-
PDF
- Split View
-
Views
-
Cite
Cite
Saima Wase, Kilee Bayne, Mark Billy, Incidental finding of mandibular ossifying fibroma with parasymphyseal mandibular fracture, Journal of Surgical Case Reports, Volume 2022, Issue 2, February 2022, rjab638, https://doi.org/10.1093/jscr/rjab638
Close - Share Icon Share
Abstract
We present an interesting case of a young male with incidental finding of a mandibular ossifying fibroma. The patient sustained direct trauma to the mandible which prompted a computer tomography (CT) scan evaluation of the facial bones. The CT scan showed bilateral mandibular fractures with one of the fractures extending through an incidental finding of a 2.3 cm mandibular parasymphyseal lesion. The patient was previously asymptomatic without dental pain, jaw pain or swelling. This case is unique in the fact that the patient has an inherently rare tumor, was asymptomatic prior to his injury, demographically young for the presentation of this size tumor, and highlights the importance of a through trauma workup.
INTRODUCTION
Ossifying fibromas are the most common type of fibro-osseous lesions. They commonly affect the mandible, in the third to fourth decade of life, with a high predilection for female gender. There are very few reports that note ossifying fibromas identified as a pathologic fracture.
A common presentation of ossifying fibroma is painless swelling of the jaw region. Therefore, they are easy to miss. If left untreated, these fibromas will continue to grow, becoming potentially disfiguring, and require a larger operation. We present a case of an incidental finding of ossifying fibroma with pathologic fracture, outside of typical demographics, that complicate trauma workup and treatment.
CASE REPORT
We present a case of a 20-year-old African American male with medical history of asthma who presents for evaluation of facial trauma. Patient was involved in an altercation sustaining direct trauma to the mandible and presented to the emergency department for evaluation of jaw pain. Prior to the altercation, patient denied dental, facial or neck mass issues. On clinical exam, he had tenderness and swelling over the left angle of the mandible as well as right mandibular parasymphysis. Tooth #25 was slightly mobile otherwise all other dentition was intact. He underwent computer tomography (CT) scan of the facial bones, which showed a non-displaced left mandibular angle fracture, a non-displaced right mandibular parasymphyseal fracture extending through a 2.3 cm expansile well-defined partially sclerotic lesion, as shown in Fig. 1. The lesion was core biopsied resulting as an ossifying fibroma. The patient was offered segmental resection with reconstructive options of osseous flap. The patient refused free flap reconstruction and elected for resection with plating technique. The patient then underwent segmental mandibulectomy of the tumor with large titanium plate reconstruction as well as open reduction internal fixation of the left mandibular angle fracture, as shown in Fig. 2. The final pathology resulted as central ossifying fibroma. The patient healed well without post-operative complications.
DISCUSSION
Fibro-osseous lesions include fibrous dysplasia, osseous dysplasia and ossifying fibromas. Ossifying fibromas are the most common type of fibro-osseous lesions [1]. Ossifying fibromas are rare benign neoplasms [2, 3] derived from mesenchymal blast cells of the periodontal ligament [4]. The pathophysiology of ossifying fibromas involves fibrous tissue replacing normal bone [3]. Histopathology demonstrates hypercellular fibrous connective tissue stroma with variable calcifications [5].
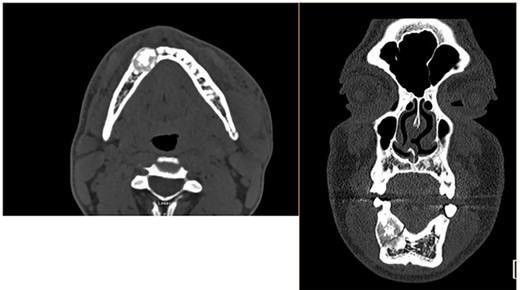
CT scan of the facial bones. These CT images in the axial (left) and coronal (right) view depict the 2.3 cm mandibular mass with pathologic fracture on the medial aspect as well as a non-displaced left mandibular angle fracture.
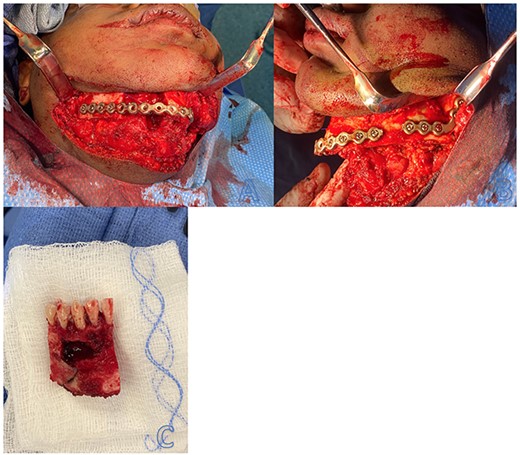
Intraoperative resection and repair of mandibular ossifying fibroma with pathologic fracture. (A) View of right segmental mandibulectomy with reconstruction using titanium reconstruction plate. (B) View of open reduction internal fixation of left mandibular angle fracture with titanium plate. (C) Resected ossifying fibroma.
Ossifying fibromas most commonly affect the mandible in 70–90% of the cases [6]. It typically presents in the third-fourth decade of life with a high predilection for females [7, 8]. The classic manifestation is a painless firm swelling of the jaw [9]. On imaging, it may appear most commonly as radio-opaque (49.2%) followed by mixed radio-opaque-radiolucent (34.9%) and radiolucent lesions (15.9%). Most lesions are unilocular (84.1%) [10]. The neoplasm is potentially aggressive; when left untreated, the dimensions can expand and cause disfiguration. This case presentation of an ossifying fibroma is rare based on the incidental diagnosis following a mandibular fracture in a 20-year-old male patient.
There are multiple modalities of treatment for an ossifying fibroma. These include but are not limited to enucleation or curettage for small lesions and surgical resection for larger lesions. The rate of recurrence following surgery is usually low. Therefore, a conservative approach is preferred for surgical management of ossifying fibromas. To further minimize the rate of recurrence, surgical resection via mandibulectomy should be performed. Surgical resection is followed by repair with a fibular free flap, bone matrix, synthetic bone substitutions, or titanium plates. In this case, our patient underwent segmental mandibulectomy with a reconstructive titanium plate due to the size of the ossifying fibroma in conjunction with right mandibular parasymphyseal fracture through the mass. Ossifying fibromas of the mandible are rare, but treatable when surgically resected and monitored postoperatively.
FUNDING
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.



