-
PDF
- Split View
-
Views
-
Cite
Cite
Magdalena Rufa, Adrian Ursulescu, Alina Stan, Nora Göbel, Marc Albert, Ulrich F W Franke, Cryopreserved aortic homograft, lifeline treatment for infected vascular prosthesis with mediastinal abscess in a re-redo case, Journal of Surgical Case Reports, Volume 2022, Issue 1, January 2022, rjab644, https://doi.org/10.1093/jscr/rjab644
Close - Share Icon Share
Abstract
We report about a 61-year-old man who, 6 years after initial uncomplicated mitral valve repair and 3 months after treatment of a pseudo-aneurysm of the ascending aorta with a Dacron patch, was admitted in our institution with an infection of the vascular graft, which was associated with sternal osteomyelitis and purulent cutaneous fistula. In a re-redo procedure, the proximal aortic arch and the ascending aorta were replaced with a cryopreserved aortic homograft. The infected part of the sternum was resected and the defect was covered by mobilizing the mediastinal tissue and with a bilateral muscle flap. The patient was discharged 20 days after surgery. This treatment concept outlines the benefit of cryopreserved aortic homograft when faced with a complex thoracic aortic infection.
INTRODUCTION
Sternal osteomyelitis combined with an infection of a vascular graft is a serious complication following open-heart surgery, with high mortality rates. In these cases, the explanation of the infected graft is the recommended treatment. Cryopreserved arterial homografts are very resistant against infection and offer good long-term results in cases of infection of either native arteries or prosthetic grafts. We present a rare case of sternal osteomyelitis, combined with a cutaneo-mediastinal fistula path, and consequently, infection of a vascular graft as a very late complication after open-heart surgery.
CASE REPORT
A 54-year-old patient underwent a mitral valve reconstruction using a quadrangular resection of the P2 segment and annuloplasty for severe regurgitation of the mitral valve. After an initial uneventful recovery, the patient returned 3 months later with fatigue, anemia, systemic inflammatory syndrome and beginning heart failure. The cause for his symptoms was a 5.5-cm pseudo-aneurysm of the ascending aorta, which was compressing on the outflow tract of the right ventricle as well as on the pulmonary artery. The aneurysm was surgically resected and the defect was closed with a Dacron patch. The pathological examination of the aneurysm showed that it was not infectious. Over the next 4 years, he presented periodically with superficial wound infections, which were treated with antibiotics and local debridement.
At almost 6 years after the initial surgery, the patient was transferred to our unit with a chronic sternal fistula. The computed tomography (CT) scan showed almost complete destruction of the manubrium sterni on the left side, a fistula path into the anterior mediastinum and an abscess collection around the ascending aorta (Fig. 1). The echocardiography ruled out any significant valve regurgitation or stenosis, endocarditis or aortic root abscess. Pseudomonas aeruginosa was cultivated from the fistula.
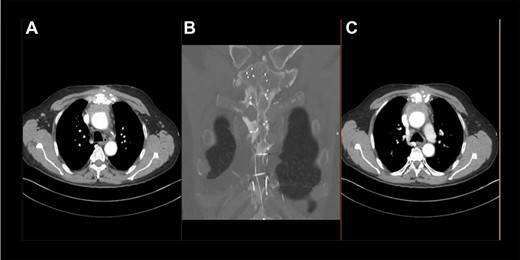
Preoperative thoracic CT scan; (A) image indicates the sternal defect caused by osteomyelitis and the infected hematoma surrounding the native aortic arch; (B) topogram indicating the sternal defect caused by osteomyelitis in coronary sectional plane; (C) image indicates the sternal defect caused by osteomyelitis and the infected hematoma surrounding the aortic prosthesis.
After cardiopulmonary bypass initialization and opening the sternum, one could see the fistula path affecting only the left side of the manubrium sterni and reaching into the mediastinum. Around the ascending aorta was an infected hematoma, with clear infiltration of the Dacron patch, no signs of aortic root abscess or infection. The patient underwent hypothermic circulatory arrest with selective antegrade brain perfusion. The ascending aorta and the proximal two-thirds of the aortic arch were replaced with a cryopreserved aortic homograft (Fig. 2). The fistula path together with the manubrium sterni and the cartilage to the second left rib were completely resected. The rib was then fixated to the right side of the sternum using a titanium plate. The remaining sternum was treated with antiseptic solution and was then conventionally closed with sternal wires. The pectoralis major was mobilized on both sides together with the skin and was used to stabilize the wound.
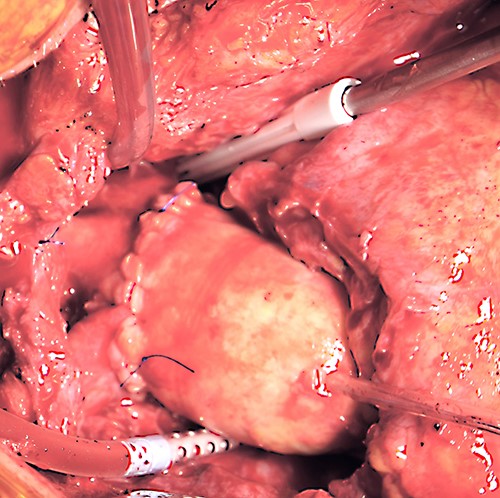
Intraoperative photograph demonstrating the surgical result after homograft replacement of the ascending aorta and aortic hemiarch.
The post-operative course was uneventful and the patient was discharged 20 days after surgery.
The histological analysis confirmed different stages of infection and inflammation of the resected aorta. Pseudomonas aeruginosa was cultivated from the intraoperative cultures. The patient received a combination of three antibiotics for 7 days, followed by single gentamicin treatment for another 10 days. The scar healed without any signs of inflammation. The control CT scan showed good consolidation of the sternum with no signs of infection (Fig. 3).
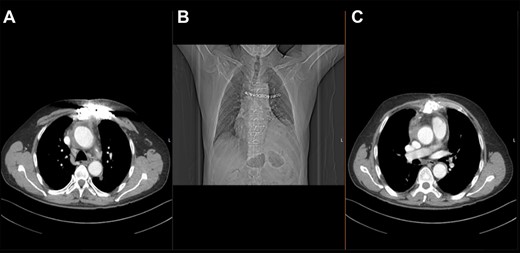
Post-operative thoracic CT scan; (A) chest wall reconstruction in transverse sectional plane; (B) topogram showing sternal wires and titanium plate arrangement; (C) chest wall closure and aortic homograft with small seroma collection in transverse sectional plane.
At his follow-up visit after 6 months, and again 5 years after surgery, the patient was completely restored into normal life and the sternal wound was perfectly healed.
DISCUSSION
Sternocutaneous fistulas are rare, but since they may have a devastating course, increased awareness of this infectious complication after open-heart surgery is important [1]. Moreover, sternal osteomyelitis combined with an infection of a vascular graft is a life threatening complication. Staphylococcus aureus is the most frequent organism found after coronary artery bypass grafting surgery. Candida species and gram-negative bacteria are more common after heart or heart–lung transplantation. Pseudomonas aeruginosa has been rarely reported [2]. Complete resection of the infected foreign material and of the affected aorta with debridement of the surrounding tissue, followed by antibiotic treatment, gives most probably the best results. An orthotopic reconstruction is the best option for all thoracic and thoraco-abdominal pathologies, and the use of coated prostheses, homografts or self-made vascular tubes from xenopericardial tissue has to be discussed from case to case [3]. The use of cryopreserved homografts is related to low reinfection rates and decreased early and mid-term mortality, especially when aggressive debridement has been undertaken [4, 5].
The use of pedicled myocutaneous or muscle flaps without sternal resection and/or omental transposition has proved to be an effective and reliable method for the management of patients with complicated cardiothoracic problems [1, 6–11]. In our case, the described sternal reconstruction technique in combination with antibiotic treatment proved to be an additional option for the successful management of advanced sternal osteomyelitis.
CONSENT
Written informed consent was obtained from the patient for the publication of this case report and any accompanying images.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.
AUTHORS’ CONTRIBUTIONS
All authors participated in the design of the case report and coordination and helped to draft the manuscript. All authors read and approved the final manuscript.
References
Carrel T1,



