-
PDF
- Split View
-
Views
-
Cite
Cite
Teagan Fink, Siddhartha Deb, Anannya Chakrabarti, Gynaecomastia-like change of a female breast with tri-layer ductal epithelium as described in the male breast, Journal of Surgical Case Reports, Volume 2022, Issue 2, February 2022, rjac032, https://doi.org/10.1093/jscr/rjac032
Close - Share Icon Share
Abstract
A 31-year-old female presented with asymmetrical fullness in the right breast and was found to have a large span of fibrocystic change and nodular glandular tissue on magnetic resonance imaging. Breast malignancy could not be excluded, and thus excisional biopsy was performed. Histopathology revealed a rare finding of gynaecomastia-like histopathological changes of a female breast. Gynaecomastia is traditionally a clinical condition affecting the male breast and characterized by ductal hyperplasia, periductal fibrosis and oedema of the tissue. We describe the first finding of gynaecomastia-like change with a tri-layer ductal epithelium in a female breast, as previously described in the male breast.
INTRODUCTION
Gynaecomastia is a benign clinical condition affecting the male breast, presenting as an enlargement of breast tissue and characterized by ductal hyperplasia, periductal fibrosis and oedema of the tissue. The current definition does not include gynaecomastia-like changes of the female breast. As such, there is a paucity of literature describing the condition in the female population, suggesting the condition may be unrecognized and subsequently underreported. We describe the first finding of gynaecomastia-like change with a tri-layer ductal epithelium in a female breast, as previously described in the male breast. An overview of the literature and remaining research questions is presented, as well as preliminary recommendations for the perioperative management of females diagnosed with gynaecomastia.
CASE REPORT
A gravida 1 para 0 (G1P0) premenopausal 31-year-old female presented with new asymmetrical firmness in the right upper outer breast. She had a history of a bilateral wise pattern breast reduction, took no regular medications and was a nonsmoker. She had a maternal family history of ovarian cancer diagnosed in fifth decade of life. Bilateral breast examination revealed no overlying skin or nipple changes, and a discrete mobile firmness in the right upper outer breast, and no palpable lymphadenopathy. The ultrasound demonstrated increased density and a glandular ridge at 9 O’clock 6 cm from the nipple of the right breast, breast imaging-reporting and data system (BI-RADS) classification score of 3 (Fig. 1A). Mammography demonstrated normal breast tissue (Fig. 1B). Core biopsy was indicative of benign breast tissue with a differential of a breast hamartoma. The patient proceeded to undergo magnetic resonance imaging for further characterization, which showed asymmetric fibrocystic change and nodular glandular tissue with enhancement across a large span (15 mm × 45 mm × 28 mm) on the right lateral breast without a focal lesion (Fig. 2). Breast malignancy could not be excluded, thus the patient proceeded to a diagnostic excisional biopsy. Histopathology revealed a 52 mm span of gynaecomastia-like change of the female breast, with a tri-layered pattern of ductal hyperplasia focally, as has previously been described in male gynaecomastia (Fig. 3) [1]. An underlying aetiology was not found on postoperative serological investigations, and the patient continued with routine breast screening as per local guidelines.
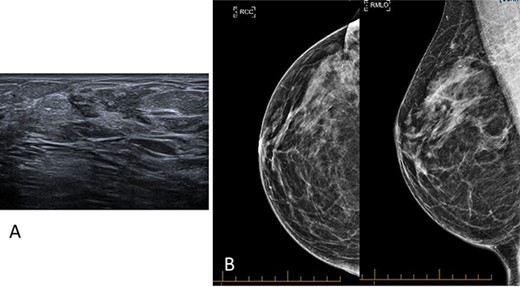
(A) Ultrasound imaging of the right breast highlighting increased density and a glandular ridge at 9 O’clock 6 cm from the nipple, BI-RADS classification score of 3. (B) Mammography imaging of the right breast demonstrating normal breast tissue.
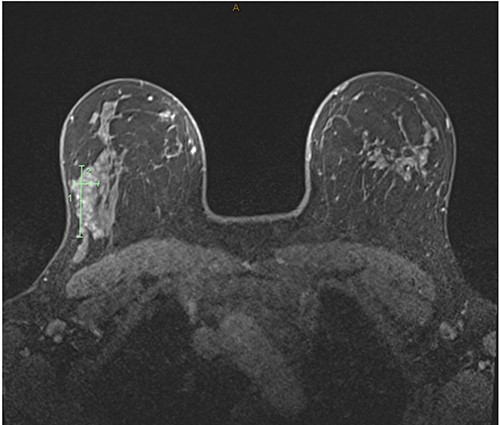
T1-weighted magnetic resonance images of the bilateral breast demonstrating asymmetric fibrocystic change and nodular glandular tissue with enhancement affecting tissue span of 15 mm × 45 mm × 28 mm on the right lateral breast without a focal lesion.
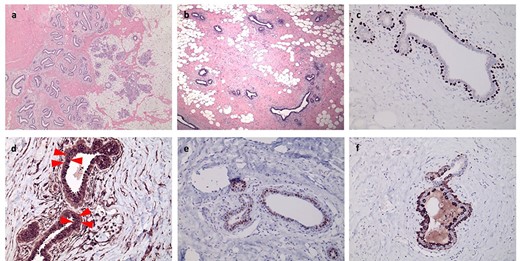
Histological slides and immunohistochemical characterization of gynaecomastia-like change in a female breast, with (a) showing the interface of the lesion with normal breast lobular tissue and (b) typical ducts of gynaecomastia present in the centre of the lesion. (c) p63 shows staining of only basal cells, (d) Bcl-2 staining accentuates an intermediate layer (arrows), which is also highlighted by ER staining (e), whereas CK5 staining is present in both the luminal and basal layers (f).
DISCUSSION
Gynaecomastia-like changes in the female breast have been identified in two retrospective studies of consecutive breast pathological specimens by Umlas et al. (n = 1242) and Kang et al. (n = 2709), who reported an incidence rate of 0.15–0.32% [2, 3]. Patients presented with fullness or mass in the breast, without skin or nipple signs. Age at diagnosis varied from the second to sixth decade of life. Radiological investigations were indeterminant or demonstrated a nonspecific breast or axillary mass.
Gynaecomastia in males is defined as the physiological or pathological enlargement of breast tissue due to an imbalance of androgenic and oestrogenic hormones. In men, aetiology varies from congenital or acquired endocrinopathies, malignancy, extremes of age, organ failure and prescribed or illicit drugs [4]. Histologically, there is stromal and epithelial ductal hyperplasia. Recent studies have demonstrated a tri-layer finding of a myoepithelial basal layer and two epithelial cell layers in a distinctive immunohistochemical staining pattern. The intermediate luminal layer is hormone receptor positive and Bcl-2 and cyclin D1 positive. The inner luminal layer expresses CK5 and CK14, and is hormone receptors and Bcl-2 negative [1].
Few studies have attempted to look for similar patterns in the female breast [5] and gynaecomastia-like change is thought to occur within the spectrum of fibrocystic change. Typical histological characteristics include ductal hyperplasia, oedema and periductal stromal fibrosis – with some contention regarding the significance of terminal duct lobular free areas. This case also demonstrated ductal hyperplasia with periductal stromal fibrosis and myxoid changes across a large area, along with the tri-layered epithelium staining seen in men (Fig. 3).
Cases of breast cancer arising in males with gynaecomastia have rarely been seen, yet a sound understanding of whether gynaecomastia contributes as a precursor for breast cancer is lacking [1]. Female patients presenting with a breast lump or fullness require rigorous workup to exclude a breast malignancy given this is a significant and more common pathology in women compared with gynaecomastia [1]. Evidence-based guidelines for management of gynaecomastia in males are thus insufficient for female patients, as surgical excision is often required to confidently exclude a breast malignancy [6]. If gynaecomastia-like change is demonstrated in a female breast, we would recommend a diagnostic work up to include serological screening (testosterone, oestrogen, luteinizing hormone, follicle stimulating hormone, live function, electrolytes and renal function, thyroid function and serum human chorionic gonadotrophic hormone) and a medication review as outlined by Narula et al. These investigations will determine underlying pathophysiological, pharmacological or malignant causes for gynaecomastia [4].
CONCLUSION
We describe the first finding of gynaecomastia-like change with a tri-layer ductal epithelium in a female breast, as previously described in the male breast. We believe this may represent a distinct cellular compartment more akin to male breast tissue that may show similar hyperplasia due to oestrogen effect as is seen in men. This clinical entity can present as a palpable mass or radiological lesion in a female breast, and thus patients may undergo extensive work up to confidently exclude a breast malignancy for a benign breast condition. Surgeons may need to perform a diagnostic excisional biopsy and serological investigations to exclude pathological causes of gynaecomastia. With little published data on gynaecomastia-like change of a female breast, larger studies are required to develop evidence-based management guidelines of this rare clinical entity.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.
INFORMED CONSENT
Authors have obtained written informed consent from the patient for this case report, and ethics approval from our institute (Epworth Healthcare Reference Number EH2021–710).



