-
PDF
- Split View
-
Views
-
Cite
Cite
Anzel Jansen van Rensburg, Marjan Ghadiri, A case report of superior mesenteric artery syndrome, Journal of Surgical Case Reports, Volume 2022, Issue 1, January 2022, rjab630, https://doi.org/10.1093/jscr/rjab630
Close - Share Icon Share
Abstract
Superior mesenteric artery (SMA) syndrome is a rare condition resulting in small bowel obstruction. The third part of the duodenum becomes compressed because of the narrow angle between the aorta and the SMA. Those at risk of developing SMA syndrome include patients who develop rapid weight loss, malignancy, eating disorders, burns, trauma and substance abuse. We present a case of a 73-year-old man that presented 5 days post a total hip replacement with abdominal pain and profuse bilious vomiting for 2 days. A computed tomography scan of his abdomen showed gross distension of his stomach with an abrupt occlusion of the duodenum at the level of the SMA which was consistent with SMA syndrome. The patient was treated conservatively and was later discharged from surgical services once his symptoms resolved and he was able to tolerate diet.
INTRODUCTION
Superior mesenteric syndrome is a rare cause of proximal small bowel obstruction. It results from the third part of the duodenum being compressed by the superior mesenteric artery (SMA) due to loss of the angle between the SMA and the aorta [1]. The SMA arises at the first lumbar vertebral level of the aorta where it is surrounded by adipose tissue and lymphatics. SMA syndrome is quite rare with prevalence in the literature reported as 0.1–0.3% with just over 400 cases described in the literature [1, 2]. The most common causes described include marked weight loss, anatomical variation, malignancy, eating disorder, burns, trauma and substance abuse [3, 4]. Common symptoms associated with SMA syndrome include nausea, vomiting and epigastric abdominal pain.
CASE PRESENTATION
A 73-year-old male was transferred from a private hospital to the local public hospital 5 days post left total hip replacement with a 2-day history of nausea, bilious vomiting and colicky abdominal pain. His bowels had not opened since prior to the procedure. His background included previous right total hip replacement, benign prostate hyperplasia and depression. His medications included mirtazapine, tamsulosin, calcium carbonate and denosumab. He is a non-smoker and does not drink alcohol. On examination his observations were all within normal limits and he appeared to be very slim build. His height was 174 cm and he weighed 49 kg with a body mass index of 16.2. His abdomen was generally tender and distended, but not peritonitic. His blood results showed a serum potassium of 3.2 mmol/L, sodium 148 mmol/L, magnesium 0.94 mmol/L, albumin 34 g/L, creatinine 104 μmol/L, eGFR 61 ml/min (acute kidney injury), white cell count 7.7 × 109/L, haemoglobin 114 g/L. A computed tomography (CT) scan of his abdomen (Figs 1–3) showed a grossly distended stomach measuring 26.2 cm × 14.3 cm × 14.6 cm. It appeared fluid filled with moderate distension of the first and second part of the duodenum. The third part of the duodenum was partly fluid filled with an abrupt luminal collapse within the distal aspect where it passes between the superior mesenteric artery and aorta. The aorta mesenteric angle was reduced to ~23°. The remaining small bowel was decompressed with no free fluid or gas.
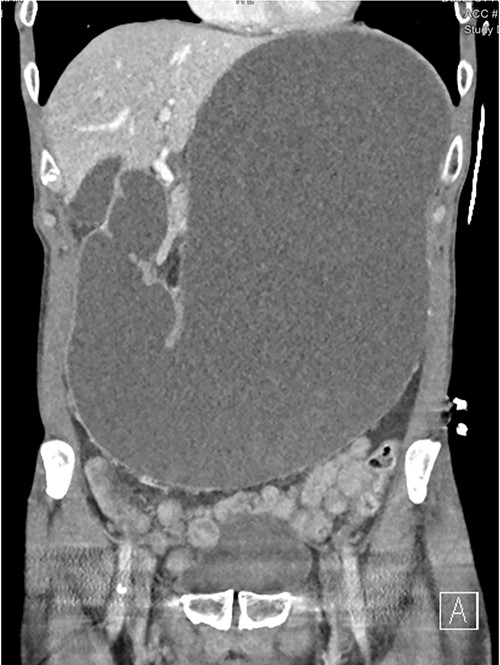
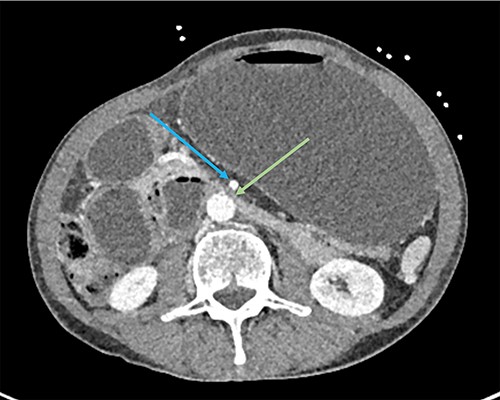
CT showing grossly distended stomach, first and second part of duodenum with sudden collapse and obstruction of duodenum (green arrow) at the superior mesenteric artery (blue arrow).

CT shows duodenum obstructed (orange arrow) between the aorta and superior mesenteric artery.
The patient was reviewed immediately, and a nasogastric (NG) tube was placed with 2.8 L of bilious fluid drained. The NG tube was placed on free drainage with 4 hourly aspirates. The patient was admitted and given aggressive intravenous fluid therapy and electrolyte replacement. An upper endoscopy showed a normal oesophagus, a few localized 3 mm non-bleeding erosions in the cardia of the stomach with a normal appearing duodenum and proximal jejunum. There was no evidence of any strictures or obstructing masses. A nasojejunal feeding tube was placed for enteral feeding. With regular dietician review enteral feeding was started and the rate was slowly increased until goal rate was reached. He was reviewed by General Medical Physician to ensure no other pathology was present. The patient was discharged home with enteral feeding as well as clear fluid diet. His diet was slowly increased to free fluid, soft diet and eventually normal diet as tolerated. Additional supplement protein drinks were also included to increase calorie intake. As his oral intake increased, the enteral feeding was decreased with regular dietician review. He was also reviewed in clinic every fortnight to ensure his weight continued to increase and to assess his diet progress. There were significant issues with recurrent blockage of his NJ tube requiring multiple admissions to unblock the tube and tube replacements. Eventually the decision was made, once the patient was able to tolerate more oral food, for ongoing oral diet and regular review. He continued to recover well and at his 3-month review, he had reached his normal weight of 54 kg, tolerating normal diet and denied any symptoms of SMA syndrome. He was subsequently discharged to his regular physician.
DISCUSSION
SMA syndrome is a rare cause of proximal small bowel obstruction resulting from compression of the third part of the duodenum by the SMA. Risk factors include rapid weight loss, malignancy, eating disorders, burns and substance abuse. Some studies have also shown a correlation with lying in supine position, trauma, spinal orthotics or high insertion of the duodenum at the ligament of Treitz [3–6].
The diagnosis involves CT imaging, barium swallow or contrast X-ray studies. The contrast studies show obstruction with failure of progression past the third part of the duodenum. CT imaging with vascular reconstruction allows the aortomesenteric angle to be measured. The normal aortomesenteric angle is 38–65° and the distance is 10–28 mm. An angle of <25° is considered the most sensitive diagnostic measure for SMA syndrome. The diagnosis is further supported if the aortomesenteric distance measures <8 mm [7, 8].
In our case, the angle was reduced to 23 mm and the distance 8.5 mm. Our patient reported always being of slim build, however, after having his hip replacement he spent a significant amount of time lying in his bed in supine position and likely decreased oral intake. This would have contributed to acute weight loss, predisposing him to the loss of the mesenteric fat pad.
SMA syndrome can be managed conservatively or with surgery. Conservative management involves gastric decompression, intravenous fluid and electrolyte replacement in the initial period followed by nutritional support which includes enteral feeding, TPN and slow oral diet. If conservative management fails, surgical treatment options should be considered. These include strong procedure where the duodenum is mobilized after dividing the ligament of trietz. The benefit of this is procedure is there is no bowel anastomosis, however, a 25% failure rate is reported [9]. Other surgical procedures include gastrojejunostomy and duodenojejunostomy with or without division of the fourth part of the duodenum. Gastrojejunostomy provides decompression however, it fails to relieve the obstruction which can result in return of symptoms. Duodenojejunostomy is the preferred procedure [2, 9].
SMA syndrome is a rare condition and controversy remains in the literature as to the diagnosis. Early recognition of the symptoms is important to allow early intervention and improve patient outcomes.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- aorta
- abdominal pain
- small bowel obstruction
- computed tomography
- substance abuse
- weight reduction
- cancer
- diet
- eating disorders
- burns
- dilatation, pathologic
- superior mesenteric artery
- superior mesenteric artery syndrome
- surgical procedures, operative
- wounds and injuries
- abdomen
- duodenum
- hip replacement arthroplasty
- stomach
- vomiting bile



