-
PDF
- Split View
-
Views
-
Cite
Cite
Tong Li, Peng Hao, Xiaojing Lv, Hui Tian, Treatment of a rare recurrent pulmonary arteriovenous malformation after multiple embolization by robotic-assisted thoracoscopic surgery, Journal of Surgical Case Reports, Volume 2022, Issue 2, February 2022, rjac006, https://doi.org/10.1093/jscr/rjac006
Close - Share Icon Share
Abstract
Pulmonary arteriovenous malformations (PAVMs) are a rare pulmonary arteriovenous direct traffic vascular malformation, which directly connect the pulmonary artery to the pulmonary vein without pulmonary capillary bed. Currently, surgical resection and percutaneous transcatheter embolization are the main mode of treatment. Embolization is gradually becoming the preferred treatment for people with PAVMs, because it is less invasive and easy to repeat. We describe a case of PAVMs with hemoptysis that relapsed again after three times of embolization and then only presented new symptoms of transient ischemic attack. Finally, the patient was treated by Da Vinci robotic-assisted thoracoscopic surgery, and there were no obvious post-operative complications and recurrence. It is the first report of multiple recurrent complex PAVMs and we present our experience with the treatment of recurrent PAVMs.
INTRODUCTION
Pulmonary arteriovenous malformations (PAVMs) are rare pulmonary arteriovenous direct traffic vascular malformations. The incidence of PAVMs is about 2–3 per 100 000 patients and it is currently advocated patients with feeding arteries ≥3 mm in diameter which should be treated actively to improve hypoxia symptoms and avoid complications. To date, there are two treatments of PAVMs: intervention and surgery. The indication of surgery in recurrent complex PAVMs remains to be discussed.
CASE REPORT
A 44-year-old man presented with hemoptysis and was diagnosed with PAVMs by computed tomography (CT) 3 years ago. In the past 2 years, the patient accepted three times right pulmonary artery branch embolization. But he appeared the same symptom and CT indicated the recurrence of PAVMs only 1 month later after each operation (Fig. 1). Not long after the third intervention, the patient was admitted to the neurology department for paroxysmal numbness and weakness of all limbs and diagnosed as TIA.
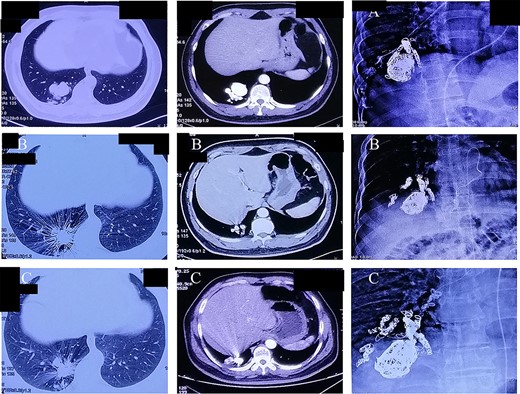
(A–C) Chest computer tomography and angiography on three times of pulmonary artery branch embolization.
His vital signs were within normal range and oxygen saturation was 98%. But we observed that he had clubbed fingers. Lung auscultation, cardiac examination and brain MRI were unremarkable. The transcranial doppler indicated the presence of right–left shunt. On CT and 3D reconstruction, a dilated and tortuous vessel structure and many coils in the right lower lobe were found (Fig. 2). The patient had no relevant HHT history or family history. The diagnosis was considered as idiopathic recurrent PAVMs and secondary TIA resulting from paradoxical embolization. Then, the patient was transferred to the department of thoracic surgery. A large number of malformed vessels and embolic coils were distributed throughout the right lower lobe, so it was difficult to complete resection only using video-assisted thoracoscopic lobectomy. After thorough discussion, we decided to excise the right lower lobe by Da Vinci robotic-assisted thoracoscopic surgery to completely solve PAVMs, and meanwhile, we could remove the steel ring of previous embolization, so as to avoid complications such as ectopic embolization.
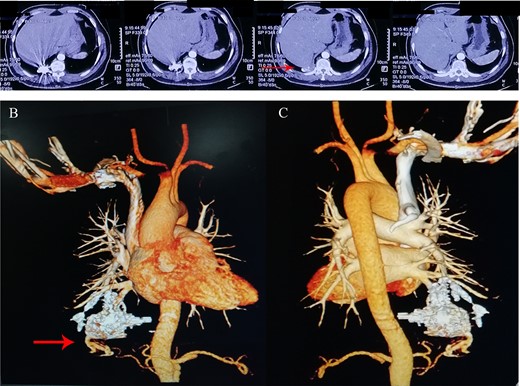
(A) A round density and local artifacts were observed in the lower lobe of the right lung on pre-operative computerized tomography; (B) anterior and (C) posterior 3D reconstruction showed a dilated and tortuous vessel structure in the right lower lobe.
A 4-cm assistive incision was made in the third intercostal anterior-axillary space, and two other instrument arm operation ports were made in the sixth and eighth costal of the front axillary line. The camera port was made in the seventh costal of the midaxillary line (Fig. 3). The first step is releasing the inferior pulmonary ligament and pleuropulmonary adhesions. And then, the inferior lobe vein, the branch of the pulmonary artery and the bronchus of the right lower lobe were clamped in turn by using staplers. The right lower lobe finally was removed. The pathological specimen showed a large number of abnormally tortuous vascular masses and spring coils located on the distal side of the right lower lobe after the operation (Fig. 3). The patient’s symptom disappeared after surgery, and there were no obvious post-operative complications. He was discharged 5 days after surgery. Three months later after the operation, post-operative review of chest CT showed no recrudescence.
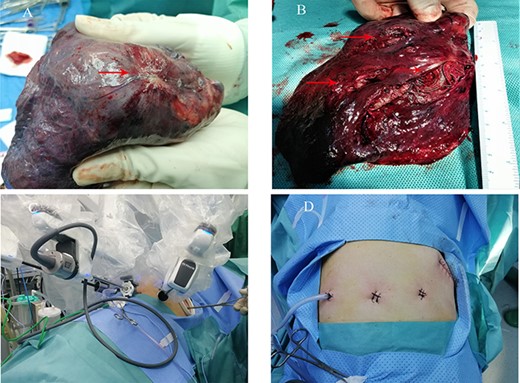
(A and B) The pathological specimen showed a large number of abnormally tortuous vascular masses and spring coils located on the distal side of the right lower lobe after the operation; (C and D) the location of a 4-cm assistive incision, two other instrument arm operation ports and a camera port on the lateral chest wall.
DISCUSSION
It is the first study to report a patient with recurrent PAVM who had received vascular embolization for three times in the past and still had recurrence. According to the literature, the incidence of recanalization or collateral circulation in patients with PAVMs after embolization is up to 20% because of the presence of unrecognized additional feeding arteries in the intervention [1]. Nevertheless, repetitive interventions may increase the incidence of embolization complications such as vascular recanalization, establishment of collateral circulation and down-stream migration of the device [2]. And some researchers believe that patients with repeated imaging procedures and therapeutic interventions can result in levels of radiation exposure that would be classified as harmful [3, 4]. Therefore, whether patients of recurrent PAVMs can benefit from multiple interventions remains to be debate.
The patient was treated by Da Vinci robotic-assisted thoracoscopic surgery to cure recurrent PAVM. Until now, there are no randomized controlled trials or reviews to compare interventional embolization and minimally invasive thoracic surgery, even Da Vinci robotic-assisted thoracoscopic surgery. Due to the great trauma and numerous intra-operative and post-operative complications of traditional open surgery, intervention with less invasive had been the first choice to treat PAVMs since the 1980s, and open surgery had only been used as a supplement to PAVMs which are not amenable to embolization or an emergency surgery to control hemorrhage [5, 6]. With the development of minimally invasive techniques, video-assisted thoracoscopy and even Da Vinci robotic-assisted thoracoscopic surgery have been proven to be safe and feasible, which can significantly reduce the damage to patients [7]. Research shows that the Da Vinci robot surgery is less invasive to patients and has fewer intra-operative and post-operative complications than video-assisted thoracoscopic surgery [7]. What is more, the influence of blood vessel variation, peripheral inflammation and adhesion in recurrent PAVMs may increase the risk of surgery and extreme blood loss. The Da Vinci robot, with its flexible manipulator arm and 3D surgical field, has a huge advantage in tackling these problems [8]. Therefore, we think that local excision, segmentectomy or lobectomy by using Da Vinci robot is a safe method for recurrent and complex PAVMs.
CONCLUSION
The patient of recurrent PAVMs after multiple embolization will benefit from introduced surgery earlier. And robotic-assisted thoracoscopic surgery may be a more thorough and effective treatment.
CONFLICT OF INTEREST STATEMENT
All authors have no conflicts of interest to declare.
FUNDING
None.
REFERENCES
Contegiacomo A, Del Ciello A, Rella R, Attempati N, Coppolino D, Larici AR, et al.
Andersen PE, Duvnjak S, Gerke O, Kjeldsen AD.
Shovlin CL, Condliffe R, Donaldson JW, Kiely DG, Wort SJ, British Thoracic S.
Kneuertz PJ, Singer E, D’Souza DM, Abdel-Rasoul M, Moffatt-Bruce SD, Merritt RE.
Kent MS, Hartwig MG, Vallières E, Abbas AE, Cerfolio RJ, Dylewski MR, et al.



