-
PDF
- Split View
-
Views
-
Cite
Cite
Miraal Dharamsi, Christopher Castagno, Kyle J Klahs, Amr Abdelgawad, Ahmed M Thabet, Unroofing osteotomy for dissociated tibial intramedullary magnetic rod during implant removal: a case report, Journal of Surgical Case Reports, Volume 2022, Issue 11, November 2022, rjac516, https://doi.org/10.1093/jscr/rjac516
Close - Share Icon Share
Abstract
The PRECICE® intramedullary rod (NuVasive, San Diego, CA) utilizes multiple telescopic components to magnetically drive limb lengthening. These devices are routinely explanted after desired growth correction is met. To the author’s knowledge, this is the first description of an osteotomy assisted extraction of a disassociated tibial magnetic lengthening rod. A 17-year-old girl with fibular hemimelia and resolved left tibial length discrepancy after successful surgical lengthening underwent a complex implant removal approximately seven years after regenerate consolidation. During implant removal, the telescopic portion of the rod remained lodged in the tibial medullary canal and a subsequent unroofing osteotomy of the tibia was performed. Tibial limb length discrepancies are oftentimes corrected with complex implants comprised of multiple fragile components that are routinely explanted. During the unfortunate event of a telescopic intramedullary rod dissociation, an unroofing osteotomy can be successfully performed to removal all implant components.
INTRODUCTION
Fibular hemimelia can present as a spectrum of unilateral lower limb deficiencies to include shortened extremity [1, 2]. Treatment options include either amputation or limb reconstruction surgeries, including limb lengthening procedures [1]. The PRECICE® intramedullary rod (NuVasive, San Diego, CA) uses a magnetically driven telescopic mechanism controlled with an external device, to lengthen the limb [3, 4]. The use of internal limb lengthening technologies has been proven to be not only effective but also advantageous as compared to external fixation strategies with risks such as pin tract infections, muscle transfixion and malalignment [4, 5].
Limb lengthening is fraught with possible complications and intramedullary lengthening techniques may present challenges with the rate of lengthening and implant failure [6]. The literature on magnetic lengthening devices is limited in the pediatric population, with a paucity of reported outcomes and complication [7, 8].
In this case report, we describe a rare complication of implant breakage in the tibial medullary canal during routine implant removal. We also explain our surgical approach to retrieve the residual fragment, including tibial unroofing osteotomy for implant removal and subsequent internal fixation.
CASE REPORT
A 17-year-old female with a history of fibular hemimelia and successful left tibia lengthening via telescopic intramedullary rod presented to the orthopaedic clinic to discuss implant removal.
The patient had first presented to the orthopedic clinic at age ten due to limb length discrepancy (LLD) causing a progressively worsening limp. Initial hip to ankle scanogram identified that the left lower extremity (LLE) was shorter than the right by 3.1 cm (Fig. 1A). The patient underwent distal femoral and proximal tibial epiphysiodesis for the right lower limb with no complications. A year later the LLE was 2.5 cm shorter than the right (Fig. 1B). The patient then underwent left tibia and fibula osteotomy with insertion of a bone lengthening intramedullary rod which lengthened by 0.25 mm ×3 a day for eight weeks (Fig. 1C). A delayed union was identified nine months after the lengthening procedure indicating explantation of the two distal and one proximal interlocking screw for dynamization (Fig. 1D). Following the surgery, the patient recovered with osseous union, decreased pain, and improved gait (Fig. 1E).
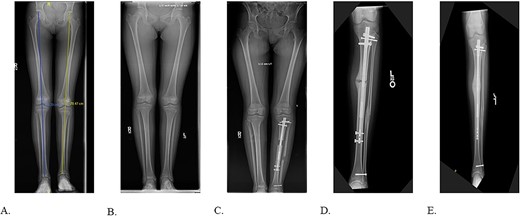
A: 10.5-year-old female with fibular hemimelia, affected left side. B: 11-year-old female status post right distal femur and proximal tibia epiphysiodesis. C: 8-weeks status post left tibia/fibula osteotomy and PRECICE implantation. D: 9-month postoperative PRECICE implantation of left tibia with delayed union. E: 3-months postoperative dynamization of left tibia with osseous union.
Six years after the PRECICE device was implanted the decision was made for its removal due to the patient’s complaints of left knee 8/10 distally radiating pain and in accordance with the manufacturers recommendation to remove the PRECICE intramedullary rod due to the rare earth magnet.
SURGICAL TECHNIQUE
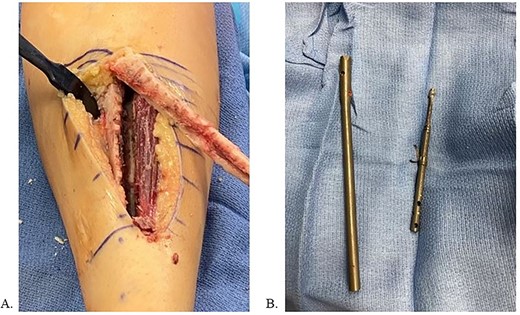
The patient was positioned supine on a radiolucent table with fluoroscopy coming from the contralateral side. The prior infrapatellar scar was incised, revealing bony ingrowth around the proximal end of the implant. A 3.2-mm guide pin was advanced into the center of the implant and a cannulated reamer removed the bony overgrowth. Residual bone surrounding the proximal implant was debrided using a bone curette and then a Nuvasive© conical extractor was attached to the exposed receiving end. The remaining proximal interlocking screw was localized under fluoroscopy and removed. When backslapping the implant, the components disassociated, and the telescopic portion remained lodged in the tibial medullary canal. When consulted intraoperatively, the mother chose to remove all implants by means of tibial osteotomy. An 8 cm long anterior ¼ circumference of the tibia unroofing osteotomy was performed using multiple drill holes and osteotomes (Fig. 2A/B). The remaining portion of the implant was removed with a clamped vice grip and mallet. (Fig. 3A/B). The osteotomy was reduced using a point-to-point reduction clamp and secured with three 2.7-mm lag by technique screws. The wound was irrigated, and 5 cc of demineralized bone matrix was applied to bolster osseous healing.
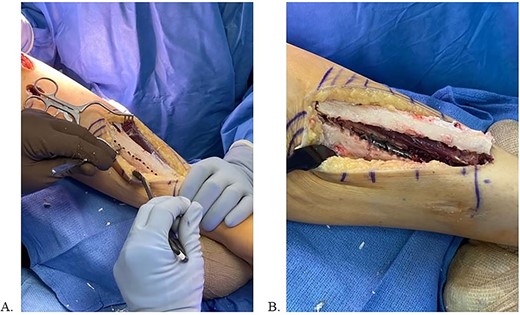
A: Multi-drill hole technique used to facilitate unroofing osteotomy. B: Completed unroofing osteotomy with visible implant.
Final radiographs showed adequate alignment, internal fixation of the tibial osteotomy, and complete hardware removal aside from the three new fixation screws (Fig. 4A). The incisions were closed, dressed and the leg was immobilized in a Controlled Ankle Motion (CAM) boot. The patient spent six weeks non-weight bearing but was able to return to work without any pain or limping at three months post implant removal (Fig. 4B). Final 12-months follow-up demonstrated radiographically healed osteotomy site and maintained equal limb lengths and alignment (Fig. 5A-C).
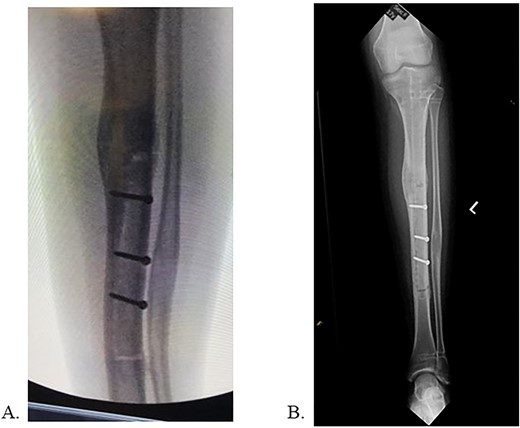
A: Intraoperative radiograph demonstrating complete implant removal with x3 fixation screws. B: 6 weeks postoperative radiographs demonstrating maintained alignment at osteotomy site.
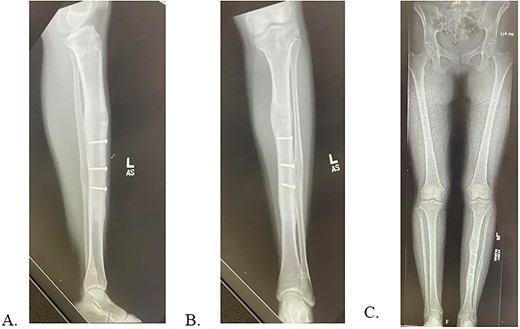
A: 12 months postoperative PRECICE explantation with osseous union at osteotomy site of lateral left tibia. B: 12 months postoperative PRECICE explantation with osseous union at osteotomy site of AP left tibia. C: 12 months postoperative PRECICE explantation with equal limb lengths and alignment.
DISCUSSION
The complexities of implant removal are often overlooked, and surgeons should be prepared when the procedure does not progress as expected. Guidance is needed for physicians who encounter the challenge of unexplained magnetic intramedullary rod breakage [3].
Intramedullary rod utilization for limb lengthening is reliably successful, with its efficacy noted consistently through the literature [5, 7, 9–11]. Femoral and tibial intramedullary implant breakage has been reported due to falls, and due to fatigue failure at the welding seam; however, removal strategy remains elusive [4, 8, 12]. In our case, the distal interlocking screws had previously been removed during the dynamization surgery. The bony ingrowth into the distal interlocking holes may have resulted in the mechanical failure between the two parts of the telescopic rod. Utilizing perfect circle technique and re-drilling the distal interlock screw holes may have removed the osseous ingrowth and allowed for easier explanation; however, this step was not attempted. Osteotomies have also been used for explanting tibial intramedullary implants after breakage [13]. Multiple drill hole osteotomy technique has been described to be superior when compared to osteotomy using an oscillating saw or Gigli saw, due to greater preservation of the periosteum and less necrotizing heat generation, allowing for faster bone healing and new bone formation [14, 15].
All surgical procedures and operations carry inherent risk of complications that can normally be mitigated through pre-operative planning, and adherence to established protocols. This case demonstrates that in the unexpected event of a telescopic intramedullary device dissociation, an unroofing osteotomy can be successfully performed.
STATEMENT OF INFORMED CONSENT
The patient was informed that data concerning the case would be submitted for publication. The patient agreed and consented to release of this data for publication.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



