-
PDF
- Split View
-
Views
-
Cite
Cite
Shunya Tamamine, Tomoki Himejima, Toshihito Mitsui, Hiromu Masuoka, Masakatsu Hihara, Natsuko Kakudo, A case of occipital spindle cell lipoma: a case report, Journal of Surgical Case Reports, Volume 2022, Issue 11, November 2022, rjac544, https://doi.org/10.1093/jscr/rjac544
Close - Share Icon Share
Abstract
Spindle cell lipoma (SCL) is a subtype of lipoma first defined by Enzinger; it accounts for ~1.5% of all fatty tumors. Most cases occur in the posterior neck and shoulders of middle-aged men and rarely in women or the occiput. A 41-year-old woman presented to us with complaints of a mass on her left occiput which had slowly grown in size over six years. We excised the tumor, and pathological findings confirmed the diagnosis of SCL. There was no recurrence one year after the surgery.
INTRODUCTION
Spindle cell lipoma (SCL), a subtype of lipoma, is a benign tumor composed mainly of mature adipocytes and spindle-shaped cells. It is rare and accounts for ~1.5% of all adipose tumors and occurs primarily in men between the ages of 45 and 65 years in the posterior neck and shoulders. Herein, we report a case of SCL that occurred on the occiput of a woman and was surgically removed.
CASE REPORT
A 41-year-old woman presented with a complaint of a mass in her left occiput that had slowly grown in size for six years (Fig. 1). She had no history of trauma or surgical procedures in the area and no other medical history, medication or allergy. The clinical diagnosis from the referring physician was ‘suspected epidermal cyst’. On physical examination, we observed a 9.0 × 8.0 cm tumor that was elastic and soft. There was no pain, redness or elevated temperature at the tumor site.

Magnetic resonance imaging (MRI) of her head revealed a discrete, well-defined tumor in the compartment of the left occiput. The internal structure of the tumor was heterogeneous and showed a low-intensity signal on T1-weighted images and an isointense signal on T2-weighted images (Fig. 2). The clinical diagnosis was an SCL or lymphangioma.
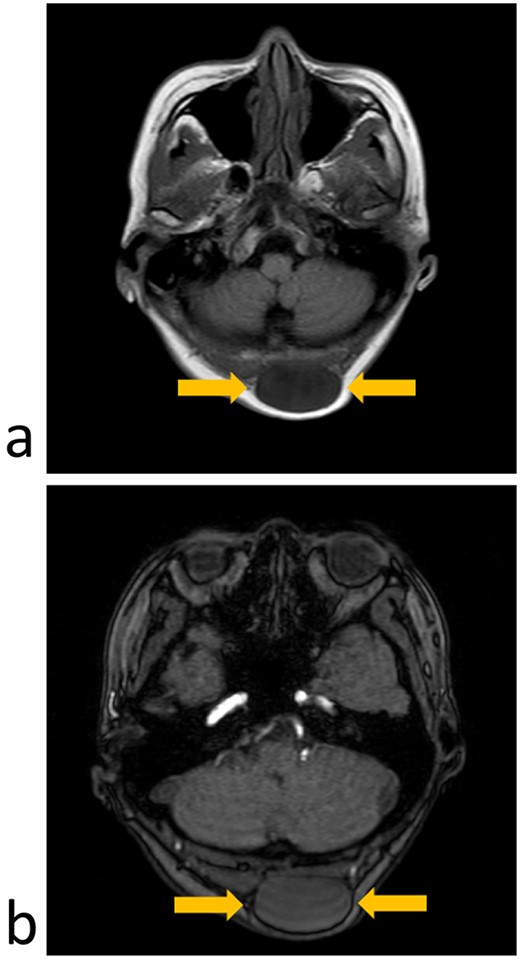
MRI imaging (axial section); (a) T1-weighted image showing a low-intensity signal area under the scalp; (b) T2-weighted images showing an isointense signal of the tumor.
The patient underwent surgical excision of the tumor, which was located between the scalp and galea. It was well encapsulated and separated from the adjacent tissue. There were no adhesions to adjacent tissues or vascular involvement. The mass was 5.1 × 4.5 cm and was completely removed without complications. The patient’s post-operative course was unremarkable (Fig. 3).
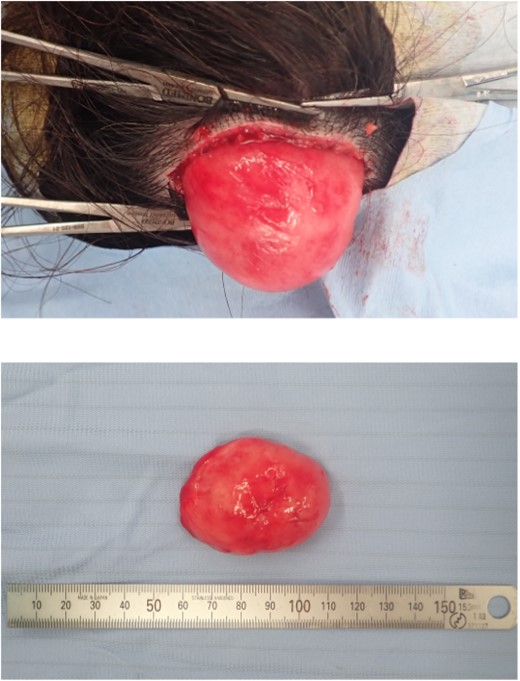
Encapsulated tumor after resection, ~51 × 42 mm in size; no adhesion to the adjacent tissue or vascular involvement.
Pathologically, the lesion was well demarcated, with proliferation of spindle-shaped cells with poor nuclear atypia but low cell density. A small number of mature adipocytes were observed within the lesion. Immunostaining showed that spindle cells were CD34-positive, retinoblastoma 1 (Rb1) absent and S100 protein-negative. Based on the above, a diagnosis of SCL with a poor fatty component was made (Fig. 4). There was no recurrence 1 year after surgery.
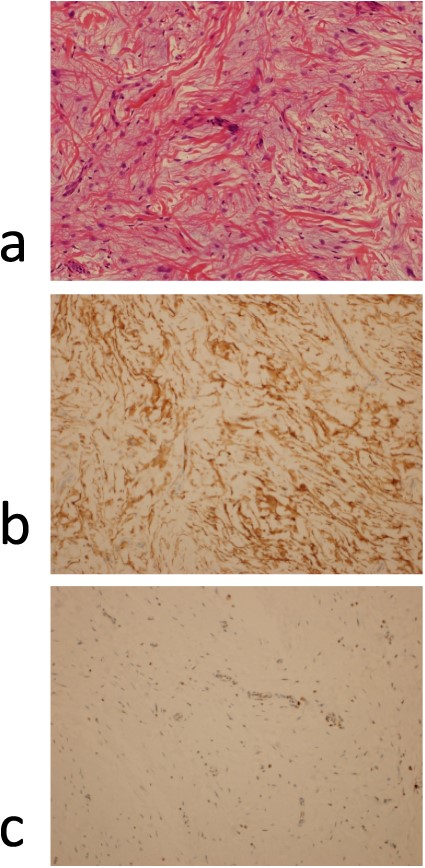
(a) Pathological findings (hematoxylin–eosin stained × 200); there is proliferation of spindle cells with pale nuclei of chromatin along with acidophilic collagen fibers against a background of basophilic mucus-like stroma; immunohistochemistry results (× 200); (b) positive staining for CD 34; (c) positive staining for Rb1.
DISCUSSION
SCL, a subtype of lipoma that was first defined by Enzinger, is a benign tumor composed mainly of mature adipocytes and spindle-shaped cells [1]. SCL occur primarily in men between the ages of 45 and 70 years [1, 2]. It is rare and accounts for ~1.5% of all adipose tumors [3]. It presents as a solitary painless mass with a predilection for the posterior neck and shoulders which is termed the ‘shawl area’. The autopsy case was a lesion on the occipital area of a 41-year-old woman, which is rare considering that 91% of cases occur in men and 87% occur in the ‘shawl area’ [1].
MRI findings of SCL, especially fat findings, vary widely depending on the lesion [4, 5].
Jelinek et al. examined 27 patients diagnosed with SCL and found that 7 (26%) showed ≥90% fat, while 5 (19%) showed no fat at all on MRI [4]. This is thought to be due to histological variations, which are discussed below. In autopsy cases, the fat signal was slight, and correlated with this, there was only a small amount of pathologically mature fat.
Pathologically, SCLs exhibit variable amounts of three elements: bland spindle cells aligned in parallel bundles, mature adipocytes and ropey collagen [6]. However, diagnosis can be elusive when low-fat and free-fat patterns occur [7]. Therefore, immunostaining is used for definitive diagnosis. SCL is characterized by CD34 positivity, S100 protein negativity and Rb1 protein deletion in immunostaining. This contrasts with liposarcoma, which must be differentiated from SCL, which is essentially CD34-negative and S100-positive [5–7]. In the autopsy case, pathology revealed proliferation of spindle-shaped cells with poor nuclear atypia, thickened collagen fibers and a few mature adipocytes, fulfilling the three basic elements of SCL.
In addition, immunostaining was positive for CD34, negative for S100 protein and absent Rb1 protein, and based on these findings, a diagnosis of low-fat SCL was made.
In summary, we present a case of SCL on the left occiput. Subcutaneous tumors that are suspicious for adipose species on physical examination, but lacking a fatty component on MRI, should also be considered as a differential diagnosis for SCL.
ACKNOWLEDGEMENTS
We would like to thank Editage (www.editage.com) for English language editing.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



