TF) is a benign trichogenic tumour that has both epithelial and mesenchymal components and exhibits partial to complete follicular induction.TF is rare and in our case it is mimicking sarcoma. We report a 35-year-old gentleman who presented with a lump over his left lower leg for the last 15 years. The lump was gradually increasing in size with a slight discomfort, no pain or any other symptoms. Consequently, the patient had an ultrasound which revealed bilobed solid lesion, and ultrasound-guided core biopsy revealed basaloid neoplasm. After positron emission tomography scan and discussion in MDT wide local excision performed. The histopathology revealed TF. Hence, TF should be included in differential diagnosis of relative superficial suspicious sarcomas. If there is any suspicion and changes in behaviour of long-term stable nodules they should be excised with a clear margin as there are aggressive TF reported in the literature.
INTRODUCTION
Tricoblastic fibroma is a benign, rare skin tumour originating from hair follicles. The two variants are plaque and nodular. The plaque variant is almost exclusively located on the face with deep tissue infiltration. Trichoblastoma includes all benign cutaneous neoplasms usually composed of follicular germinative cells. According to Altman [1], the plaque variant of trichoblastic fibroma (TF) is a poorly circumscribed neoplasm, particularly at its lateral and deep margins. Local observation supports the mitotic figures as being more numerous in the plaque variant of TF which considers this clinical variant as a low-grade follicular malignancy [1].
CASE PRESENTATION
We present a case of a 35-year-old gentleman who reported a lump over his left lower leg for the last 15 years. He noticed within the last few months as it gradually increased in size with a slight discomfort, no pain or any other symptoms. He is fit and healthy apart from mild asthma which requires ventolin occasionally and he also suffers from anxiety. He has no other skin disease. Routine investigations including full blood count, urea, electrolytes and liver function tests were performed which were unremarkable. Consequently, the patient had an ultrasound which revealed bilobed solid lesion within the subcutaneous fat measuring 39x15x24 mm, suspicious for neoplasm (Fig. 1). Initially, an ultrasound-guided core biopsy was performed and it was consistent with basaloid neoplasm (Fig. 2).
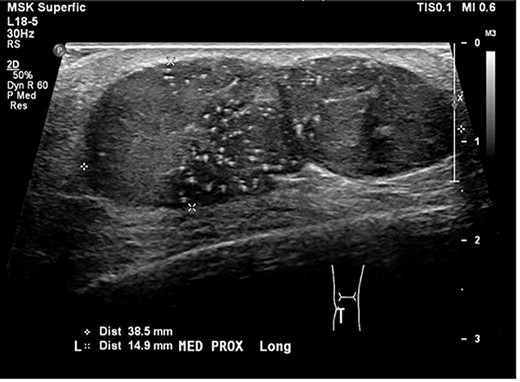
an ultrasound scan shows bilobed solid lesion measuring 39x15x24 mm.
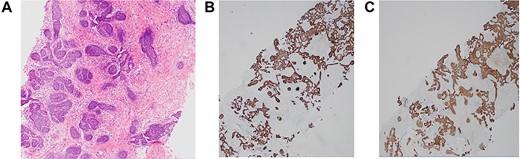
histopathology slides of a 35-year-old patient. (A) Haematoxylin and eosin (H&E) image. (B) p63 stain image. (C) CK5 stain image.
Subsequently, due to the report suggesting neoplasm the patient had 18-FDG positron emission tomography computed tomography scan. The finding was consistent with a 13 mm soft tissue nodule at left lower leg. The nodule appeared solitary with mild FDG avidity, potentially it will be low grade given such a mild avidity on PET scan report. No other metastatic or synchronous lesion was identified.
The patient was discussed in a multidisciplinary team meeting and advised for formal excision. The patient underwent an elective wide local excision and key stone flap and he was discharged from hospital with no complications. Post discharge from hospital, he developed superficial wound dehiscence, which was managed with regular wound care by community nurse and it healed completely. The final histopathology was consistent with benign trophoblastic fibroma (Fig. 3). On further follow-up, patient was discharged from surgical outpatient clinic with no recurrence.
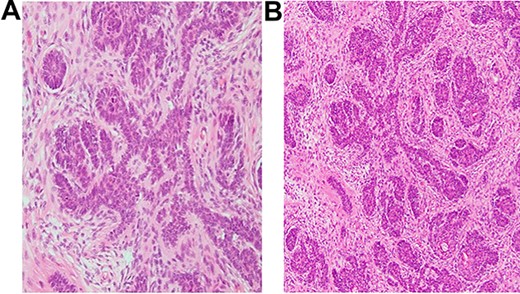
histopathology slides of a 35-year-old patient. (A and B) Dermal-based nodule with proliferating nests and cords of basaloid cells on a background of fibrotic stroma and presence of scattered mature folliculocystic structures.
DISCUSSION
TF is a benign trichogenic tumour that has both epithelial and mesenchymal components and exhibits partial to complete follicular induction [2]. Trichoblastoma is a predominant tumour of hair follicle, characterized by well-circumscribed nests and cords of bland follicular basaloid cells in close association with stroma [3].
Although there seems to be a close relationship to trichoepitheliomas, this tumour deserves a separation from classical conventional trichoepitheliomas. TF differs from these by nodular character, unusual location, size, consistency, involvement of deeper tissues, age of patients and additional histopathologic findings [4].
There are two clinical presentations of TF, nodular and plaque variants. The plaque variant is almost exclusively located on the face with deep tissue infiltration [1]. According to the biggest case series of 10 cases, all tumours were located on the face. Nine out of 10 patients were women. The mean age at presentation was 63.8 years, ranging from 35 to 81 years [2]. There are a couple of theories about plaque variant of TF. One of them suggests that plaque variant of TF is a poorly circumscribed neoplasm, with numerous mitotic figures and considers this clinical variant as a low-grade follicular malignancy [1]. Contrary to this, the other theory suggests the plaque variant is just a large trophoblast fibroma and entirely benign [1].
TF has been reported on other parts of the body as solitary, mobile, subcutaneous nodules with normal overlying skin. They have been reported on the vulva, scalp predominantly in women [5]. In one study, six TFs were reported with five female patients and one male. Three tumours were on the back, one was reported on the left gluteus, one on right skull and one on left thigh. They were reported on patients aging from 1 to 20 years varied in size from 1.8 to 6 cm [4]. There is a breast TF reported with contralateral breast cancer. In this case, the ultrasound scan and mammogram suggested benign lesion but MRI suggested malignancy due to the presence of choline regardless of the concentration. The histopathology of lesion confirmed TF [6].
In one of the studies, a locally aggressive trichoblastoma was revealed in patients that had a median age of 64 years at diagnosis (range 39–98 years), with male predominance (63.9%). The sites involved were most often the face (60%) followed by the trunk (20%) and the limbs (17.1%) [4].
Trichoblastomas and basal cell carcinomas (BCCs) can sometimes be difficult to differentiate histologically on biopsy samples [5]. Sellheyer et al. [5] showed that PHLDA1, a follicular stem cell marker, differentiated between desmoplastic trichoepithelioma (PHLDA1+) and morpheaform BCC (PHLDA1−). Here, we showed that locally aggressive trichoblastic tumours almost always have some degree of PHLDA1 expression, a feature that may be useful to differentiate such tumours from BCC [5].
There is no consensus in the literature about the surgical management of trichoblastic tumours with locally aggressive growth. Complete excision with free surgical margins seems mandatory. The recommendation is a 10 mm initial lateral margin from the palpable tumour, and an excision including the entire subcutis, until the first fascial plan as deep margin [5].
Our patient was male and 35 years old with a rare presentation of TF which mimic sarcoma initially and after wide local excision with 10 mm margin and flap it was concluded as TF. Patient had no recurrence on follow-up and no further follow-up was required.
In summary TF should be included in differential diagnosis of relative superficial suspicious sarcomas. If there is any suspicion and changes in behaviour of long-term stable nodules they should be excised with a clear margin as there are aggressive TF reported in the literature.
ACKNOWLEDGEMENT
1. Dr Sumi Ranjit, Pathologist, Anatomical Pathology and Haematology Department, Capital Pathology.
2. Dr Jaswini Sivalingam Anatomical Pathologist Registrar, Canberra Hospital.



