-
PDF
- Split View
-
Views
-
Cite
Cite
Amjad Alshammari, Eman Aljufairi, Anwaar Alsayed, Oncocytic mucoepidermoid carcinoma of the parotid gland: case report, Journal of Surgical Case Reports, Volume 2022, Issue 2, February 2022, rjac039, https://doi.org/10.1093/jscr/rjac039
Close - Share Icon Share
Abstract
Mucoepidermoid carcinoma is the most common malignant tumour of salivary glands. Oncocytic variant is rare and could be mistaken for benign entities like oncocytoma and Warthin tumour on cytology. We present a case of a 67-year-old female presented with left parotid gland mass, which was diagnosed as a benign oncocytoma on cytologic examination. Later, the patient underwent left parotidectomy where the histologic examination revealed a malignant oncocytic mucoepidermoid carcinoma. The distinction between these entities is essential to get a proper management for the patient. On cytology alone, it is quite difficult to differentiate; however, histologic examination shows malignant features including infiltrative borders, lymphovascular invasion and perineural invasion excluding a benign tumour. The presence of mucin is an important clue to suspect oncocytic mucoepidermoid carcinoma. Ancillary studies can help reach a wright diagnose, as oncocytic mucoepidermoid carcinoma is positive for P63 and has MAML2 translocation.
INTRODUCTION
Mucoepidermoid carcinoma (MEC) is the most common malignant tumour of salivary glands [1], whereas the majority of cases arise in the parotid gland [2]. However, a set of cases of MEC were reported in other sites such as conjunctiva, lacrimal gland, lacrimal sac, bronchi and thyroid [3]. MEC contains distinguished combinations of squamoid, intermediate and mucus-producing cells [1]. Oncocytic variants MEC (OMEC) is very rare and defined by the existence of >50% oncocytic cells. However, oncocytic metaplasia in MEC is common [1, 3]. Oncocytic change occurs as a result of alteration in mitochondria and appears as enlarged cells with abundant eosinophilic granular cytoplasm [4]. There are several oncocytic lesions of the salivary gland including oncocytosis, oncocytoma, oncocytic carcinoma and some salivary gland tumours that could show oncocytic changes as Warthin tumour, pleomorphic adenoma or acinic cell carcinoma [5]. Oncocytic neoplasm accounts for 1% of parotid neoplasms, where only 11% are malignant [6]. OMEC is challengeable to diagnose, if the typical MEC cells were limited to small foci or absent. Moreover, it could be missed in cytology as in our case which signed out as benign oncocytoma [6]. This case report aims to introduce and apprise both pathologists and clinicians to OMEC, and it is critical to be familiar to this rare entity, which simulate benign tumours.
CASE REPORT
A 67-year-old female presented with a left-sided parotid mass; she went through fine needle aspiration (FNA). Two passes with 25G needle are done and stained with diff-quik. Microscopically, the smear shows a high cellularity with numerous oncocytic cells in large and small groups, whereas no mitosis nor pleomorphism were noted. The case signed out as benign oncocytoma. Eight months later, superficial parotidectomy was done.
Gross appearance: received a parotid gland excision specimen measuring 4 × 4 × 2 cm. Histologically, the tumour shows nests, trabeculae and sheets of oncocytic cells that are separated by strands of desmoplastic stroma with a chronic inflammatory infiltration. Cytologically, the oncocytic cells were round to polygonal, and the nuclei were centrally placed with a prominent nucleoli and an appendant granular eosinophilic cytoplasm with a low nuclear to the cytoplasmic ratio. The majority of tumour was surrounded by a thin fibro-collagenous capsule (Fig.1).
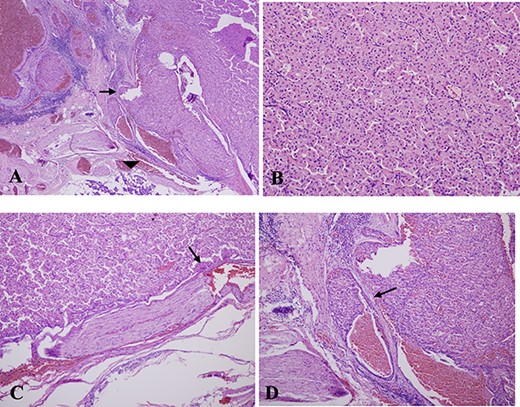
(A) Histologic features of the oncocytic mucoepidermoid carcinoma (arrow) with background normal salivary gland (arrowhead), low-power view. (B) High-power view. (C) Perineural invasion. (D) Vascular invasion. (hematoxylin and eosin-stained slide).
The tumour was positive for CK7, whereas it was negative for S100, CD10, renal cell carcinoma (RCC) marker and c-kit. CK5/6 and P63 show a focal positivity in basal cells only.
Mucicarmine was positive in both the intraluminal secretions and the scattered mucous cells interspersed with the oncocytes (Fig. 2).
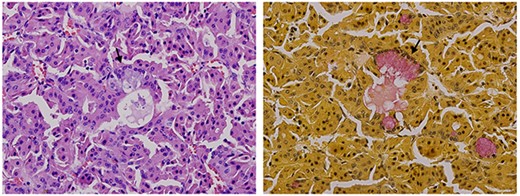
Mucicarmine stain shows the presence of mucous cells within nests of oncocytic cells. (A) Hematoxylin and eosin stained. (B) Mucicarmine stain.
DISCUSSION
MEC is the most common malignant tumour of the salivary gland in all ages [7]. Grossly, it is usually cystic particularly in low-grade cases [7]. Microscopically, it shows three main types of cells: epidermoid cells, mucous cells and intermediate cells, whereas the proportions of these types differ [7]. Moreover, other cell types could be seen in minor or focal proportions as columnar, clear cells and oncocytic cells [7]. In some cases, one type of predominance could be seen [7]. In this case, the diagnose would be the variant of MEC as clear cell MEC or OMEC could be rendered [7]. Furthermore, there is a rare variant described in the literature including: sclerosing MEC, unicystic MEC, sebaceous MEC, psammomatous MEC, spindle cell MEC and goblet cell aggressive MEC [7].
Pathologist can miss OMEC, especially in FNA as there are many oncocytic lesions effecting salivary glands [8]. Mainly, when it is predominant population of oncocytic cells lacking nuclear atypia, mitotic activity or necrosis [8]. Even in histopathologic examination, it would be a challenge to pick it up without a foci or a residual typical MEC [8].
Thus, Brannon and Willard recommend a cutoff at 50% or more oncocytic cells in a tumour with a background of classical histopathological pattern of the MEC to call it OMEC [9].
There is a long list of differentials diagnose, and pathologists can approach first by looking for mucous cells, which will exclude oncocytoma and oncocytic carcinomas [10]. Oncocytic cystadenoma has a characteristic appearance with a multiple cystic structure lined by oncocytic cells and also mucous, epidermoid and intermediate cells can be seen [10].
Warthin’s tumour shows prominent lymphoid tissues that are often accompanied by germinal centres and cystic spaces, which are lined by two layers of columnar cells, and it does not include mucous, epidermoid and intermediate cells [11, 12]. Oncocytic myoepithelioma and myoepithelial carcinomas exhibit features of myoepithelial cells as plasmacytoid and spindle cells [10]. Acinic cell carcinoma displays a characteristic of acinic cells that have a granular and basophilic cytoplasm and eccentric located nuclei [10]. Some metastases can show similar features such as thyroid and adrenal carcinoma [10].
Facing such a situation, a variety of tests can help to distinguish OMEC from other differentials. Mucin can be highlighted by Mucicarmine stain. Moreover, recent studies proved that p63 show diffuse nuclear staining in OMEC, where peripheral staining pattern is noticed in both oncocytoma and oncocytic carcinomas. FISH also can be done for MECT1-MAML2 fusions, as studies shows that MEC has recurrent t(11, 19) (q21; p23) translocation [1, 8]. In general, salivary gland tumours are managed depending on several factors [13]. In case of benign tumour and low-grade MEC stage, T1 and T2 partial superficial parotidectomy is recommended [13]. In high-grade MEC or advanced stages of tumours T3 and T4 cases, at least a superficial parotidectomy with consideration of a total or subtotal parotidectomy should be done [13]. Postoperative radiation is required in patients with high-grade tumours, advanced stages of T3 and T4, positive margins, perineural invasion, lymph node metastases, lymphatic or vascular invasion. Meanwhile, chemotherapy is not routinely used [13]. Patient should be followed up regularly with reducing frequency as time pass from the completion of treatment [13]. In general, MEC has a good prognosis, and OMEC variant does not affect the prognosis [8].
CONCLUSION
MEC rarely exhibits oncocytic cells predominance. Although most of the oncocytic lesions are benign, the pathologist should always exclude the malignant oncocytic tumour as a clinical course and management divers. It may be worthwhile to use ancillary techniques for the differential diagnosis.
CONFLICT OF INTEREST STATEMENT
The authors declare that there are no conflicts of interest regarding the publication of this paper.
FUNDING
None.



