-
PDF
- Split View
-
Views
-
Cite
Cite
Kian C Banks, Diana S Hsu, Jeffrey B Velotta, Extrapleural pneumonectomy for recurrent thymoma diagnosed after return of paraneoplastic Morvan syndrome, Journal of Surgical Case Reports, Volume 2022, Issue 1, January 2022, rjab636, https://doi.org/10.1093/jscr/rjab636
Close - Share Icon Share
Abstract
A 50-year-old male with history of HIV, syphilis, paraneoplastic Morvan syndrome secondary to thymoma resected in 2013 presented recently with tachycardia, tremors, diarrhea, hyperhidrosis and bilateral lower extremity pain leading to the discovery of thymoma recurrence. He initially developed Morvan Syndrome after thymectomy in 2013 and gradually improved with negative anti-contactin-associated protein-like 2 antibody testing in 2017 and symptom resolution in 2018. Upon return of dysautonomia symptoms, subsequent imaging revealed widespread disease recurrence diffusely in the right lung parenchyma and pleura for which he underwent right extrapleural pneumonectomy. He was managed with low-dose prednisone perioperatively, but when his symptoms worsened, he was started on rituximab and methylprednisolone. Nearly 3 months from surgery, he died from urinary sepsis. This represents a unique case of recurrent paraneoplastic Morvan syndrome leading to the diagnosis of metastatic thymoma as well as the challenges of symptom control during the surgical management of the underlying disease.
INTRODUCTION
Paraneoplastic Morvan syndrome is a rare disorder comprising of dysautonomia, neuropsychiatric features, neuropathic pain and neuromyotonia that is typically associated with thymoma [1]. Most cases present with onset of Morvan syndrome prior to diagnosis of the underlying tumor and are improved after treatment of the tumor [1, 2]. However, there have been reported cases of initial presentation of symptoms presenting after disease recurrence [2]. Here, we present our management of a case in which paraneoplastic Morvan syndrome initially presented upon thymoma resection, gradually resolved and then returned prior to identification of tumor recurrence.
CASE REPORT
A 50-year-old male with history of HIV, syphilis, paraneoplastic Morvan syndrome secondary to thymoma resected in 2013 presented more recently with tachycardia tremors, diarrhea, hyperhidrosis and bilateral lower extremity pain leading to the discovery of disease recurrence.
Previously, in 2013, he had presented with dyspnea and was found to have a stage III type AB thymoma for which he underwent median sternotomy, thymectomy and partial right middle lobectomy. After surgery, he developed symptoms of hyperhidrosis, tremors, tachycardia, tachypnea, anxiety, anorexia, hallucinations and altered mental status. At that time, he tested positive for anti-contactin-associated protein-like 2 (CASPR2) antibody and was diagnosed with paraneoplastic Morvan syndrome. He had no improvement with intravenous immunoglobulin but responded successfully to one dose of rituximab. Thereafter, he was maintained on prednisone and azathioprine until he was weaned off all medications in 2018 when his symptoms had completely resolved. As of 2017, his anti-CASPR2 antibody level was negative.
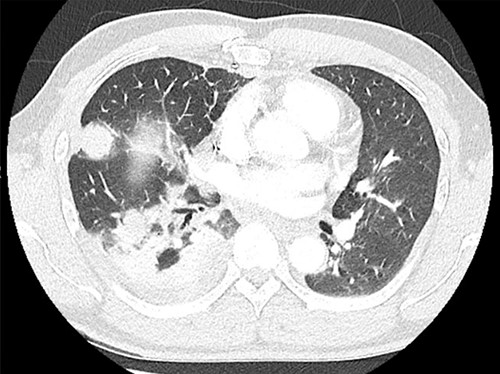
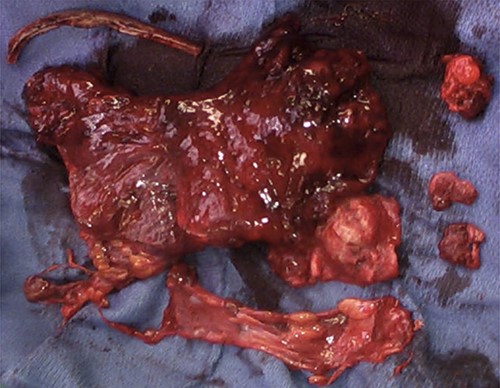
After redeveloping the symptoms of dysautonomia, he was found to have a positive anti-CASPR2 antibody level as well as recurrent disease in the right lung parenchyma and pleura (Fig. 1). His case was evaluated by a multidisciplinary team of thoracic surgery, neurology, medicine and oncology who recommended prednisone for symptom control and palliative salvage surgical resection of disease. He then underwent an uncomplicated right extrapleural pneumonectomy with diaphragm resection and reconstruction with an unremarkable postoperative course (Fig. 2). Final pathology revealed multiple foci of metastatic thymoma as well as a small focus of squamous cell carcinoma.
Postoperatively, he continued to have diarrhea, hyperhidrosis and lower extremity pain, but these were initially managed by continuing 10 mg prednisone daily. About 4 weeks after surgery, despite no evidence of recurrent disease on computed tomography, his symptoms of dysautonomia worsened, so, while weighing the risks of immunosuppression on wound healing and infection status, rituximab and methylprednisolone were started. His subsequent course was complicated by recurrent urinary tract infections and about 3 months after surgery he died from sepsis due to pyelonephritis.
DISCUSSION
Morvan syndrome is a subgroup of disease related to the CASPR2 protein that functions in proper localization of voltage-gated potassium channels in the nervous system [1, 3]. Patients with Morvan syndrome specifically develop anti-CASPR2 antibodies that lead to the syndrome’s classic features [3]. Greater than 80% are diagnosed in males and up to 25% of patients will have relapses [3]. While it has been associated with multiple tumor types, 40% of paraneoplastic Morvan syndrome cases are associated with thymoma, yet, it is seen in <1% of thymoma patients [1, 2, 4].
Onset of symptoms after thymoma resection have previously been reported and there is a theory that thymectomy and chemotherapy for thymoma may act as disease triggers due to antigens in thymic tumors [2]. However, the rate of clinical resolution of symptoms after tumor excision is unknown [4]. One case report documented complete resolution of symptoms within 48 h of surgical resection that was maintained with continued immunosuppression [4]. Other cases have reported symptom resolution after thymoma treatment with chemotherapy and radiation [5]. It is worth noting that Morvan syndrome-associated thymomas have a worse overall prognosis than recurrent thymomas or thymomas associated with myasthenia gravis [6]. The syndrome itself can be quite devastating and cases have been reported with fluctuating blood pressure which can occasionally be so extreme as to lead to death [7].
Our case represents one in which the thymoma not only recurred but also in which detection was preceded by the return of the associated paraneoplastic syndrome. This case also highlights the nuance associated with managing the syndrome’s potentially devastating symptoms while also attempting to treat the underlying malignancy. The perioperative continuation of steroids was necessary to keep symptoms manageable, but this likely contributed to our patient’s postoperative infection. Also, the eventual addition of rituximab and methylprednisolone made him more vulnerable to the urinary sepsis that led to his death further emphasizing the complexity of this disease process. Our case demonstrates that resection of metastatic disease is feasible with extrapleural pneumonectomy, but these patients remain at high risk of morbidity and mortality due to the immunosuppression required to control paraneoplastic symptoms.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.
References
- tachycardia
- hiv
- prednisone
- diarrhea
- syphilis
- methylprednisolone
- surgical procedures, operative
- thymectomy
- thymoma
- tremor
- antibodies
- diagnosis
- diagnostic imaging
- hyperhidrosis
- pleura
- rituximab
- dysautonomia
- lower limb pain
- urosepsis
- generalized illness
- parenchyma
- right lung
- extrapleural pneumonectomy
- morvan's disease



