-
PDF
- Split View
-
Views
-
Cite
Cite
Christopher Shean, Janaka Balasooriya, James Fergusson, Low-grade appendiceal mucinous neoplasm (LAMN) as a mimicker of perforated diverticulitis: a case report, Journal of Surgical Case Reports, Volume 2022, Issue 2, February 2022, rjac014, https://doi.org/10.1093/jscr/rjac014
Close - Share Icon Share
Abstract
The differential diagnosis of abdominal pain is wide as both benign and malignant pathologies must be considered. There are currently no published case reports of low-grade appendiceal mucinous neoplasms (LAMNs) mimicking perforated diverticulitis. LAMNs are a heterogenous group of tumours, with no consensus treatment algorithm based on stage and histology. In this case report, we discuss a patient who presented emergently with generalized peritonism, with a diagnosis of perforated diverticulitis made on computed tomography scan. At laparotomy, a perforated appendix was identified, with histopathology identifying a perforated LAMN. This case highlights the importance of considering this rare but increasing incidence tumour when operative management is being planned.
INTRODUCTION
The differential diagnosis of abdominal pain must include both benign and malignant causes [1], with diagnosis achieved through history, examination, and adjuncts including biochemical markers and imaging [2]. Computed tomography (CT) is the imaging modality of choice in patients presenting with generalized peritonism [3], but comes with radiation exposure, which can be of concern in younger patients.
Low-grade appendiceal mucinous neoplasms (LAMN) are a heterogenous group of tumours that are rare but have a rising incidence, with treatment differing significantly based on stage and histology [4]. However, there is no current consensus guideline for the classification and treatment of appendiceal mucinous neoplasms [4]. Although there have been published reports of ruptured appendiceal diverticula mimicking LAMN [5], as well as LAMN being diagnosed in a presumed pelvic mass [6], there are no published reports of perforated LAMN as a mimicker of diverticulitis in a patient with generalized peritonism. Although rare, LAMNs are considered a significant clinical entity as perforation or positive resection margin leaving residual tumour can lead to the development of pseudomyxoma peritonei (PMP) [7]. A small case series showed no long-term recurrence after laparoscopic resection for non-perforated LAMN, with recurrence occurring in one patient that had perforation [8]. Examination of pathological specimens concluded that the involvement of neoplastic cells at the surgical margin did not necessarily lead to PMP, and also that a clear margin did not necessarily prevent PMP from developing [9]. The case presented here highlights the importance of considering this rare but increasing incidence tumour when intra-operative diagnosis is different to the entity anticipated based on pre-operative CT.
CASE
A 51-year-old male presented with 2 days of generalized abdominal pain and profuse watery stools. The pain commenced suddenly and had worsened, becoming so severe the patient was unable to mobilize. The patient’s background medical history consisted only of a supraumbilical hernia repair with mesh 6 years prior, with one colonoscopy 5 years prior completed due to a family history of bowel cancer, which identified a benign polyp. The patient denied any diverticula identified at that colonoscopy. A CT was obtained at presentation that identified a large volume of free gas and free fluid with concern for sigmoid diverticulum perforation (see Figs 1 and 2). At presentation, the patient was haemodynamically stable but had generalized peritonism on abdominal examination. Given the CT and examination findings, an exploratory laparotomy was organized.
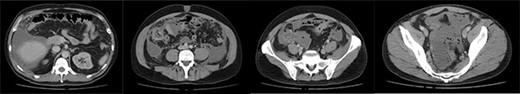
Axial slices of computed tomography scan showing a large volume of free fluid and free gas, with multiple sigmoid diverticula, reported as concerning for perforated sigmoid diverticula.
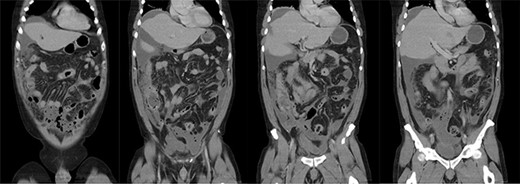
Coronal slices of computed tomography scan showing a large volume of free fluid and free gas, with multiple sigmoid diverticula, reported as concerning for perforated sigmoid diverticula.
A midline laparotomy was performed which identified gross four-quadrant purulent peritonitis with enteric content. In addition to this, widespread gelatinous deposits were encountered, with the main focus identified in the right iliac fossa (see Fig. 3). Biopsies of these gelatinous deposits were taken for histopathological examination. The sigmoid colon was thought to be thickened, but macroscopically normal. A dilated and thickened appendix with perforation was identified, but neither wide base nor associated caecal mass was seen. Thorough examination of the remainder of the abdomen was undertaken, which identified the liver and the remainder of the bowel to be unremarkable. An appendicectomy was performed, with the caecum appearing normal. The base of the appendix was transfixed with vicryl sutures. The intra-peritoneal free fluid and gelatinous deposits were washed out thoroughly after this.

Intra-operative photo taken at the time of laparotomy showing gelatinous deposits.
Histopathology identified a ruptured appendix with a LAMN and associated inflammation, abnormal epithelium transected at the surgical margin, and extravasated acellular mucin involving the peritoneum. This was histologically staged as a pT4a PM1a tumour.
The patient had an ileus and an acute kidney injury that resolved over 1 week. After this, he was discharged home. At review 2 months later, the patient was well and had returned to full work duties with no further issues. Repeat CT scan at this time did not identify any significant peritoneal metastases. Given the diagnosis of ruptured LAMN and the concern for PMP in the future, the patient was referred to a sub-speciality institution for ongoing management. It was determined that the patient does have a risk of developing PMP and that progress tumour markers and follow-up CT scan was to be performed in another 6-month time.
DISCUSSION
LAMN is a rare malignancy accounting for 1% of gastrointestinal neoplasms and is found in less than 0.3% of appendicectomy specimens [10, 11]. In this case, it is unclear whether free acellular mucin was due to acute perforation of the LAMN, or from longstanding spread. Because of the suspicion of a mucinous tumour given the gelatinous deposits, thorough irrigation within the abdomen was completed to minimize the risk of tumour cell implantation. There is limited and mixed evidence surrounding the increased risk of PMP after the perforation of LAMN [9], suggesting that there are additional factors above surgical resection and perforation affecting the risk of developing PMP. The patient was referred to a specialist peritonectomy unit for consideration of further management, with conservative management consisting of ongoing surveillance suggested at this time.
Although perforation is a known complication of LAMN, there are currently no published case reports that have described a patient presenting with generalized peritonitis with CT suggesting of perforated diverticulitis, subsequently found to be due to perforation of LAMN with features of appendicitis. This case highlights the importance of considering this rare but increasing in incidence pathology when forming a differential diagnosis for abdominal pain in general, as well as for surgical planning for patients with an acute abdomen. This case emphasizes the importance of considering LAMN in surgical management where the intra-operative diagnosis does not match the diagnosis made pre-operatively. This highlights the high yield of thoroughly inspecting the remaining colon, small bowel and other organs when a presumed CT diagnosis such as perforated diverticulitis does not match the findings identified in the operating theatre.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
The case report did not receive any funding.
CONSENT
Informed written consent was obtained from the patient that allowed for publishing of the patient history, case details and relevant imaging.



