-
PDF
- Split View
-
Views
-
Cite
Cite
Taro Ikeda, Takashi Hosokawa, Shunpei Goto, Makoto Hashimoto, Eri Nagasaki, Takayuki Masuko, Successful laparoscopic-assisted partial splenectomy and splenopexy with umbilical approach to wandering spleen with an enlarged cyst in a pediatric patient, Journal of Surgical Case Reports, Volume 2022, Issue 10, October 2022, rjac483, https://doi.org/10.1093/jscr/rjac483
Close - Share Icon Share
Abstract
A 10-year-old girl with a wandering spleen with an enlarged cyst was successfully treated by laparoscopic-assisted partial splenectomy and splenopexy. The patient visited our hospital with a complaint of a lower abdominal mass. Abdominal computed tomography showed malposition of the spleen and the presence of a 10 cm diameter splenic cyst (SC) in the lower pole. In surgery, the navel was opened with an inverted Y-shaped incision. The SC was punctured and aspirated the contents of the cyst, the migrating spleen was pulled out of navel and the partial splenectomy was done. The residual spleen was laparoscopically fixed by creating an extraperitoneal pocket. Pathologically, the cyst was covered with a vitrified fibrotic capsule and was diagnosed as a pseudocyst. We considered it a traumatic cyst. The postoperative course was uneventful. This minimally invasive laparoscopic procedure was feasible and effective for treating wandering spleen with a large SC in a pediatric patient.
INTRODUCTION
Splenic cyst (SC) is a rare condition, and wandering spleen with a SC is even rarer. Treatment for SCs varies depending on the pathological diagnosis of the cyst and age. For a wandering spleen, splenic fixation is the standard method if there is no blood flow disturbance and the spleen can be preserved.
We report a case of a wandering spleen with a giant SC, which underwent laparoscopic-assisted partial splenectomy and splenopexy with a favorable outcome.
CASE REPORT
The patient was a 10-year-old girl. She visited our hospital after her grandmother noticed a mass in her lower abdomen that she had been aware of for 6 months. Abdominal ultrasonography revealed that she had a large mass centered in her lower abdomen. The tumor border was clear, the internal structure was heterogeneous and the blood flow was poor (Fig. 1). We suspected an ovarian tumor, but blood tests showed no elevated tumor markers such as AFP and CA19–9. Abdominal magnetic resonance imaging revealed a cystic mass 10 cm in diameter with high intensity on T1-weighted images and high intensity on T2-weighted images (Fig. 2). Abdominal computed tomography revealed a spleen near the navel and a cystic lesion with poor contrast that continued from the lower pole of the spleen (Fig. 3).
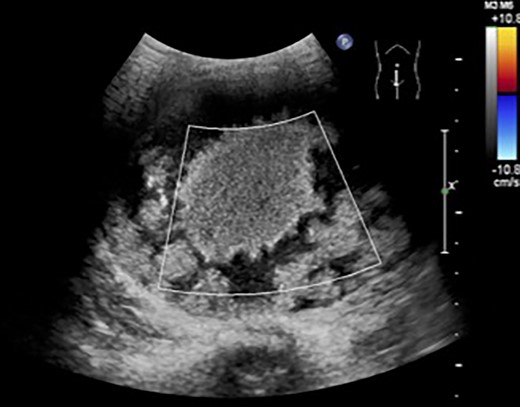
Abdominal ultrasonography revealed a large mass centered in her lower abdomen. The tumor border was clear, the internal structure was heterogeneous and the blood flow was poor.
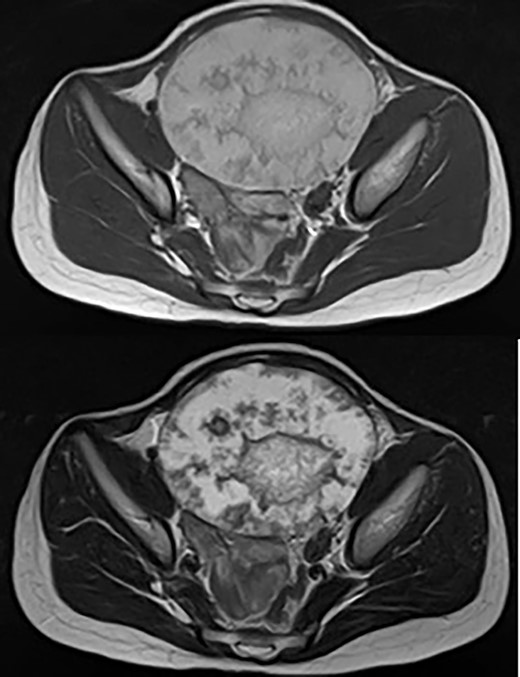
Abdominal magnetic resonance imaging revealed a cystic mass 10 cm in diameter with high intensity on T1-weighted images (upper) and high intensity on T2-weighted images (lower).
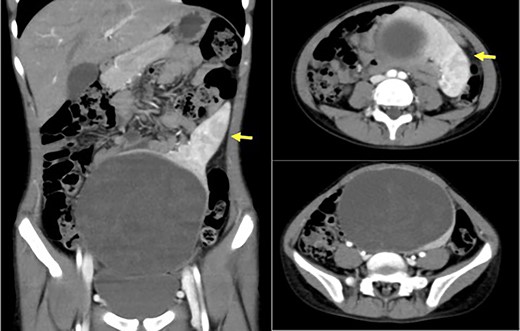
Abdominal computed tomography revealed a spleen (arrows) near the navel and a cystic lesion with poor contrast that continued from the lower pole of the spleen.
We diagnosed it as a wandering spleen with a giant SC and performed surgery. A small laparotomy was performed through an inverted Y-shaped incision of the navel, and a SC was found just below the wound. A partial biopsy of the cyst wall was performed, and a rapid pathological examination ruled out a malignant tumor. Aspiration of the cyst contents allowed the spleen to be externalized. Under direct vision, the blood vessels leading to the lower segment of the spleen were sealed, the splenic parenchyma was dissected by soft coagulation and a partial excision of the spleen was performed. The preserved upper pole of the spleen was put back into the abdominal cavity, and a pocket was made in the retroperitoneum under the left diaphragm using a laparoscopic method to store and fix the spleen (Fig. 4). Pathological examination revealed a pseudosplenic cyst covered with a hyalinized fibrous capsule. It was thought that chronic external force was applied to the migratory spleen and pseudocysts were formed. The postoperative course was uneventful and the patient was discharged from the hospital on the eighth postoperative day. At present, 3 years have passed, and the spleen has reached the same size as the ipsilateral kidney, and the cosmetic appearance is satisfactory.
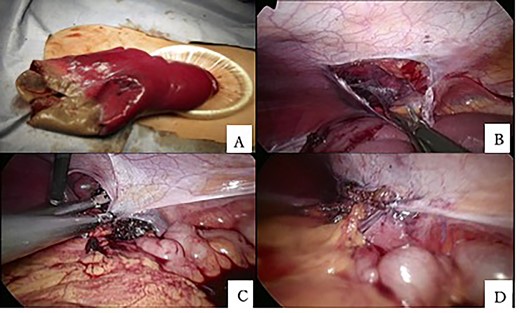
(A) The spleen could be externalized by aspiration of the cyst contents through an umbilical incision. (B) A retroperitoneal pocket was created under the left diaphragm laparoscopically. (C, D) The superior pole of the spleen was placed in the retroperitoneal pocket and fixed.
DISCUSSION
SC is a rare condition with an incidence of 0.75 per 100 000 and is usually asymptomatic. It is incidentally found during ultrasonography or other imaging modalities [1]. It can be classified as a true cyst or a pseudocyst depending on whether it has an epithelial lining. True cyst can be either congenital or acquired. Pseudocyst of the spleen originates from traumatic injury, hemorrhage, infection and infarction [2, 3]. The indications for treatment are not clear and depend on the size and nature of the cyst, age and symptoms. The large cyst larger than 5 cm is candidates for surgery because of the high risk of complications such as rupture and the low possibility of spontaneous recovery. Therefore, their treatment is absolutely necessary and laparoscopy/laparotomy splenectomy is the method of choice [4].
In 1878, Martin [5] first reported a case of wandering spleen in Berlin, Germany. In 1895, Rydygier [6] completed the splenic fixation for the first time. The spleen was fixed in the cavity formed by the abdominal posterior wall peritoneum to treat the wandering spleen. Hall [7] reported that the lower pole of the spleen was fixed in the retroperitoneal space, while the spleen pedicle was fixed to the peritoneal incision, and the upper pole of the spleen was suspended and fixed to the ribs. Since a wandering spleen may cause torsion and may require emergency surgery, surgery is necessary even if the patient is asymptomatic. A variety of methods have been tried since the first report [6]. The Pouch method and mesh fixation of the spleen to the retroperitoneum are known. Fukuzawa et al. [8] reported a method of laparoscopically exfoliating the retroperitoneum under the left diaphragm using a balloon and fixing the spleen by dropping it into the space.
However, there have been few reports of wandering spleen with giant SC, and no treatment has been established. Awe et al. [9] reported that a splenectomy by laparotomy was performed for a wandering spleen with SC complaining of occasional abdominal discomfort. Splenic fixation seems to have been difficult to perform in the past due to problems with the surgical technique and the possibility of recurrence. Upadhyaya et al. [10] reported that laparoscopic cystectomy and splenic fixation were performed for a large splenic spleen with a large splenic cyst complaining of dysmenorrhea. In addition, Fonseca et al. [11] reported that partial splenectomy and splenic fixation were performed for a wandering spleen with partial strangulated necrosis due to torsion, and no recurrence was observed.
In a wandering spleen with SC, as in our case, the spleen can be pulled out of the wound by aspiration of the cystic contents through a small umbilical incision, enabling safe partial splenectomy. In addition, we believe that this method of laparoscopic fixation of the preserved spleen is useful in terms of safety and cosmesis.
For wandering spleen with giant cysts, it is important to safely perform splenic preservation and splenic fixation to prevent recurrence of migration as much as possible.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



