-
PDF
- Split View
-
Views
-
Cite
Cite
Jay Lodhia, Anande Kumbwaeli Salewi, Happiness Sway, Adnan Sadiq, David Msuya, Late presentation of midgut malrotation in a young adult, Journal of Surgical Case Reports, Volume 2022, Issue 11, November 2022, rjac515, https://doi.org/10.1093/jscr/rjac515
Close - Share Icon Share
Abstract
Midgut malrotation is a congenital anomaly due to partial or complete failure of rotation of the midgut in fetal life. Majority of the cases present in the neonatal period and 90% within the first year. Adult presentation is rare and the true incidence is unknown as some cases pass undiagnosed. Whirlpool sign is pathognomic for midgut malrotation and management involves surgery.
INTRODUCTION
Midgut malrotation is a congenital anomaly in the embryological development, and it approximately affects 1 in 500 births; however, a number of cases can go undetectable [1]. Adult midgut malrotation is rare with an incidence between 0.0001% and 0.19% in asymptomatic adults. It is hard to determine the true incidence of adult malrotation due to the non-specific signs and symptoms [2]. In the case report, we present a young adult with midgut malrotation and highlight the importance of a thorough clinical history and higher imaging modalities to aid diagnosis.
CASE PRESENTATION
A 19-year-old male was brought to us with a 2-day history of non-projectile vomiting of an average of 2–3 episodes a day, containing greenish material and associated with peri-umbilical pain. He also reported a history of constipation, generalized body weakness and significant weight loss. He denied history of abdominal distension and fever. However, he reported the symptoms to have been long standing since he was 6 years old whereby he experienced such symptoms twice a month. He reported relief of the symptoms when he takes liquid diet.
On admission, he was clinically weak and undernourished, mildly dehydrated but not pale. He was not jaundiced, there was no lower limb edema nor enlarged peripheral lymph nodes. His supine blood pressure was 102/55 mmHg, resting pulse of 98 beats per minute, respiration rate of 17 breaths per minute and saturating at 95% on room air. His random blood glucose was of 8.4 mmol/l. His body mass index was 16 kg/m2. He had a scaphoid abdomen with periumbilical tenderness, no organomegaly appreciated, succession splash was positive and normal bowel sounds were heard on auscultation. Other systems were essentially normal.
His laboratory results revealed a normal leucocyte count and hemoglobin of 12.2 g/dl. His serum sodium was 122.40 mmol/l and potassium was 2.57 mmol/l. Renal and liver function tests were within normal range as well as serum albumin and total protein. His abdominal ultrasound was normal. His esophageal-gastro-duodenoscopy showed normal mucosa with 2 l of bilious contents in the stomach; however, no obvious obstruction seen. His abdominal–pelvic computed tomography (CT) scan showed a severely dilated duodenum with a transition point at the superior mesenteric artery. Twisting of the mesentery seen around the superior mesenteric artery with ‘Whirlpool sign’ (Fig. 1). These features suggestive of midgut volvulus.
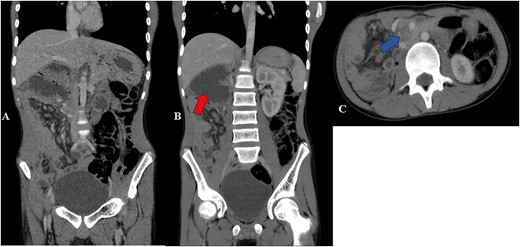
Contrast CT abdomen—coronal (A and B) and axial views (C) show small bowels on the right side of the abdomen and the large bowels on the left side of the abdomen. Image B shows distended duodenum (red arrow). Image C shows twisting of the mesentery and the superior mesenteric artery giving whirlpool sign appearance (blue arrow).
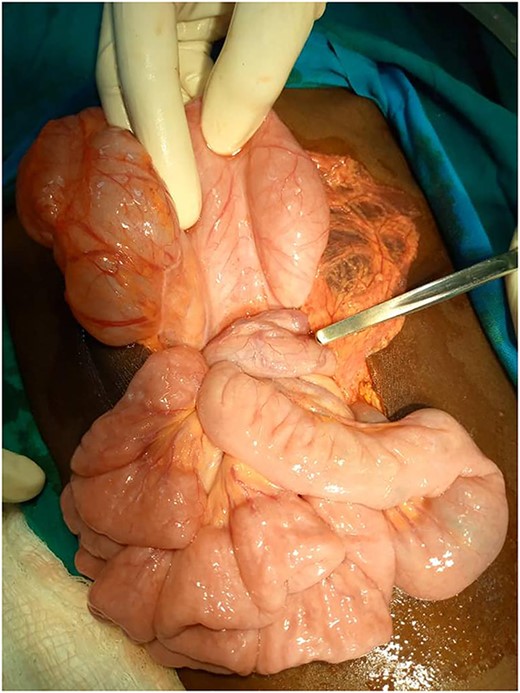
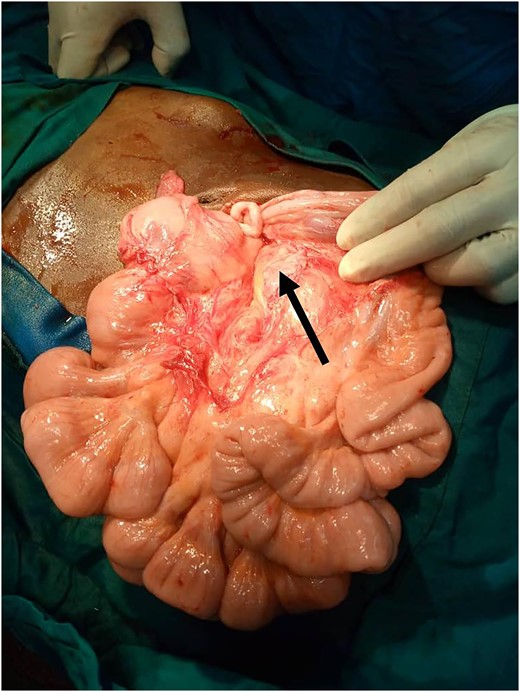
During the stay in the ward, the patient was kept on maintenance intravenous fluids along with 3% sodium chloride, oral rehydration solution and potassium chloride to correct electrolytes, meanwhile on semi-solid diet. He was then scheduled for a laparotomy whereby intraoperatively there was midgut malrotation. The second and third parts of the duodenum were twisted around the superior mesenteric artery (SMA) causing gastric outlet obstruction (Fig. 2). There was a grossly distended stomach and first part of the duodenum. The cecum along with the rest of the colon was at the right side and the small bowels were on the left side of the peritoneum. Ladd’s procedure was done to maintain gastrointestinal patency (Fig. 3).
He continued to fair well postoperatively and was discharged on Day 2 post-surgery with oral analgesia and antibiotics. He was reviewed 2 weeks post-surgery whereby he was tolerating oral feeds well and control serum sodium, potassium and hemoglobin were within normal range.
DISCUSSION
Initial presentation of symptomatic adult midgut malrotation is rare and the incidence is approximately 0.2%. Ninety percent of the patients will present in their first year of life [1]. Midgut malrotation is a congenital anomaly and is considered a failure of the normal 270° counterclockwise rotation of the gut between the 5th and 11th weeks of gestation [1, 2]. This forms a narrow SMA pedicle and lack of posterior peritoneal fusion, leading to subsequent midgut volvulus and obstruction with potential vascular compromise as was seen intraoperatively in the index case [1].
Midgut malrotation in adults may present as an acute abdomen that requires urgent intervention but may also present in non-acute setting with non-specific and chronic symptoms as our case, which include intermittent abdominal pain, bloating and food intolerance hence leads to increased morbidity and mortality [3]. This unspecific features cause delay in diagnosis similar to our case [3]. The acute features include midgut volvulus, small bowel obstruction and bowel ischemia [3]. Upper gastrointestinal series with oral contrast is the test of choice in the pediatric group along with Doppler ultrasound of the SMA; however, currently contrasted CT scan is the modality of choice showing ‘whirlpool’ sign as seen in Fig. 1 [4].
Intervention includes surgery (Ladd’s procedure), which consists of counterclockwise derotation of the midgut, division of the Ladd’s bands, widening of the narrowed root of the small bowel mesentery and performing appendectomy [5]. Appendectomy is performed to avoid diagnostic challenges in the future as reported by Hanna et al. whereby their patient presented with left-sided appendicitis and midgut malrotation was found intraoperatively [6, 7]. Other differentials include cecal volvulus, mesenteric ischemia, irritable bowel syndrome, adhesions, Crohn’s disease and pancreatic diseases [8, 9].
Malrotation is rarely seen in adults; hence diagnosing its presentation can be difficult. Surgeons therefore should be familiar with midgut malrotation and consider this as a differential diagnosis when comes across adult patients with chronic atypical abdominal pain and intermittent partial small bowel obstruction. Surgeons should be able to perform complete Ladd’s procedure and, if necessary, seek assistance from a pediatric surgeon.
ACKNOWLEDGEMENTS
The authors would like to thank the patient for permission to share his medical information to be used for educational purposes and publication.
CONFLICT OF INTEREST STATEMENT
The authors declare they have no competing interests.
FUNDING
No funding or grant support.
INFORMED CONSENT
Written informed consent was obtained from the patient for publication for this case report; additionally, accompanying images have been censored to ensure that the patient cannot be identified. A copy of the consent is available on record.
AUTHORS’ CONTRIBUTIONS
J.L. and A.K.S. conceptualized and drafted the manuscript. J.L. and D.M. were the lead surgeons. A.K.S. and H.S. reviewed the medical records and A.S. reviewed and reported the radiology films. All authors have read and approved the final script.



