-
PDF
- Split View
-
Views
-
Cite
Cite
Wakako Kubota, Akihiro Sakuma, Ryuji Katada, Tomoya Nagao, Chiaki Murota, Usefulness of early diagnosis of small bowel obstruction due to broad ligament hernia using multidetector computed tomography: a case report, Journal of Surgical Case Reports, Volume 2022, Issue 1, January 2022, rjab598, https://doi.org/10.1093/jscr/rjab598
Close - Share Icon Share
Abstract
Small bowel obstruction due to broad ligament hernia (BLH) is a rare type of internal hernia. Preoperative diagnosis is difficult, as clinical symptoms and imaging results are often nonspecific. BLH has a high risk of strangulation and requires surgery for the reduction of herniated bowels. According to an analysis of 140 BLH cases reported in Japan, the typical patient is a middle-aged woman who has been pregnant and has no history of abdominal surgery and the characteristic computed tomography (CT) findings. This report will enable preoperative early diagnosis with our description of the typical patient with BLH and the characteristic CT findings. Tortuousness and dilation of the ovarian veins were noted in three cases, including in ours. This may be used as a new CT feature of early detection. Additionally, we report a case of BLH successfully treated after early diagnosis using multidetector CT.
INTRODUCTION
Small bowel obstruction (SBO) is a common condition encountered by radiologists in emergency departments. Internal hernia is uncommon, with a reported incidence of up to 3% of all cases of SBO. If strangulated and left untreated, internal hernia results in overall mortality >50% [1]. Broad ligament hernia (BLH) is a very rare type of internal hernia accounting for 4–5% of all of internal hernia cases [1]. Preoperative suspicion and diagnosis in the emergency setting are difficult because of the rarity of BLH, the nonspecific clinical presentation and limitations in imaging. There are still many cases that cannot be diagnosed preoperatively. For many cases, the patient is diagnosed with enteritis and simple bowel obstruction. Delayed diagnosis of a patient can lead to intestinal resection, peritonitis and even death [2–4]. Here, we report a case of BLH that was diagnosed early based on characteristic CT findings.
CASE REPORT
We present the case of a 46-year-old woman admitted to the emergency department of our hospital for acute lower abdominal pain that started 6 hours before admission.
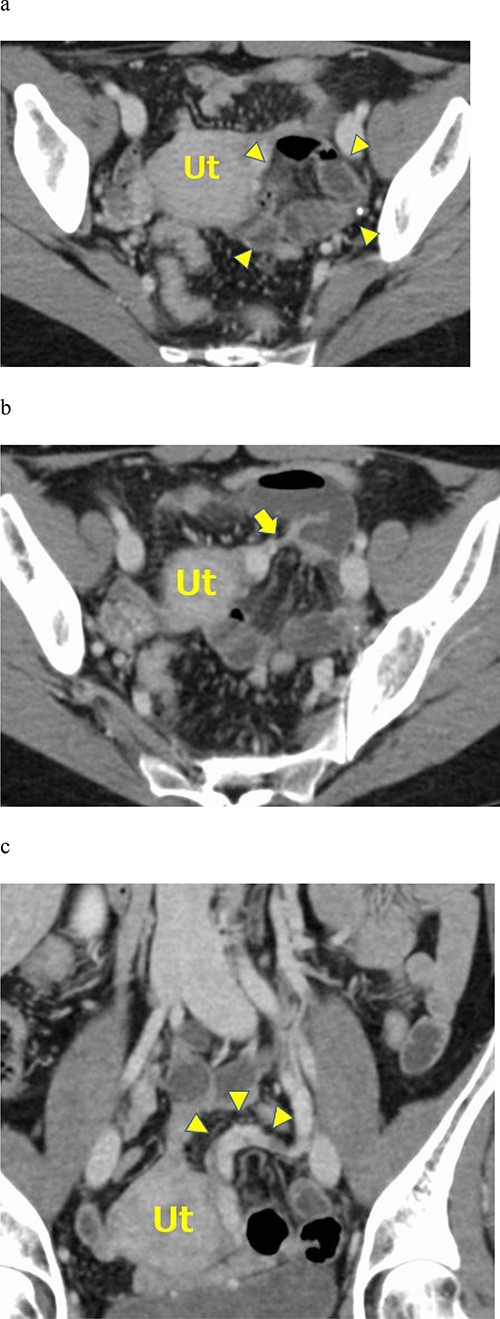
a. Contrast-enhanced axial CT showing fluid-filled dilated small bowel loops in the posterior pelvic cavity (arrowheads). The small bowel loops compressed the uterus on the right side. b. Contrast-enhanced axial CT showing mesenteric vessels converging around the uterus (arrow). c. Contrast-enhanced coronal CT images showing the left ovarian venous dilatation and tortuousness (arrowheads).
She had a history of three normal vaginal deliveries and no surgical history. In physical examination, her abdomen was slightly distended and showed diffuse tenderness; however, no rebound tenderness or muscular guarding was observed. Her heart rate and laboratory studies were normal.
An abdominal X-ray examination revealed no niveau formation. Abdominal contrast-enhanced computed tomography (CT) using a 320-row multidetector CT (MDCT) scanner (Aquilion ONE, Canon, Japan) was performed. The contrast-enhanced abdominal CT showed a cluster of dilated small bowel loops on the left side of the pelvic cavity and bowel loops compressing the uterus on the right side of the pelvis (Fig. 1a). The CT scan showed mesenteric vessels converging around the uterus (Fig. 1b). A small amount of ascites was found at Douglas’ fossa. Contrast-enhanced coronal CT images showed left ovarian venous dilatation and tortuousness (Fig. 1c). Enhancement of the wall of the small bowel loops was not decreased, indicating the absence of bowel ischemia.
Based on these MDCT findings, the patient was diagnosed with SBO due to incarceration through the left BLH. Emergency exploratory laparoscopy was performed. In the laparoscopic finding, there was no bloody ascites, small intestinal loop was dilated. Pulling out the small intestinal loop from incarceration revealed a defect of the left broad ligament (Fig. 2). The incarcerated intestine was congested and discolored. However, after the release, the intestinal color and peristalsis were improved and the intestinal resection was not performed. The defect was closed by sutures. Postoperative course was excellent and the patient was discharged 4 days after surgery.
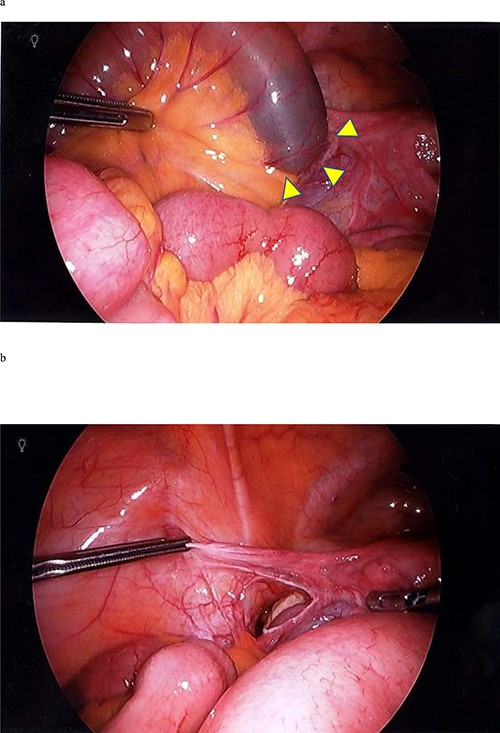
a. A laparoscopic image showing a fissure on the left side of the broad ligament. Arrowheads indicate the position where the small intestine entered. The oral side was dilated. b. A laparoscopic image showing a defect in the left broad ligament.
DISCUSSION
Internal hernia is rare, accounting for 0.5–3% of all SBO cases. Additionally, BLH is a rare type of internal hernia, accounting for 4–5% of all internal hernia cases [1]. According to a report by Baron, the first case was reported in an autopsy by Quain in 1861 [5]. Broad ligament defects are classified as congenital or acquired. Congenital cases have an embryologic basis due to a developmental peritoneal defect around the uterus. Acquired defects are due to surgical trauma, pregnancy and birth trauma, perforations following vaginal manipulation, or prior pelvic inflammatory disease [6].
Hunt classified two types of hernia through the broad ligament based on the degree of the defect (Fig. 3). One is the fenestra type, in which there is a defect in the broad ligament, and the other is the pouch type, where there is herniation into the anterior or posterior aperture of the broad ligament. More than 90% of cases, including our own, are of the fenestra type [6].
![Hunt’s classification divides the disease into fenestra and pouch types based on the nature of the hernial defects [6].](https://oupdevcdn.silverchair-staging.com/oup/backfile/Content_public/Journal/jscr/2022/1/10.1093_jscr_rjab598/1/m_rjab598f3.jpeg?Expires=1772429812&Signature=U3Imy8KSpvNHxzwFIctx0HCLHY29DZxCP2bip83HAs8rwWN~dgcgpIJJe0DgDSveWVj7WlPESi1Yf8vazCVPP2S0o8y3x6e68g7yU1lSE2BYrhbBjVhDoR-vflrsz~HQ6qvvGePlluiCFEZISF2HzPuBEmZ2~WGUn3Z0DO646gUfs61cBwO92FI7N9N2nsiXASI-NiEMePsdB78k2TOBppfsv9orB2VKIJWgDrRAuS16ZKio6LpG7i2VLat0fgrDGX66vsSnC27EINvycrxWAolNReizkp8Ui-MFD3dbPQlkt7vcwoKNrb5LK28KuGqAU3WVaZA4zNx0FCzvC~KWYg__&Key-Pair-Id=APKAIYYTVHKX7JZB5EAA)
Hunt’s classification divides the disease into fenestra and pouch types based on the nature of the hernial defects [6].
To date, the number of BLH cases reported in Japan has increased. This trend may be associated with technical advances of MDCT, the number of CT scans performed in Japan and wider recognition of BLH. We searched the literature using the Japan Centra Revuo Medical database, selecting ‘broad ligament’ and ‘hernia’ as keywords. We analyzed 140 cases reported in Japan (June 1993–March 2021), including our own, with CT findings. There have been no reports in the English and Japanese medical literature describing CT examination-based findings in >100 BLH cases.
The typical patient with BLH is a middle-aged woman (average 52 years, ranging in age from 23 to 94 years) who has been pregnant (92.0%) and has had no abdominal surgical history (75.6%). The patient reported here is the typical patient type (Table 1).
Patient characteristics, CT characteristics and preoperative diagnosis rate of 140 cases reported in Japan (June 1993–March 2021), including the case reported in this study
| Age (years) (mean) . | 23–94 (52.0) . |
|---|---|
| Pregnancy history (%) | 92.0 |
| No abdominal surgical history (%) | 75.6 |
| Hunt classified Fenestra type (%) | 92.0 |
| Computed tomography characteristics (%) | |
| (1) A dilated small bowel loop in the vicinity of the pouch of Douglas or uterus | 98.6 |
| (2) A shifted or compressed uterus, sigmoid colon, or rectum as a result of the small bowel loop | 89.9 |
| (3) Congested mesentery converging at the broad ligament, which is associated with the small bowel loop | 29.5 |
| Preoperative diagnosis rate (%) | 46.4 |
| Age (years) (mean) . | 23–94 (52.0) . |
|---|---|
| Pregnancy history (%) | 92.0 |
| No abdominal surgical history (%) | 75.6 |
| Hunt classified Fenestra type (%) | 92.0 |
| Computed tomography characteristics (%) | |
| (1) A dilated small bowel loop in the vicinity of the pouch of Douglas or uterus | 98.6 |
| (2) A shifted or compressed uterus, sigmoid colon, or rectum as a result of the small bowel loop | 89.9 |
| (3) Congested mesentery converging at the broad ligament, which is associated with the small bowel loop | 29.5 |
| Preoperative diagnosis rate (%) | 46.4 |
Patient characteristics, CT characteristics and preoperative diagnosis rate of 140 cases reported in Japan (June 1993–March 2021), including the case reported in this study
| Age (years) (mean) . | 23–94 (52.0) . |
|---|---|
| Pregnancy history (%) | 92.0 |
| No abdominal surgical history (%) | 75.6 |
| Hunt classified Fenestra type (%) | 92.0 |
| Computed tomography characteristics (%) | |
| (1) A dilated small bowel loop in the vicinity of the pouch of Douglas or uterus | 98.6 |
| (2) A shifted or compressed uterus, sigmoid colon, or rectum as a result of the small bowel loop | 89.9 |
| (3) Congested mesentery converging at the broad ligament, which is associated with the small bowel loop | 29.5 |
| Preoperative diagnosis rate (%) | 46.4 |
| Age (years) (mean) . | 23–94 (52.0) . |
|---|---|
| Pregnancy history (%) | 92.0 |
| No abdominal surgical history (%) | 75.6 |
| Hunt classified Fenestra type (%) | 92.0 |
| Computed tomography characteristics (%) | |
| (1) A dilated small bowel loop in the vicinity of the pouch of Douglas or uterus | 98.6 |
| (2) A shifted or compressed uterus, sigmoid colon, or rectum as a result of the small bowel loop | 89.9 |
| (3) Congested mesentery converging at the broad ligament, which is associated with the small bowel loop | 29.5 |
| Preoperative diagnosis rate (%) | 46.4 |
Several articles have reported the utility of CT findings since it was first described by Suzuki et al [7]. Based on our analysis of cases, BLH has the following characteristic CT findings: (1) a dilated small-bowel loop in the vicinity of the pouch of Douglas or uterus (98.6%); (2) a shifted or compressed uterus, sigmoid colon or rectum as a result of the small-bowel loop (89.9%) and (3) congested mesentery converging at the broad ligament, which is associated with the small -bowel loop (29.5%) (Table 1). All these characteristics were noted in the present case, which prompted our decision for early intervention and resulted in successful bowel rescue. The preoperative diagnosis rate is low at 46.4% (Table 1). There are still many cases that could not be diagnosed preoperatively [2–4]. For many cases, preoperative diagnosis was possible by looking at the MDCT images [4].
In our patient, MDCT images showed left ovarian venous tortuousness and dilatation. This may appear early by the small bowel loop compressing the round ligament, which has ovarian blood vessels. Tortuousness and dilation of the ovarian veins were noted in three cases, including ours [4]. This may be used as a new CT feature for early detection.
CONCLUSION
BLH has a high risk of strangulation and requires surgery for the reduction of the herniated bowels. Preoperative diagnosis of BLH is typically difficult. However, we want to point out that the typical patient with BLH is a middle-aged woman who has been pregnant and has no history of abdominal surgery. Additionally, using advanced imaging techniques, such as MDCT, can enable a preoperative early diagnosis.



