-
PDF
- Split View
-
Views
-
Cite
Cite
Jia Xi Julian Li, Ranah Lim, Mark Damien Muhlmann, Laparoscopic Ladd’s procedure: a case report and review of the literature on patient selection for an appropriate surgical approach, Journal of Surgical Case Reports, Volume 2022, Issue 12, December 2022, rjac577, https://doi.org/10.1093/jscr/rjac577
Close - Share Icon Share
Abstract
Intestinal malrotation is a rare condition which is managed surgically with the Ladd’s procedure. We report a case of an adult male presenting with symptomatic intestinal malrotation which was successfully treated with a laparoscopic Ladd’s procedure. While traditionally performed with a laparotomy, the case highlights the emerging evidence in the literature supporting the laparoscopic approach and explores factors affecting patient selection for an appropriate surgical approach.
INTRODUCTION
Intestinal malrotation is a rare condition which is managed surgically with the Ladd’s procedure. While traditionally performed with a laparotomy, there is emerging evidence in the literature supporting the laparoscopic approach. We report a case of an adult male presenting with symptomatic intestinal malrotation who was successfully treated with a laparoscopic Ladd’s procedure and a review of the literature on the laparoscopic Ladd’s procedure, including factors affecting patient selection for an appropriate surgical approach.
CASE REPORT
A 28-year-old male was referred for a review of his severe abdominal pain associated with eating, unintentional weight loss and intermittent vomiting and diarrhoea over several years. His background medical history included a laparoscopic converted to open appendicectomy performed overseas when he was an adolescent. Clinical examination and biochemical investigations were unremarkable. Computed tomography (CT) of the abdomen demonstrated features of intestinal malrotation, with the entirety of the large bowel on the left and the small bowel on the right, without any evidence of acute obstruction (Fig. 1).
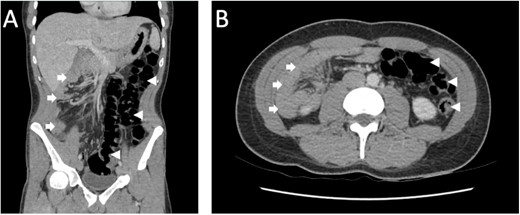
CT abdomen/pelvis in the portal venous phase (A) coronal, (B) axial demonstrating features of intestinal malrotation with the colon (arrowhead) predominantly located on the left and the small bowel (arrow) on the right.
After obtaining an informed consent, the patient proceeded to an elective laparoscopic Ladd’s procedure. Intra-operative findings demonstrated partial malrotation of the intestine, multiple small bowel adhesions to the mesentery, Ladd’s bands running from the right upper quadrant and the lateral aspect of the second part of the duodenum to the caecum and ascending colon, and a caecum positioned towards the epigastrium and the left iliac fossa with adhesions to the sigmoid colon, splenic and hepatic flexures (Fig. 2). The Ladd’s bands were divided, and the terminal ileum, caecum and ascending colon were mobilized off the duodenum. Adhesions to the small bowel and between the colonic flexures, sigmoid and caecum were divided, thereby widening the mesentery. At the end of the procedure, the small and large bowels were placed in a non-rotated position.
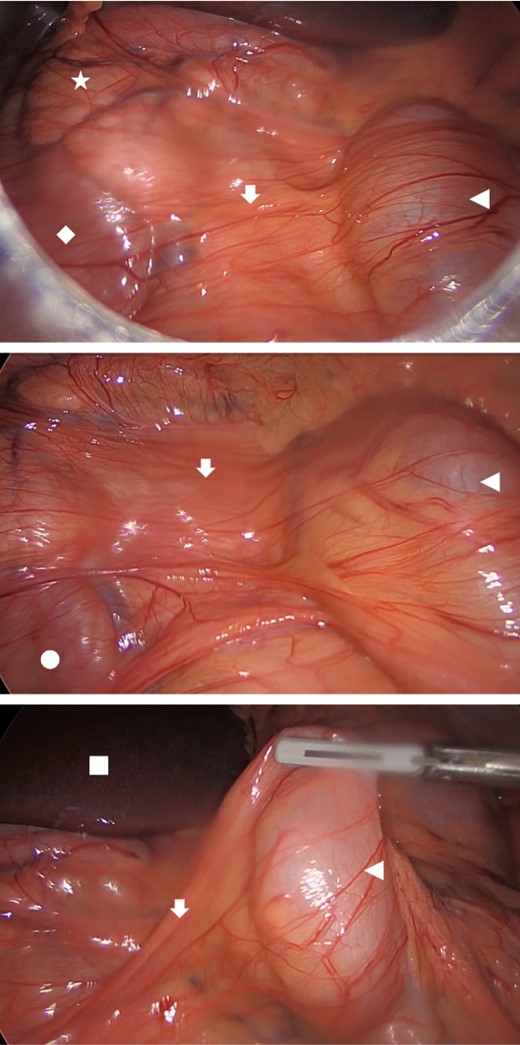
Intra-operative findings demonstrating Ladd’s bands (arrow) attached to the caecum (arrowhead) and spanning across the head of pancreas (star), second (diamond) and third (circle) part of the duodenum; left lobe of the liver (square) in the background.
Post-operative recovery was uneventful. At follow-up 1 month post-operation, the patient was still complaining of ongoing mild abdominal pain associated with oral intake, but no further weight loss was reported. At 3-month follow-up, his symptoms had improved markedly with no further abdominal pain, appetite had improved and patient reported healthy weight gain.
DISCUSSION
Midgut malrotation arises when the normal embryological rotation and fixation of the intestines fails to occur [1]. Disruption at different stages of this process results in various anatomical anomalies and consequent clinical presentations. These include an abnormally high position of the caecum and narrow mesentery predisposing to midgut volvulus and congenital adhesive Ladd’s bands compressing the duodenum with resultant chronic obstructive symptoms [2].
With an estimated incidence of 0.5–1%, most cases are diagnosed in the neonatal period presenting with midgut volvulus [1, 2]. With children and adolescents, presenting complaints are often non-specific and chronic in nature, typically including recurrent abdominal pain, nausea, vomiting, intermittent obstructive symptoms, weight loss and failure to thrive [3]. Adults are more commonly asymptomatic with malrotation found incidentally on imaging or intra-operatively for other indications [1, 3]. Despite being asymptomatic, the rare risk of acute midgut volvulus remains [2].
In addition to acute midgut volvulus, surgical repair of intestinal malrotation with the Ladd’s procedure is generally recommended even for asymptomatic patients to mitigate the risk of future midgut volvulus and its potentially catastrophic consequences. In the symptomatic patients, the procedure can also result in the alleviation of chronic gastrointestinal symptoms related to malrotation [2–5]. Key components of the Ladd’s procedure include detorsion of midgut volvulus if present, division of abnormal Ladd bands running from the caecum to the right upper quadrant to alleviate extrinsic compression, broadening of the mesenteric base to prevent future volvulus, placement of the bowel in a non-rotated position and functional with the duodenum and small bowel on the right side and colon on the left and appendicectomy to avoid future diagnostic dilemma [2, 3, 6, 7].
While traditionally approached by laparotomy, there is increasing evidence supporting the feasibility of the laparoscopic Ladd’s procedure in both adult and paediatric populations [1, 2, 8]. Several retrospective studies have demonstrated less post-operative pain, earlier resumption of normal diet and shorter length of hospital stay with the laparoscopic approach, while complications rates appear similar to laparotomy [1–3, 7, 8]. Also there is the theoretical advantage of less adhesion formation associated with laparoscopy such that the risk of post-operative adhesion-related small bowel obstruction and the risk of recurrent volvulus from re-narrowing of the mesenteric base by new adhesions may be reduced compared to laparotomy [3, 7, 9].
Conversion from laparoscopic to open may be required due to poor vision, bowel distention or if volvulus is suspected. Consequences of converting to an open operation include longer operative times, greater estimated blood loss and longer hospital admission and increased morbidity [8–10]. In a retrospective study of paediatric patients, Skertich et al. found emergency surgery, pre-operative sepsis and need for pre-operative nutritional support to be associated with increased rates of conversion to open. These factors should be considered carefully in the pre-operative planning for an appropriate surgical approach [8].
Feasibility of the laparoscopic approach relies on adequate intra-abdominal working space, and this may be challenging in the presence of acute volvulus with distended and friable bowel and in smaller-sized patients due to an intrinsically smaller abdominal cavity [1, 10]. While the literature exploring this in adults is limited, Svetanoff et al., in a retrospective study of paediatric cases, found a higher success rate with laparoscopy in the absence of volvulus and a 43.8% conversion rate in those with volvulus, while for patients weighing <3 kg, laparoscopy was feasible with a 10% conversion rate [10]. However, no difference was found in the acute post-operative and long-term outcomes for both these subgroups within the limits of their study [10].
Ladd’s procedure for intestinal malrotation can be approached by open or laparoscopic techniques. While laparoscopy may be challenging in certain patient groups and conditions, definitive conclusions to guide patient selection for the laparoscopic approach is limited by the paucity of cases and the retrospective nature of available studies in the literature. Individualized patient assessment and pre-operative planning remains important in determining a safe and effective approach to the Ladd’s procedure.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



