-
PDF
- Split View
-
Views
-
Cite
Cite
Kennedy K Misso, Christina Mapunda, Omar Said, Vanessa Poppe, Mugisha Nkoronko, Kondo Chilonga, Infant gastroduodenal necrosis: a case report, Journal of Surgical Case Reports, Volume 2022, Issue 1, January 2022, rjab645, https://doi.org/10.1093/jscr/rjab645
Close - Share Icon Share
Abstract
We report a case of a two month old baby who had presented with an acute abdomen. Intra operative necrosis of the abdominal esophagus to distal of ligamentum treitz was noted. He was subjected to palliative care and passed away on Day 8 post-surgery.
INTRODUCTION
Perforation and necrosis of the stomach is a rare event post-neonatal period. It is a fatal condition that occurs mostly during neonatal period; fewer cases have been reported in Japan during infancy [1]. The stomach is relative mobile, distensible with three muscular layers and vast of blood supply, making it resistant to perforation post-neonatal period [2]. Nearly all perforations in infancy occur in the neonatal period. The risks being prematurity, low birth weight, asphyxia, annular pancreas and gastrointestinal obstruction [2]. In adults, majority of perforations are due to peptic ulcer diseases and gastroduodenal malignancies [2].
CASE REPORT
A case of a 2-month-old male baby referred to our facility with 1-week history of abdominal pain, abdominal distension associated with inability to pass stools and low-grade fever. He had uneventful pre-natal and postnatal periods. His mother took him to traditional healers where herbal medications were given of which she could not recall or specify their nature. Upon examination, he was tachypneic with a respiratory rate of 40 breaths per minute, saturating at 94% in room air with a silent distended abdomen and hypothermia of 35.2°C. His blood cell count revealed a leukocytosis of 28 billion cells per liter, neutrophil and lymphocyte predominance by 53.2 and 36%, respectively. An abdominal ultrasound revealed ascites, paralytic bowels and ruled out intussusception.
He was then prepared for exploratory laparotomy, and intraoperative gastrointestinal fluid of about 200 ml was noted and drained (Fig. 1).
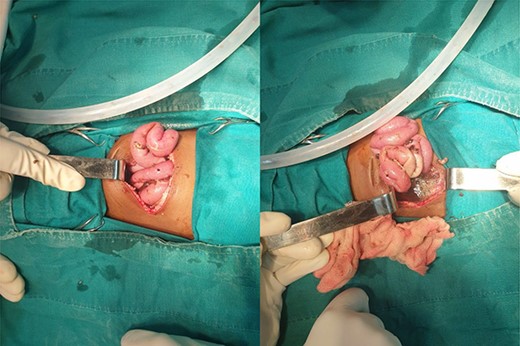
Intestinal fluid leaking into peritoneal cavity, with change in color of the proximal jejunum.
Necrosis of 20 cm of the jejunum extending cephalad to involve the duodenum, stomach and abdominal part of the esophagus was noted with extensive autolysis from abdominal esophagus to the ligamentum treitz (Fig. 2).
Nasogastric tube was vivid seen within the peritoneal cavity, exiting from abdominal esophagus (Fig. 3).
Due to the extensive nature of the pathology and clinical stability of our patient, a decision to close the abdomen was made. His parents were counseled on the prognosis of their baby.
Post-operative, he had acute kidney injury that resolved, a high output enterocutaneous fistula deep seated surgical site infection and respiratory distress. He was managed conservatively on palliative basis with crystalloids and supportive oxygen therapy. He died on Day 8 post-operative.
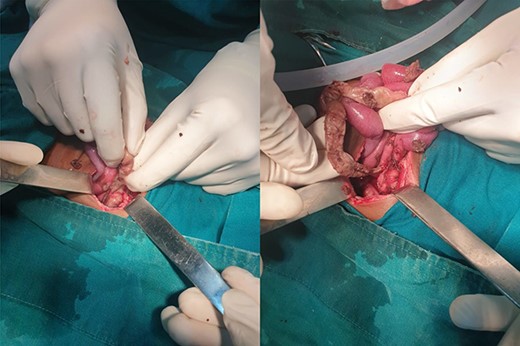
Necrosis of the jejunum and whole length of duodenum with detached mesentery.
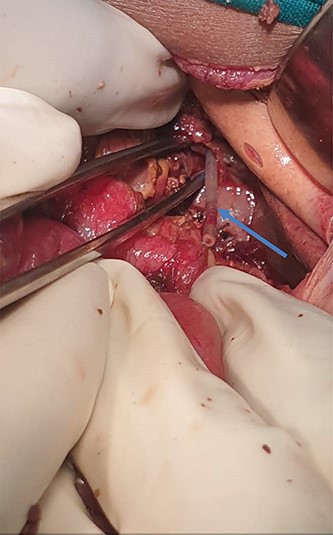
Orogastric tube seen at the abdominal end of the esophagus. (blue arrow).
DISCUSSION
To the best of our knowledge, we have never come across of such an extensive necrosis and autolysis that had a descending pattern from abdominal esophagus to proximal 20 cm of the jejunum. Not from published case reports, such an incident has been reported. Macroscopically, the pancreas and hepatobiliary were normal. The small bowel and the colon were well perfused and healthy. We postulate that our patient had an acute abdomen that was made worse by the herbal medications given. We hypothesize that there were both duodenal and gastric perforations that caused leakage of their secretions as well as bile and pancreatic fluids. Creating a caustic environment that caused autolysis and necrosis of surrounding structures. Alternative theory is that our patient had selective ischemic infarcts that were partially occluding the celiac trunk and superior mesenteric artery.
CONCLUSION
Herbal intoxication remains a common practice in our population. With unmeasured dose of the active ingredient that comes from it. Improvement in health-seeking behavior, particularly in vulnerable population, is critical.
ACKNOWLEDGEMENTS
The authors express their sincere gratitude to all members of the Emergency Medicine Department, all nurses of the general surgery and the main operating theater staffs who were directly involved in caring and managing our patient throughout his illness. We also appreciate the parents of our patient for overwhelming readiness and consenting for the academic forum.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
This work was not financially supported.
CONSENT
Parents of our patient provided a written consent to proceed with academic publications.
GUARANTOR
All authors in the article accept full responsibility for the work, had access to the patient’s information and decision to publish.



