-
PDF
- Split View
-
Views
-
Cite
Cite
Wahab Moustafa, Lydia Karamani, Stefan Schreiber, A case of anterior choroidal artery injury after resection of a pilocytic astrocytoma in the amygdale—a case report, Journal of Surgical Case Reports, Volume 2022, Issue 11, November 2022, rjac519, https://doi.org/10.1093/jscr/rjac519
Close - Share Icon Share
Abstract
The anterior choroidal artery (AChA) arises from the last segment of internal carotid artery (ACI), the communicating C7 segment and comprises the terminal branch of ACI. Anatomical its origin located supraclionoidal after the ophthalmic C6 segment of ACI and after the rise of posterior communicating artery. The AChA gains greater importance because of its small size and its region of blood supply. With its perforating branches supplies important intracranial structures such as the optic tract, the posterior limb of the internal capsule, the lateral geniculate body, the medial temporal lobe and the medial area of the pallidum. The anterior choroidal artery is a fine artery and consists of two parts, a cisternal and a plexal one. There are only few studies published, which describe the exact anatomy and the impact of its damage. On the present report, we discuss a case of an iatrogenic injury of the anterior choroidal artery and its hazardous consequences.
INTRODUCTION
The anterior choroidal artery (AChA) is the terminal branch of ACI and arises from the communicating C7 segment. The AChA is a thin artery with a diameter of almost 0.94 on average [1]. It arises only 2–5-mm distal to the posterior communicating artery (PComA) [2] and it is divided in two parts, a cisternal and a plexal one. The cisternal segment extends from the origin of AChA to the choroidal fissure medial to the lateral ventricle. The AChA runs forward intraventricular and enters the choroidal plexus, and at that level consists the plexal segment.
The AChA through its extension supplies critical structures such as the optic tract, the posterior limb of the internal capsule, the lateral geniculate body, the medial temporal lobe and the medial area of the pallidum [3]. Therefore, damages in the cisternal segment can cause infarction in those critical areas with manifestation of serious neurological deficits.
It is also worth mentioning the fact that the AChA provides anastomotic branches with the posterior circulation and especially with the posterior choroidal artery and the posterior cerebral artery. At the same time among all the supplying structures the posterior limb of internal capsule do not receive blood from any collateral circulation rather than from the main AChA branch. Thus the posterior limb of internal capsule is especially vulnerable to damages.
We present a case of a secondary injury of AChA after operating a tumor located in the left amygdale.
CASE REPORT
A 40-year-old man subjected to the outpatient care of our hospital for many years with the diagnosis of temporal epilepsy with complex partial seizures. After a long period free of seizures came in 2019 to a recurrence with episodes of focal epileptic seizures. The brain imaging with cranial magnetic resonance tomography (MRT) revealed a new lesion on the left hippocampus. The patient underwent regularly follow-ups in our outpatient clinic and the lesion has been shown stable until the last brain imaging in May 2022. The lesion has been changed morphologically and presented larger in size, with an increase in contrast enhancement. The lesion has appeared with a total mass of 8 × 14 × 15 mm, hypointense, surrounded by a peripheral hyperintense area, in the Flair sequence, Fig. 1. At that moment the patient complained intermittent dizziness and headache. He was otherwise alert, oriented with glasgow coma scale (GCS) 15/15. There was any cranial nerve palsy or neurological deficit of the extremities. The gait presented smooth and coordinate.
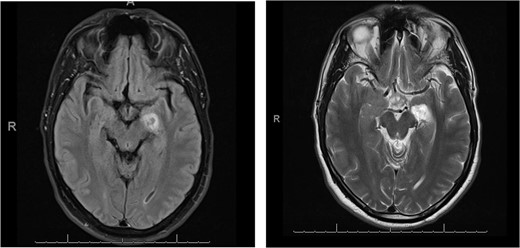
Flair sequence showing the lesion in the left amygdala as hypointense with surrounding hyperintense edema (links). T2-weighted imaging presenting the lesion hyperintense in the left amygdala (right).
The imaging findings have been represented and sufficiently explained to the patient. Based on the radiological progression the surgical resection of the lesion has been indicated.
The patient admitted to our clinic for performing the operation. Through a temporo-parietal approach, we reached the lesion located on the left uncus of hippocampal gyrus. The lesion appeared a grey-glass form with well-recognizable border zone to the neighbor edematous changed tissue. During the tumor preparation came to an adverse injury of a thin vessel running in the choroidal fissure. To avoid a life-threatening intracranial bleeding the vessel had to be sacrificed and had been coagulated.
For the postoperative standard care the patient had been admitted to the intensive care unit. Through an early neurological examination has been revealed a combination of neurological deficits with right hemiplegia, right hemihypesthesia, right facial palsy and ipsilateral hemianopsia.
In regard to the new neurological manifestation we performed a brain magnetic resonance imaging (MRI). This demonstrated in the diffusion-weighted imaging (DW-MRI) an ischemic area in the posterior limb of capsula interna and a ring-shaped lesion in the thalamus, showing in Fig. 2. Moreover it appeared a contrast agent enhancement of 5-mm temporal, which was evaluated as a sing of residual tumor. During the inpatient stay we initiated physiotherapy and ergotherapy, which both resulted to a gradually improvement in clinical performance. In the meantime the histological finding revealed a pilocytic astrocytoma, WHO grad I.
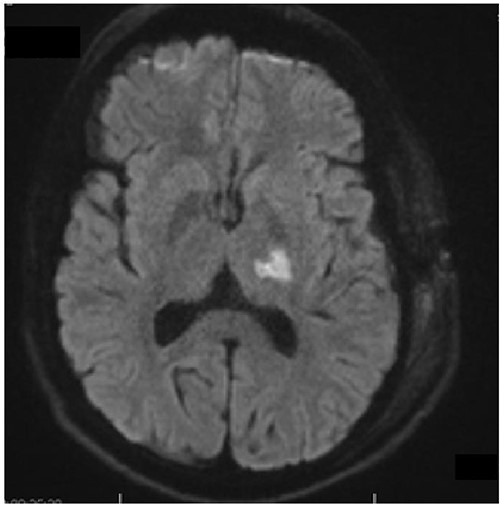
Axial diffusion-weighted MRI shows restricted diffusion in the posterior limb of internal capsule.
DISCUSSION
Here, we described a severe adverse complication with a negative outcome after operating a pilocytic astrozytoma in the left hippocampal region. During the procedure provoked inevitably an injury in the course of anterior choroidal artery affecting the blood supply in critical brain structures. This report refers to an individual experience of a sole case demonstrating an unusual surgical complication.
With respect to the current literature there are many different diseases and conditions, which could affect the patency of AChA. Aneurysmas, arteriovenous malformations (AVM), vasculities, infarction, Moyamoya disease and brain tumors could be detected as risk factors. Referring to the brain tumors the AChA is especially susceptible to tumors located in the lateral ventricle. Recorded are cases of meningeomas, choroid papilloma and gliomas [2].
Even though AChA is a thin artery with almost a diameter of approximately 0.8 mm and a range diameter of 0.3–1.6 mm is very vulnerable to damage [4]. The AChA supplies with blood essential brain areas and an injury on its course could affect the quality of patient’s life. On the present report, we discuss an iatrogenic factor which led to occlusion of the AChA after resection of a pilocytic astrozytoma.
There are two syndromes described after occlusion of AChA; the complete and the incomplete form. The complete form represents typically with hemiplegia, unilateral loss of sensation and hemianopsia. The incomplete form is more common and its clinical manifestation can vary in severity.
It is notable to mention that the hazardous side effects after damaging the AChA presented mostly by affecting its cisternal segment.
ACKNOWLEDGMENTS
The authors would like to express their respect and appreciation to the patient for consenting to this study. We are very thankful for the collegiality and the competence of the team.
AUTHORS’ CONTRIBUTIONS
We would like to thank the authors for their contribution on publishing this case. All colleagues have contributed equally to this study.
TECHNICAL APPENDIX
No complex data were needed. We conducted this study using the online medical bank PubMed and the patient’s chart. We are very grateful for all infrastructure and technical support provided. No statistical code was needed for the aims of this publication.
STRENGTHS AND LIMITATIONS
Major strength of this study is the presentation of an uncommon surgical complication and its educational role in avoiding similar situations. Another advantage arises from the fact that the current literature about similar iatrogenic complications is limited or almost scanty. On the other hand the main limitation of this study is the presentation of an already described syndrome.
ETHICS
A written consent for publication has been obtained from the patient.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



