-
PDF
- Split View
-
Views
-
Cite
Cite
Thomas Kotsis, Panagitsa Christoforou, Andreas Polydorou, The contribution of oncovascular surgery in a young patient with idiopathic retroperitoneal fibrosis, Journal of Surgical Case Reports, Volume 2022, Issue 1, January 2022, rjab589, https://doi.org/10.1093/jscr/rjab589
Close - Share Icon Share
Abstract
Surgical resection remains the cornerstone for the treatment of oncological disease. When a critical arterial or venous structure is involved in a tumor mass, successful relief of symptoms and long-term oncological control are achieved through careful preoperative planning by an interdisciplinary team that necessarily includes a vascular surgeon. We describe the involvement of a vascular surgeon in the oncology of a 22-year-old woman, who is diagnosed with idiopathic retroperitoneal fibrosis.
INTRODUCTION
Complete surgical resection remains the cornerstone of treatment for most malignancies. The purpose is to provide vascular resection exclusions for limb sarcoma, retroperitoneal sarcoma or pancreatic cancer. Radical surgical resection may offer a unique opportunity for treatment or relief for these patients. Here we report the involvement of the vascular surgeon in oncological surgery of a 22-year-old woman with idiopathic retroperitoneal fibrosis (RPF).
CASE REPORT
A 22-year-old with a history of polycystic ovaries and mesenteric resection, 6 months ago, was hospitalized for flatulence, indigestion, vomiting, anorexia and weight loss. He underwent computed tomography (CT) of the abdomen (Fig. 1), where a mass encloses the abdominal aorta and the arterial and venous axes as well as the right ureter. During the operation, a peritoneal tumor mass was found, which surrounds the lower part of the abdominal aorta and the pelvic vessels. A rapid biopsy was sent and the response to Castleman’s disease surprised the surgical team, who requested a vascular surgeon to be present. The mass was removed from the vessels, followed by appendicectomy and resection of the aortic lymph nodes (Fig. 2). The patient had a normal postoperative course and left the hospital on the fourth day after the operation.
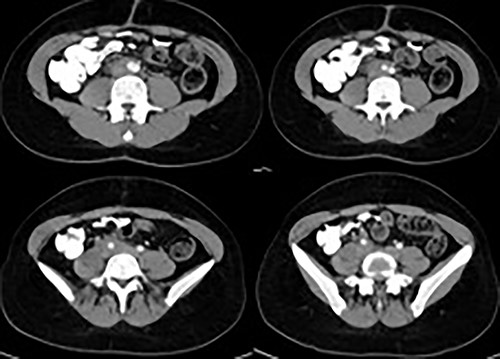
CT of the abdomen revealed a mass encloses the abdominal aorta and the arterial and venous axes as well as the right ureter.

During the operation, the mass was detached from the abdominal aorta and common iliac arteries and veins.
The final pathology report showed fibrosclerotic disease in the context of idiopathic retroperitoneal fibrosis that developed during the retroperitoneal development phase.
DISCUSSION
Posterior peritoneal fibrosis is a rare disease characterized by fibrotic lesions infiltrated by chronic inflammatory cells around the abdominal aorta and the common iliac arteries surrounding the ureter and causing obstructive uropathy. There is no specific etiology for more than 70% of retroperitoneal fibrosis classified as idiopathic, which includes inflammatory AAA, chronic periarthritis and perineural fibrosis. The incidence is approximately 1:100 000 persons and the mean age is 60 years, while men are more vulnerable [1]. There have been reported cases at younger ages, especially in the third and fourth decades of life and even in children [2].
Idiopathic RPF typically surrounds the aorta and iliac arteries; stenosis of the arteries is rare, on the contrary, venous pressure is common, especially the inferior vena cava and can cause lower limb edema, while inferior vena cava syndrome, deep vein thrombosis and pulmonary embolism are uncommon, due to development of collateral circles. Also, periaortic tissue can expand to the mesenteric and celiac arteries, causing stenosis and ischemic complications, like mesenteric vasculitis [3–5]. Idiopathic RPF is usually diagnosed by CT, which detects the typical anatomical feature ‘the mantle sign’ or magnetic resonance imaging (MRI) [3, 6, 7].
The involvement of major vascular structures should not be an obstacle to en bloc exclusion, with the aim of therapeutic surgery of neoplasms. Vascular restorations do not increase the frequency of postoperative complications. Survival depends on the complete removal of the primary pathology and the biology of neoplasia and not on the complications associated with the vessels. An aggressive approach is needed with the cooperation of many experts and excellent preoperative planning. Vascular surgeons must demonstrate a leading position in cancer surgery in cases of the complex oncological disease, with the participation of vascular structures. The modern practice of cancer surgery requires the collaboration of vascular surgeons. The role of the vascular surgeon is extremely beneficial with his participation as a consultant of the interdisciplinary team in the preoperative combination in cancer surgery or as a primary surgeon in tumors related to blood vessels but also as a surgeon who rescues vascular complications during the operation [8–10].
The term ‘oncovascular surgery (OVS)’ is rarely used. A Google search found only 6 articles and 2 medical centers using this term till last year. The timely use of this term OVS can increase awareness of the importance of the vascular surgeon's role in complex surgeries. This can be seen from the increase in articles published on this topic, according to a current Google search [11]. The OVS refers to cancer resection with simultaneous ligation or reconstruction of a large vascular structure. An extensive understanding of tumor biology, preoperative planning, knowledge of vascular surgery techniques and multidisciplinary collaboration are required [12].
CONCLUSION
Surgical resection remains the cornerstone for the treatment of oncological disease. When a critical arterial or venous structure is involved in a tumor mass, successful relief of symptoms and long-term oncological control are achieved through careful preoperative planning by an interdisciplinary team that necessarily includes a vascular surgeon.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.
ACKNOWLEDGEMENTS
The authors declare that there is patient’s consent regarding the publication of this paper.
The authors declare that this study has been approved by the ethical committee.
Study Conception, Investigation, Writing: Thomas Kotsis, Panagitsa Christoforou.
Data Collection, Analysis: Thomas Kotsis, Panagitsa Christoforou, Andreas Polydorou.
Critical Review and Revision: All authors.
Final Approval of the Article: All authors.



