-
PDF
- Split View
-
Views
-
Cite
Cite
Catherine Hall, Mairi McLaren, Charles Mosse, A pancreatic mass and extreme elevation of CA 19–9: a benign masquerade of cholangiocarcinoma, Journal of Surgical Case Reports, Volume 2022, Issue 2, February 2022, rjac018, https://doi.org/10.1093/jscr/rjac018
Close - Share Icon Share
Abstract
Carbohydrate antigen 19–9 (CA 19–9) is a specific tumour marker for pancreato-biliary malignancy. Immunoglobulin G4-related disease (IgG4-RD) is an immune-mediated condition in which IgG4 deposits infiltrate various organs, including the biliary tract manifesting IgG4 sclerosing cholangitis and pseudotumours. An 83-year-old woman presented with severe obstructive jaundice, weight loss and an extreme elevation of CA 19–9 level of 3295 kU/L. Magnetic resonance cholangiopancreatography (MRCP) revealed a pancreatic mass amputating the biliary tree. Liver function tests revealed a cholestatic pattern and severe hyperbilirubinaemia (289umol/L). IgG4 level was found to be high at 7.97 g/L. After treatment with high-dose corticosteroids, repeat MRCP 2 months later revealed disappearance of the pancreatic mass. There was also normalization of the bilirubin and a dramatic decrease of CA 19–9. This case reports the highest published benign elevation of Ca19.9 level in the setting of IgG4 disease. Differentiation between cholangiocarcinoma and IgG4-RD is important, as the treatment is vastly different.
INTRODUCTION
Carbohydrate antigen 19–9 (CA 19–9) is a tumour marker that may be elevated in patients with pancreatic and biliary malignancy [1, 2]. CA 19–9 is a tetrasaccharide secreted by normal pancreatic parenchyma and the biliary tract [1, 2] The upper limit of normal CA 19–9 is 37 U/ml and specificity is ~90% and sensitivity is 80% for diagnosis of a malignancy [3]. However, it is not used as a screening test for malignancy as its positive predictive value is <1% and 5–10% of the population; those who are Lewis-null blood type are unable to produce the antigen [1]. As CA 19–9 titres approach 1000 U/ml, the specificity for pancreatic cancer approaches 100% [1].
Immunoglobulin G4-related disease (IgG4-RD) is an immune-mediated condition in which IgG4 histopathologic deposits infiltrate various organs [4, 5]. IgG4 sclerosing cholangitis and associated biliary pseudotumours are recently described disease processes [4, 6]. A large cohort study, recognized by The American College of Rheumatology and European League Against Rheumatology, found that there are four subgroups of IgG4-RD: hepatopancreatobiliary disease (31%), retroperitoneal fibrosis and/or aortitis (24%), head and neck disease (24%) and Mikulicz syndrome (lacrimal and parotid gland enlargement) with systemic involvement (22%) [5].
Pseudotumours associated with IgG4-RD are occasionally misdiagnosed as cholangiocarcinoma [4]. Differentiation between the two, though difficult, is extremely important due to the vastly different treatment course and the morbidity associated with resection of biliary tumours. This is the dilemma we faced.
CASE REPORT
An 83-year-old woman was referred to our hospital for investigation of a 10-day history of obstructive jaundice, lethargy and weight loss. An abdominal computed tomography (CT) found a complete obstruction of the mid common bile duct (CBD) (Fig. 1), as well as multiple intrahepatic biliary strictures, an enlarged pancreas and multiple hypodense wedge-shaped lesions in both kidneys. IgG4-RD was suggested as a unifying diagnosis of these findings, but cholangiocarcinoma could not be ruled out.

CT abdomen—complete obstruction of mid-CBD, intra and extrahepatic biliary duct dilatation; no obstructing lesion identified; enlarged pancreas with abnormal enhancement and hypodense rind; diffuse hypodense wedge-shaped lesions in bilateral kidneys.
Liver function tests (LFTs) showed a greatly elevated bilirubin of 289 umol/L, with globally elevated alanine aminotransferase (ALT) 179 U/L, alkaline phosphatase (ALP) 400 U/L and gamma-glutamyl transferase (GGT) 593 U/L. IgG4 was 7.97 g/L, which is seven times normal (reference range 0.04–0.86 g/L). The tumour marker Ca19.9 was significantly elevated at 3295 kU/L (normal <34 kU/L). A magnetic resonance cholangiopancreatography (MRCP) revealed a soft tissue mass at the head of the pancreas, amputating the biliary tree and highly suspicious for cholangiocarcinoma (Fig. 2). With markedly elevated Ca 19–9 and IgG4 titres, combined with imaging results suspicious for cholangiocarcinoma, we were presented with a diagnostic dilemma: was the mass an inflammatory pseudotumour associated IgG4-RD, a malignancy or both?
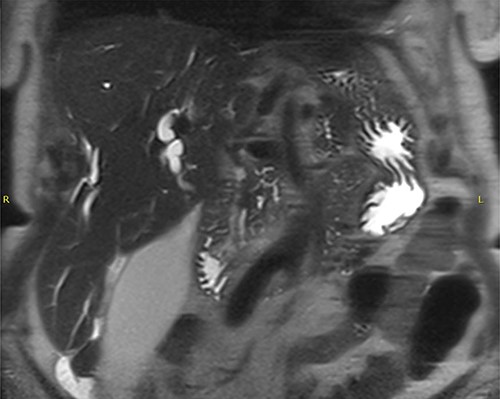
MRCP + pancreas—dilated intrahepatic biliary ducts and common bile duct with abrupt cut-off due to presence of a soft tissue mass highly suspicious for a cholangiocarcinoma; multifocal areas of heterogeneous signal and restricted diffusion in both kidneys may relate to IgG4 disease.
An endoscopic retrograde cholangiopancreatography (ERCP) was done with the intention of placing a stent to relieve biliary obstruction as well as provide an opportunity for brushings or biopsy. No obvious luminal malignant mass was visualized, and stents were unable to be placed due to complete CBD obstruction. Brushings taken at ERCP did not reveal any malignant cells. From here, a fluorodeoxyglucose positron emission tomography (FDG PET) scan was done. This showed focal uptake in the pancreatic head near the area of biliary amputation, as well as uptake in the thickened pancreas, arteries including the aorta and branching vascular uptake in the right lobe of the liver (Fig. 3). Again, an inflammatory disease such as IgG4-RD could account for this picture, but a primary neoplastic process around the head of the pancreas remained of concern.
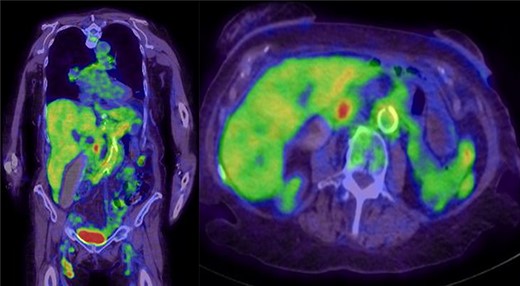
PET-CT whole body—focal increased uptake in the pancreatic head near the region of biliary tree amputation; increased heterogeneous uptake in the pancreas and kidneys; branching uptake in the right liver lobe suggesting vasculitis; extensive thoracic and abdominal aortic uptake indicating arteritis; other findings included prominent nodes with uptake in mediastinum, bilateral inguinal and external iliac.
An immunology consultation was sought, and our patient was commenced on a high dose of IV methylprednisolone. Within 5 days her bilirubin had dropped to 74 umol/L, GGT remained a similar level at 510 U/L and ALP had dropped to 226 U/L. Six days after initiation of steroids her IgG4 level was 6.00 g/L (from 7.97 g/L). Improvement was so rapid and sustained that our patient went home on oral prednisolone, which was weaned down to a maintenance dose of 12.5 mg with weekly methotrexate.
Our patient returned for surveillance investigations 2 months after initiating steroid treatment. A repeat MRCP showed complete disappearance of the CBD mass and resolution of the intra and extra hepatic biliary duct obstruction. Bilirubin was normal at 10, IgG4 was 2.44 and Ca19.9 level was 50 kU/L. A repeat FDG PET scan showed striking interval resolution of FDG avid changes involving the pancreas, liver, kidneys and vessels.
DISCUSSION
A preoperative histological diagnosis is not always a prerequisite for major surgery for lesions suspicious of cholangiocarcinoma [3, 7]. Obtaining a tissue sample can prove difficult and sensitivity of a histopathological diagnosis on biopsy is low [7, 8]. Therefore, lesions suspected to be cholangiocarcinoma are often clinically diagnosed based on a constellation of factors including findings on imaging, clinical history, biochemical findings including CA 19–9 and cholestatic patterns on LFTs [3, 7–10]. Studies have found that between 8 and 24% of resected lesions clinically diagnosed as cholangiocarcinoma were found to be benign [1, 2]. An underlying process of IgG4 disease further complicates the decision-making for the surgeon.
One large study reported that cut-off values for IgG4 and Ca 19.9 can aid in the distinction of pancreatic IgG4-RD from pancreatic cancer [11]. The combination of IgG4 level >280 mg/dl and Ca19–9 < 85.0 U/ml had the best diagnostic accuracy (85.6%) in determining whether the patient was suffering from IgG4 pancreatitis rather than pancreatic cancer [11]. Another study found that IgG4 levels greater than two times upper limit of normal were more specific for IgG4-RD rather than pancreatic cancer [12]. The same study also found that a small minority of patients with pancreatic cancer and the normal population also have IgG4 elevation [12]. To further complicate matters, several studies report pancreatic cancer co-existing with IgG4-RD [12–15]. The possibility of IgG4-RD as a paraneoplastic syndrome in the setting of malignancies has also been raised [12, 13].
IgG4 disease causing biliary obstruction with CA 19–9 elevation is a diagnostic dilemma. Though an obstructed biliary system can elevate CA 19–9 levels, a CA 19–9 of over 3000 kU/L was unparalleled in current literature for similar presentations. Our patient illustrates that IgG4-RD inflammatory pseudotumours can significantly elevate CA 19–9. Steroid treatment should resolve the biliary obstruction and greatly reduce the CA 19–9 in the absence of cholangiocarcinoma.
CONFLICT OF INTEREST STATEMENT
The authors have no conflicts of interests to declare that are relevant to the content of this article.
References
- adrenal corticosteroids
- bilirubin
- weight reduction
- cancer
- carbohydrates
- cholangiocarcinoma
- cholestasis
- glucocorticoids
- hyperbilirubinemia
- antigens
- biliary tract
- sclerosing cholangitis
- kuwait
- liver function tests
- pancreatic neoplasms
- mineralocorticoids
- magnetic resonance cholangiopancreatography
- tumor marker
- pseudotumor
- jaundice, obstructive
- infiltrates
- immunoglobulin g4
- immunoglobulin g4-related disease



