-
PDF
- Split View
-
Views
-
Cite
Cite
Hayder Alqaisi, Alkwin Wanders, Gintare Naujokaite, Lasse Pedersen, A huge retroperitoneal cyst with a rare clinical presentation, Journal of Surgical Case Reports, Volume 2022, Issue 12, December 2022, rjac592, https://doi.org/10.1093/jscr/rjac592
Close - Share Icon Share
Abstract
A 39-year-old male presented with deep venous thrombosis in the right lower limb. He had been experiencing increasing abdominal girth over several years, but this went undetected at the initial examination. Eighteen months later, a computed tomography was conducted, showing a huge retroperitoneal cyst (25 × 23 × 16 cm) lifting the right external iliac vessels. Complete surgical excision of the cyst was performed. The cyst was unilocular and contained 5 l of clear fluid. Histopathology examination found a thin cyst wall consisting of fibrous stromal tissue with a single-layer epithelium lining. Immunohistochemical staining revealed positivity for endothelial cell markers, CD31 and CD34, but negativity for the lymphatic marker podoplanin (D2–40), corresponding to a vascular origin, likely a venous malformation.
INTRODUCTION
Retroperitoneal cysts have an estimated incidence of 1/106 400 to 1/250 000 [1]. The retroperitoneal space allows cysts to grow to a considerable size before becoming symptomatic. Symptoms are usually vague and related to abdominal discomfort and increasing abdominal girth. On rare occasions, huge cysts may cause symptoms related to compression of pelvic vessels or ureteres [2, 3].
CASE REPORT
A 39-year-old male presented with right lower-limb swelling and was diagnosed with deep venous thrombosis (DVT). Following local guidelines, anticoagulants were administered. Evaluation for thrombophilia was normal. At diagnosis, he reported increasing abdominal girth, attributing this to unhealthy lifestyle, a symptom which went unnoticed by the examining physician. The patient’s medical history was noteworthy for oesophageal atresia with a tracheoesophageal fistula, which was reconstructed successfully in infancy.
He was referred to the surgical gastroenterology department 18 months after his DVT diagnosis because he felt ‘heavy’ and had a noticeable abdominal size that had developed in the course of several years. Physical examination revealed a dilated abdomen with a palpable hard mass in the lower region. Contrast-enhanced computed tomography (CT) was performed showing a huge thin-walled retroperitoneal, unilocular cystic lesion in the lower part of the abdominal cavity extending from the pubic bone to the aortic bifurcation, measuring 25 × 23 × 16 cm (Fig. 1). The cyst displaced the right side external iliac vessels anteriorly to just below the anterior abdominal wall (Fig. 2). Right-side internal iliac vessels were located under the cyst and left-side vessels had a normal anatomy. Figure 3 shows a 3D reconstruction of the iliac vessels. Varicose veins were described in the pelvic cavity.

Coronal view from an abdominal CT showing the retroperitoneal cyst (arrow on the right side of the figure) and the course of the right external iliac vessels (arrows on the left side of the figure).
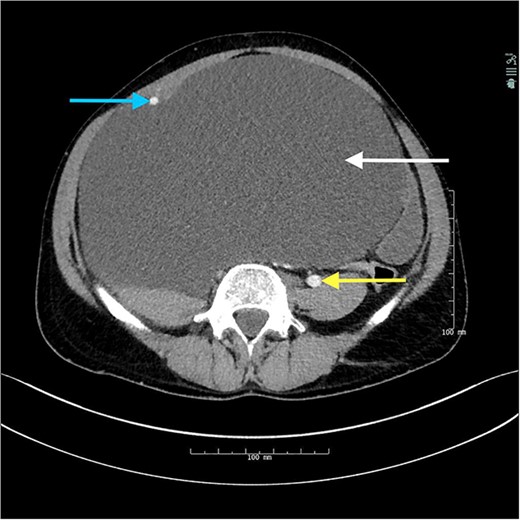
Axial view from abdominal CT showing the retroperitoneal cyst (upper arrow on the right side of the figure) with the displaced right iliac vessels (arrow on the left side of the figure) and the normally positioned left-sided common iliac vessels (lower arrow on the right side of the figure).
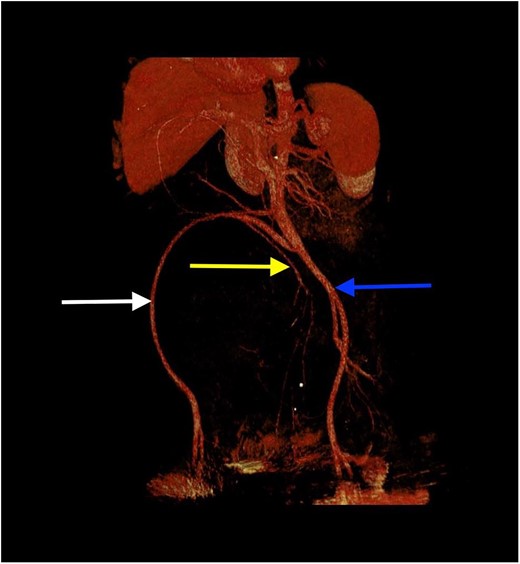
3D reconstruction of the iliac vessels. Right external iliac vessels (arrow on the left side of the figure), right internal iliac vessels (arrow in the middle) and left common iliac vessels (arrow on the right side of the figure).
Complete surgical cyst excision was performed. The cyst ruptured during the procedure, leaking 5 l of clear, serous fluid. The right iliac vessels were adherent to the cyst wall (Fig. 4). The aetiology of the cyst was not identified. Right-sided iliac vessels were closely joined with the cyst wall, and a 5-mm, non-vessel-containing pedicle was ligated adherent to the pubic bone (Fig. 5). The patient recovered well and was discharged 2 days later.
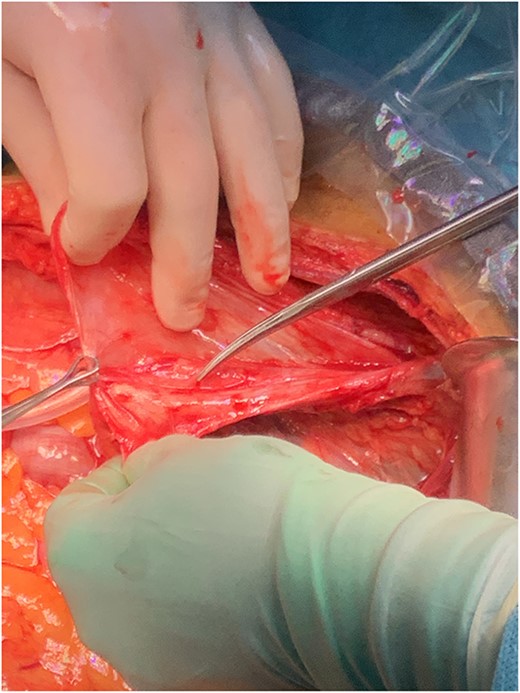
The probe points to the iliac vessels, which were part of the cystic wall (after the cyst had ruptured).
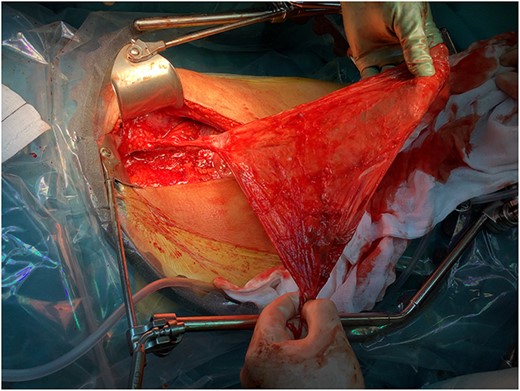
Picture taken immediately before complete surgical excision; the 5-mm pedicle is still adherent to the pubic bone.
Microscopic examination revealed a cyst wall consisting of fibrous stromal tissue with bundles of desmin-positive smooth muscle cells, elastic fibres and tiny capillaries. A single layer of flattened epithelium lined the inner cyst layer. A section of the cyst showed aggregated lymphocytes and plasma cells. Immunohistochemical staining revealed positivity for endothelial cell marker CD31 and CD34. Podoplanin (D2–40) was negative.
DISCUSSION
Classically, DVT is attributed to Virchow’s triad where a blood clot forms due to hypercoagulability, endothelial injury or blood flow stasis [4]. Here, the cyst exerted a lifting/compressing effect on the right iliac vein causing stasis and dilated pelvic veins.
Lower-limb DVT caused by benign retroperitoneal cysts is believed to be extremely rare and—to our knowledge—only one case study related to inferior vena cava compression has previously been reported [3]. Our case shows the importance of a thorough patient history and clinical examination to identify potentially causative factors to DVT. Retroperitoneal cysts may, however, be challenging to diagnose. They can grow to a considerable size, while causing only few symptoms such as abdominal discomfort and a slowly increasing abdominal girth [5]. Other reported symptoms include back pain, weight loss, fever, jaundice or referred lower-limb pain [6].
According to Yang et al., retroperitoneal cystic lesions are commonly classified as either neoplastic or non-neoplasic [7]. Neoplastic lesions relevant to our case include cystic lymphangioma, mucinous cystadenoma, cystic mesothelioma, tailgut cyst, bronchogenic cyst and pseudomyxoma retroperitonea [7]. Non-neoplastic lesions include pancreatic and non-pancreatic pseudocyst, lymphocele, urinoma and haematoma. Unfortunately, our case does not fit these categories due to the type of cyst content and the cyst’s histological manifestation and anatomical location. The negative result for podoplanin (D2–40) excludes a lymphatic origin [8]. A retroperitoneal bronchogenic origin was considered due to the patient’s history of a tracheoesophageal fistula but was excluded because of a lack of glands, cartilage and respiratory epithelium [9]. A vascular origin was also considered. Following the latest classification from the International Society for the Study of Vascular Anomalies (ISSVA), published in 2018, vascular anomalies are classified as vascular tumours or vascular malformations. Vascular malformations are subdivided into capillary, lymphatic, venous or arteriovenous malformations [10]. In our case, the cystic wall was a single layer of endothelial lining with underlying smooth muscle cells and elastic fibres. Endothelial cells presented CD31 and CD34 positivity and D2–40 negativity. In the ISSVA classification, this corresponds to a venous malformation. Venous malformations are congenital, slowly growing defects that may contain different kinds of fluid despite their vascular origin [11].
The preferred treatment for retroperitoneal cysts is excision or enucleation. Smaller, easily accessible cysts may be excised laparoscopically. Other treatment modalities, such as marsupialisation, partial excision or simple drainage, are viable but often less successful options. As noted in a case series by Kurtz et al., partial excision and drainage usually cause recurrence [1]. However, for selected patients unfit for major surgery, these modalities may provide symptom relief. With increasing use of advanced imaging techniques, like CT, magnetic resonance imaging and abdominal ultrasound, the incidence of smaller asymptomatic retroperitoneal cysts is likely to rise. Their management remains a clinical dilemma. Asymptomatic retroperitoneal cysts may never grow to become symptomatic, and surgery within the retroperitoneal space close to major vessels carries an inherent risk of serious complications. Abstaining from surgery may ultimately result in the removal of a large cyst in a more challenging procedure, leaving no material for pathology examination. Furthermore, some retroperitoneal cysts are malignant or have a malignant transformation risk. Since retroperiotoneal cysts are rare, it remains unknown how effective pre-operative imaging is in separating benign from malignant cysts. For retroperitoneal tumours generally (including cysts), small case series have been reported, suggesting that internal homogeneity, fat density, calcification and cyst formation are predictors of a benign tumour, but case series on retroperitoneal cysts alone are unavailable [12]. However, in other cyst types (e.g. ovarian cysts), benign characteristics include a thin, regular wall; a lack of septae; homogenous fluid and a lack of solid components [13]. Asymptomatic retroperitoneal cysts with such characteristics may be considered for a watchful waiting approach.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
No funding was needed.
AUTHORS’ CONTRIBUTIONS
H.A and L.P searched the literature and drafted the manuscript. A.W. revised the manuscript and evaluated the histopathology. G.N. revised the manuscript evaluated the radiology. All authors have read and approved the final manuscript.
DATA AVAILABILITY
The data of this case report are available from the corresponding author upon reasonable request.
CONSENT FOR PUBLICATION
Written consent was obtained from the patient.



