-
PDF
- Split View
-
Views
-
Cite
Cite
Kurt Wiendieck, Arnd Dörfler, Björn Sommer, Extended salvage surgery after high-dose chemoradiation therapy for tumors in the cervico-thoracic junction with invasion of the chest wall and the spine: a case series, Journal of Surgical Case Reports, Volume 2022, Issue 12, December 2022, rjac581, https://doi.org/10.1093/jscr/rjac581
Close - Share Icon Share
Abstract
The treatment of malignant tumors localized in the upper thoracic cavity and involving the spine at the cervico-thoracic junction (CTJ) is challenging. We report on three patients with malignant tumors invading the thoracic inlet and the spine at the CTJ. All three patients underwent radical tumor resection and 360° spine fusion following the posterior pedicle screw instrumentation and anterior vertebrectomy combined with implantation of an expandable titanium cage. Postoperatively, a mild paresis with hypesthesia of the ipsilateral arm occurred in one patient because of brachial plexus involvement. Two patients were still alive at last follow-up after 83 and 143 months, the third patient succumbed to tumor progression 13 months after extended salvage surgery. We display the possibilities of extended ‘salvage’ therapy in well-selected patients that were deemed hopeless regarding neurological function, biomechanical stability and tumor control after multiple courses of combined radio-chemotherapy.
INTRODUCTION
The interdisciplinary treatment of malignant tumors with vertebral invasion in the cervico-thoracic junction (CTJ) is still challenging. Concepts such as the neurologic, oncologic, mechanical and systemic decision framework or the LMNOP framework that considers the Spine Instability Neoplastic Score have been developed to provide general guidance for therapeutical decisions in these patients [1, 2]. In patients with progredient tumor growth or recurrence under first-line therapy, tumor decompression of the spinal cord is the main goal to prevent or regain neurological function and mobility. Starting with pure laminectomies, the stability of the vertebral column has moved into the focus, allowing a 360° decompression with sufficient spinal instrumentation and to provide a maximum capacity of load carrying and thus of the patient mobility [3–5]. This approach is usually accepted in patients after neo-adjuvant treatment but is rarely reported in patients after chemoradiation therapy associated with an application of higher radiation dose. Thus, we present our concept of extended salvage surgery in three patients with local recurrent and/or persistent tumors with vertebral invasion at the CTJ.
CASE SERIES
Case 1
A 54-year-old woman with non-small cell lung cancer (NSCLC) of the right upper lobe associated with deep infiltration of Th1–2 underwent a definitive chemoradiation therapy with the application of 66 Gy into the primary tumor bed from November 2009 until January 2010, followed by palliative-intent chemotherapy according to the persistent residual primary tumor. A PET-CT of February 2012 revealed a slightly increasing of the standardized uptake values to 3.2 mS in initial tumor area without any evidence of distant and lymphogenic metastasis. No neurological deficits besides a hypesthesia of the right medial upper arm and both plantar feet were evident. First, a dorsal osteosynthesis was performed with the placement of polyaxial massa lateralis screws in C5–C7 as well as pedicle screws in Th3 and Th4, which were connected via a rod-system and two cross-connectors (Vertex Reconstruction System, Medtronic). Thereafter, an extended upper bi-lobectomy combined with a radical lymphadenectomy including thoracic wall resection of the first two ribs and partial resection of the third and fourth rib was performed. After Th1–2-vertebrectomy, a distractable cage (Synthes, Johnson & Johnson) was implanted. A cerebrospinal fluid leakage through an accidental durotomy was intraoperative sealed with a fibrin sealant patch (TachoSil, Baxter) without any further cerebrospinal fluid leakage in the postoperative course. Histopathological examination revealed in toto tumor resection combined with the evidence of tumor necrosis (ypT0, ypN0(0/12), L0m V0, Pn0, regression grading 3, local R0). A control CT scan 3 months later showed an asymptomatic dislocation with loosening of the C5 and C6 mass screws. Therefore, a revision and an extended dorsal instrumentation to C4 after correction of C5 and C6 screws combined with the placement of the pedicle screws in C7 were performed. The right C6 screw could not be implanted because of insufficient bone quality. Postoperative CT showed the correct placement of instrumentation. The cervical motion was reduced 10° in every axis. The patient reported on hypesthesia in the right upper chest wall as well as dorso-medial upper arm with a minimal impairment of fine motor skills of the right hand. At last follow-up, no evidence of tumor recurrence or additional neurological deficits were seen after 83 months.
Case 2
This 46-year-old male patient presented with progressive pain and paresthesia of the left arm combined with a partial Horner syndrome based on the affection of the stellate ganglion combined with an anisocoria without any other motoric deficits. CT scan revealed a 4 × 4.6 × 2.3 cm tumor in left upper lobe infiltrating the second and third rib as well as the second thoracic vertebra. The CT-guided tumor biopsy revealed a poorly differentiated NSCLC. A combined high-dose chemoradiation therapy up to 66 Gy with vinorelbine and carboplatin was performed.
Despite the definitive chemoradiation therapy, a locally progressive tumor without evidence of distant metastasis was detected 2 months later in an MRI associated with the infiltration of Th1–3 and invasion of the first and second left thoracic root without evidence of a myelon compression (Figs 1 and 2).

Preoperative sagittal MRI (STIR) image of patient No. 2 depicting active tumor invasion of T1, T2 and T3 as well as pathological hypodense C7 and Th4 vertebral bodies.
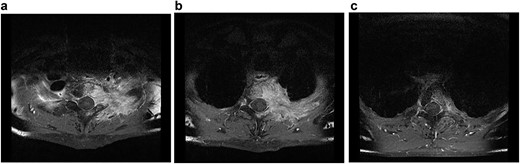
Transversal MRI STIR-images of patient No. 2 with Th1 (a), Th2 (b) and Th3 (c).
Because of a possible treatment-associated pseudo-progression of the tumor, a watch-wait-procedure was chosen in the interdisciplinary tumor conference. Five months later, CT scans showed an oligo-progression with dorsal tumor growth into the spinal canal, destruction of the Th2 vertebra and infiltration of Th1–3 vertebrae with compression of the corresponding left nerve roots still without any evidence of distant metastasis (Fig. 3).
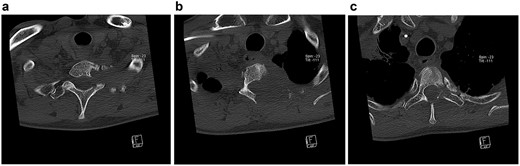
Transversal CT scans of the thoracic. Extent of bony destruction of the left pedicle, costotransverse joint and facet joint of C7/Th1 (a), the left hemilamina, pedicle, costotransverse facet joints, rib and vertebral body of Th2 (b) and hemilamina as well as pedicle of Th3 (c).
An extended left upper lobectomy with chest wall resection of the first three ribs was performed. The brachial plexus was microsurgically dissected. This surgical procedure was complicated by a tension pneumothorax caused because of the lung emphysema on the right side. Surgery was interrupted and a chest drain was inserted without any other complications.
The surgical procedure was completed 5 days later without any complication by decompression of the exiting nerve roots of the first to third thoracic vertebra followed by consequently vertebral resection. After the placement of the distractable vertebral cage, the patient was shifted into the prone position. Then, the fifth cervical to the sixth thoracic vertebra was visualized and further dorsal tumor debulking with removal of the intraspinal mass was performed. Thereafter, lateral mass screws were inserted in C5 and C6. The vertebrae C7, Th4-6 were instrumented using pedicle screws. The rod system was implanted with additive cross-connector insertion (Figs 4 and 5). During the further postoperative course, skin and muscle tissue thinned out, leading to the transfer of a mucocutaneus latissimus dorsi flap over the screws by plastic surgeons 7 months later. Unfortunately, 1 year after the spine surgery, CT scans identified a local tumor recurrence involving C1 to Th6 with the infiltration of the spinal canal and chest wall in the CTJ. The patient suffered from pain in the right shoulder and a paresis of the right hand, which worsened to a mild paresis of the arm. Palliative chemotherapy with carboplatin and etoposide was initiated. The patient died 1 month later because of the further NSCLC progression.

Postoperative sagittal CT scans with 3D-reconstruction after 360° fusion. The vertebral body replacement with a distractable cage, which is displaced anteriorly because of a slight endplate sintering.

Postoperative sagittal CT scans with 3D-reconstruction after 360° fusion. The vertebral body replacement with a distractable cage, which is displaced anteriorly because of a slight endplate sintering.
Case 3
A 45-year-old female patient with a moderately differentiated squamous cervical cancer underwent a percutaneous radiotherapy and interstitial brachytherapy. Four months later, an MRI of the cervical spine revealed pulmonary metastasis with the first three thoracic vertebra invasions. An FDG/PET excluded the evidence of other tumor manifestations and showed osseous destruction of the vertebrae and the surrounding chest wall. The chemoradiation therapy with cisplatin and 5-fluorouracil combined with the application of 45 Gy was performed and accomplished sufficient clinical-radiological tumor response. Therefore, a curative-intent surgical procedure with resection of the first and third rib and wide wedge resection of the right upper lobe combined with Th1–3 vertebrectomy followed by implantation of an expandable cage was performed. Seven days later, postoperative CT scans showed a ventral tilting of the expandable cage, which lead to an uneventful revision surgery. After another 7 days, dorsal instrumentation using pedicle screws from C5–7 to Th5–7 with a cross-connector was performed. Follow-up CT and MRI scans were unremarkable and showed no signs of sintering, loosening of screws or fractures. Fifteen months later, diffuse pulmonary metastases were diagnosed and chemotherapy with topotecan and paclitaxel was initiated. Almost 2 years later, progression of the pulmonary metastasis occurred. Therefore, a treatment with doxorubicin was initiated, which was changed to ifosfamide 3 months later because of a lack of tumor response. Another 5 months later, the patient received high-dose radiation therapy for oligo-persistent pulmonary metastasis in the right lung. At latest follow-up, the patient was tumor free and without any neurological deficits 143 months after extended salvage surgery.
DISCUSSION
The concept of a so-called ‘salvage surgery’ was described in patients with locally advanced NSCLC accomplishing with long-term survival in appropriate patients [6]. The experience in extended salvage surgery still remains very limited. In general, only few patients are deemed suitable for this type of surgery, as invasion of the ribs, vertebral bodies or great vessels are associated with a poor prognosis [7]. Radical tumor resection en bloc with the spinal segments combined with anterior and posterior reconstruction of the spinal column is usually required. However, this procedure is technically demanding especially in extended multilevel approaches [8–10]. The morbidity and mortality rates range from 28 to 56% and from 5 to 10%, respectively [8, 10]. Neurological deficits occur in up to 25% following surgery, and implant failure of spinal instrumentation is reported to be 19% [10]. Because of a paradigm shift, nowadays the extent of spine invasion is no longer a contraindication for radical surgery if complete resection is possible [11]. The completeness of resection determined the postoperative survival and the recurrence-free interval [7, 12, 13]. A recent meta-analysis identified complete (R0) resection as a prognostic marker, whereas induction and adjuvant treatment showed no influence on overall survival rates [11]. Five-year overall survival rates are 22–66% [10] and 10-year overall survival rates are 3–26% after en bloc resection of the lung, chest wall and spine [8, 11].
In our patients, we used the posterior approach introduced during the 1960s by Shaw and Paulson (Shaw–Paulson approach) according to the tumor location in the posterior compartment. Using this technique, up to 50% of the vertebra can be resected without additional stabilization [14–16]. The vertebral body replacement in combination with dorsal spondylodesis is the preferred treatment option to achieve decompression and to restore the spinal column stability. This approach is accepted in patients with a traumatic > A3 AO spine fracture [17, 18] and in cases of pathological instability because of tumor invasion, as well [19].
Local tumor invasion might destabilize the structural integrity of the vertebral body with resulting imbalance of the sagittal profile of the spine, causing pain and neurological deficits. A recent publication on spinal metastases of the CTJ underlines the challenge for biomechanical stabilization after extended surgical resection [20]. Surgical treatment options are mainly palliative and aim for minimal perioperative and postoperative morbidity. However, more radical treatment options with removal of spinal lesions showed better results in carefully selected patients [21–24].
Based on the results of the Southwest Oncology Group Trial 9416 and the Japan CliniCal Oncology Group Trial 9806, the standard treatment for sulcus superior tumors is neoadjuvant induction chemotherapy combined with high-dose radiation followed by radical surgical resection [25, 26]. Recent studies revealed that the initial application of chemotherapy and high-dose radiation followed by ‘en bloc’ resection leads to promising results with 5- and 10-year survival rates of 14–61% and 26.5%, respectively [12, 13, 27, 28], and reported recurrence rates between 41 and 59%. The key prognostic factor for tumor recurrence and survival is a complete, radical tumor resection removing the lesion in one piece surrounded by a continuous layer of macroscopic healthy tissue with tumor-free margins [13]. Since absolute criteria of inoperability of such entities include (i) the involvement of the brachial plexus above the T1 nerve root and (ii) the involvement of more than 50% of the vertebral bodies [8,29], these patients could still be considered for extended salvage therapy under certain circumstances. Complications that are frequently encountered in these patients are paresis of the ipsilateral hand because of T1 nerve root sacrifice, resection of the stellate ganglion and nerve root of C8 causing a Horner syndrome, and cerebrospinal fluid leakage [8]. The overall rate of postoperative complication after extended surgery including resection and stabilization located in the CTJ was 34% with a 18% revision rate [20]. Main reasons were surgical site infections and hematoma.
In summary, patients with tumor progression of invading the chest wall and spine that are at the end of their radio-chemotherapeutic treatment, extended surgery might be a last resort to achieve biomechanical stability patients in the CTJ even though the expected lifetime is limited. Despite high complication rates, an exteded salvage surgery appears to be a feasible alternative to achieve local tumor control in well-selected patients. By this method, further destruction of the vertebral column, damage to the spinal cord and nerve roots could be avoided.
CONFLICT OF INTEREST STATEMENT
The authors state that there are no conflicts of interest regarding this original submission.
FUNDING
None.
DATA AVAILABILITY
The data that support the findings of this study are available on request from the corresponding author, [BS]. The data are not publicly available due to the privacy of research participants.
Portions of this work were presented as a poster presentation at the 132nd Congress of the German Society of Surgery (DGCH) in Munich, Germany, on September 2015.



