-
PDF
- Split View
-
Views
-
Cite
Cite
Heerani Woodun, Heyrumb Woodun, Neeraj Sethi, Anthony Simons, Idiopathic hypopharyngeal perforation presenting as supraglottitis and parapharyngeal abscess: case report and literature review, Journal of Surgical Case Reports, Volume 2022, Issue 1, January 2022, rjab569, https://doi.org/10.1093/jscr/rjab569
Close - Share Icon Share
Abstract
A 75-year-old healthy male reported odynophagia and severe neck pain with radiation to chest and shoulders. Cardiac causes were excluded. After re-presenting with dysphonia and complete dysphagia, he was treated for supraglottitis. Imaging showed a left parapharyngeal and retropharyngeal space abscess with mediastinal emphysema. Progressive emphysema prompted contrast swallow test followed by left neck exploration and pan-endoscopy, which confirmed mucosal hypopharyngeal perforations. Histopathology reported inflammation. Autoimmune and gastroenterological aetiologies were excluded. Following conservative management, healing was demonstrated on repeat pan-endoscopy. Two months’ follow-up imaging showed complete resolution. Spontaneous hypopharyngeal perforation, atypical of Boerrhave’s syndrome and without risk factors (iatrogenic, oesophageal disease and foreign body ingestion), is rare and often misdiagnosed, including masquerading as supraglottitis. Nasoendoscopy should be complemented by radiological imaging. Presence of deep neck space collections and surgical emphysema should prompt diagnostic pan-endoscopy. Although most rupture cases require surgery, conservative management of hypopharyngeal perforations can be considered when clinically appropriate.
INTRODUCTION
Hypopharyngeal and oesophageal ruptures are infrequent but more commonly occur during diagnostic or therapeutic endoscopic procedures, due to trauma, intrinsic diseases and foreign body ingestion [1]. Presentations can be non-specific depending on the location of the rupture and time of presentation including chest pain, dyspnoea and fever or more severe features of mediastinitis or sepsis. Management depends on clinical stability, site of perforation, extent of contamination, pre-existing disease and patient co-morbidities [1].
We present a rare case of conservatively-managed idiopathic hypopharyngeal perforation in a 75-year-old male who received a delayed diagnosis following invasive diagnostic procedures after reporting initial non-specific followed by laryngological symptoms.
CASE REPORT
A 75-year-old healthy male presented to the emergency department (ED) with severe neck pain radiating to his chest and shoulders, associated with 5 days’ history of odynophagia and partial dysphagia in the absence of trauma, vomiting and foreign body ingestion. He was discharged after acute coronary syndrome was excluded. He re-presented to ED with dysphonia and complete dysphagia and was referred to the otolaryngology team.
Examinations of the respiratory and cardiovascular systems were unremarkable. Neck examination revealed surgical emphysema. Flexible nasoendocopy (FNE) showed inflamed aryepiglottic folds. He was treated for supraglottitis with intravenous Meropenem and Metronidazole and was kept nil by mouth.
Full blood count, renal function and coagulation profile were within normal limits. C-Reactive protein was mildly raised at 73 mg/l. Neck axial contrast enhanced computer tomography (CT) scan was consistent with significant paraesophageal gas and mediastinitis (Fig. 1). Magnetic resonance imaging (MRI) suggested an enhancing collection from the left parapharyngeal space extending to the mediastinum (Fig. 2). Intravenous Fluconazole was added.

Sagittal plane CT neck and thorax with oral contrast showing significant parapharyngeal gas.
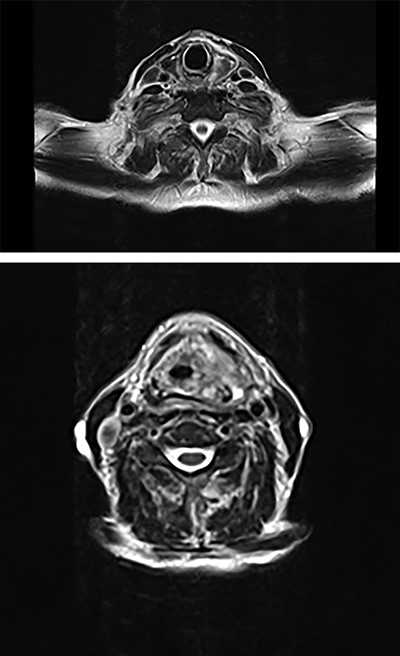
Axial plane MRI of neck and thorax showing a heterogenous collection on left parapharyngeal space extending inferiorly.
He was transferred to the tertiary Head & Neck Unit (10 days after his initial presentation) where dysphagia and surgical emphysema persisted. Repeat FNE showed inflamed aryepiglottic folds and pooling of saliva in the piriform fossa and ineffective swallow. Chest plain radiography showed small bilateral pleural effusions and minor pneumomediastinum. Coronavirus disease of 2019 was negative.
Intravenous Meropenem, Metronidazole and Fluconazole were continued, and he remained nil by mouth with nasogastric tube feeding. Water-soluble contrast swallow was undertaken after repeat CT showed emphysema progression (Fig. 3). A left sided oropharyngeal perforation was suggested.
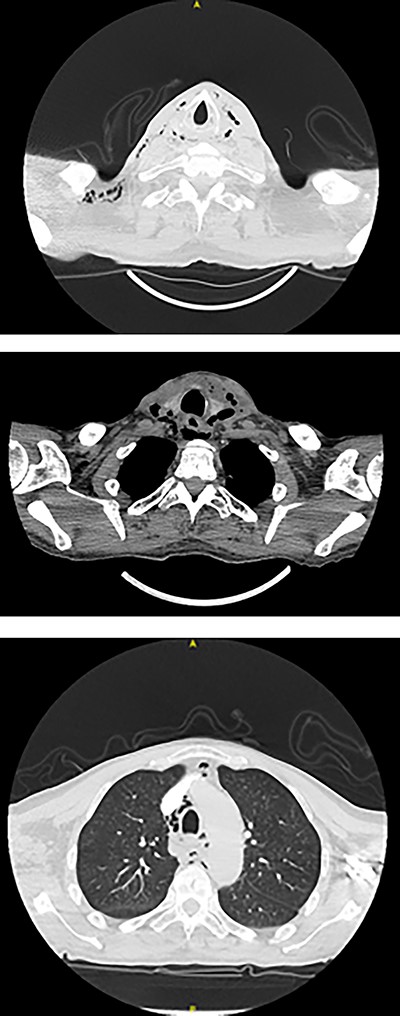
Axial planes CT neck and thorax showing left parapharyngeal abscess with tracking into the prevertebral space, significant progression of air pockets in mediastinal and cervical soft tissue extending to right axillary region.
Subsequent pan-endoscopy and neck exploration confirmed multiple slit-like four or five mucosal perforations in left posterior pharyngeal wall and left piriform fossa with muco-purulent discharge (Fig. 4). Two corrugated drains, one directed inferiorly towards pharynx and one superiorly, were secured. Histology of tissue biopsy confirmed acute and chronic inflammation with granulation, which was negative for dysplasia, malignancy and cytomegalovirus, fungal, acid-fast bacilli infections. No microbial growth was obtained from culture.
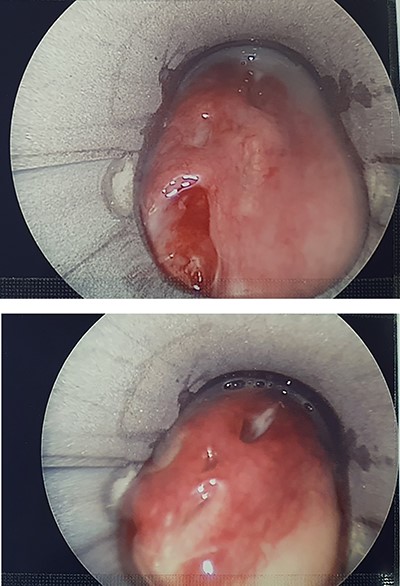
Pharyngoscopy showing slit-like mucosal perforations in left posterior pharyngeal wall and left piriform fossa with muco-purulent discharge.
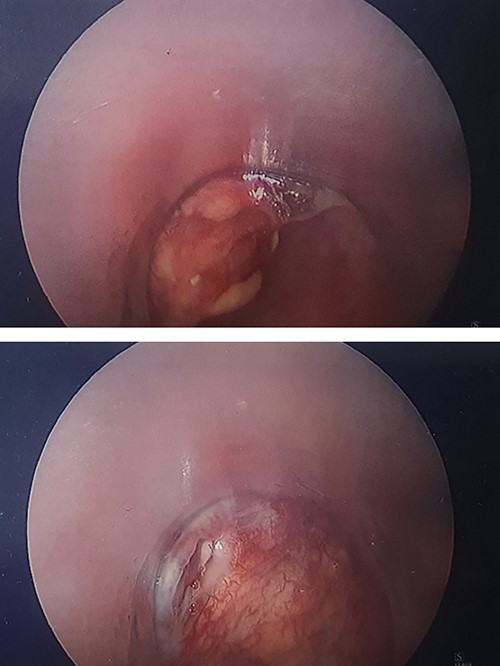
He was managed conservatively. Two days post-operatively, surgical emphysema had resolved and there was minimal drain output. Contrast swallow 6 days post-operatively showed aspiration and repeat pharyngoscopy, 10 days post-operatively, showed healing perforations (Fig. 5).
Inflammatory bowel disease and autoimmune diseases were excluded. He received a trial of dexamethasone and proton-pump inhibitors. After discussion with microbiologists, he completed a 3 weeks’ course of antibiotics and antifungals. Subsequent swallowing assessment showed no signs of aspiration and contrast swallow showed complete resolution. MRI at 4 weeks after discharge indicated complete resolution of perforations and the patient resumed his baseline status.
DISCUSSION
Literature about spontaneous hypopharyngeal ruptures is sparse. The aetiology of this case is uncertain. Foreign bodies can cause cervical oesophagus perforation [1]. Iatrogenic causes include endoscopic or surgical manipulation [1], endotracheal intubation [2] and laryngeal mask airway placement [3]. Koscienlny et al. [2] reports cases presenting with dysphagia, surgical emphysema, pyrexia, leucocytosis and another with increasing dysphagia and an initial diagnosis of retropharyngeal abscess. Both cases required surgery and antibiotics for iatrogenic perforation.
Other case reports include a 30-year-old male who sustained a fistula of the piriform sinus after sneezing while obstructing both nostrils leading to cervical subcutaneous emphysema and pneumomediastinum. He was managed conservatively [4]. A 49-year-old female underwent open repair and stenting for a hypopharyngeal and cervical oesophageal perforation after an initial diagnosis of retropharyngeal abscess. She had presented twice with odynophagia and dysphagia after an episode of yelling [5]. A 56-year-old female reported right sided severe chest pain after eating two mouthfuls of vegetables and a contrast swallow demonstrated a large tear in the mid-oesophagus, features of achalasia and mediastinal contamination. She underwent a three-stage oesophagectomy with an uneventful recovery [6].
Our patient did not undergo any procedures and denied foreign body ingestion, episodes of emesis, yelling or other activities causing increases of pressure in the larynx.
This case is also atypical of Boerrhave’s syndrome, which represents 15% of all oesophageal ruptures [7]. The lower third of the oesophagus in the left lateral position is usually involved due to anatomical weakness and a sudden increase in intraluminal oesophageal pressure, commonly after persistent vomiting [8].
It is important to exclude intrinsic diseases including malignancy [1, 8] and rheumatological conditions. This case study patient did not have personal or family history of rheumatological conditions; vasculitis screen was negative and histopathology did not indicate malignancy.
Late presentation, delayed diagnosis and misdiagnosis result in significant morbidity and mortality rates, from 10 to 50% [9]. Contained oesophageal perforations can be more challenging to diagnose as patients have mild symptoms compared with oesophageal ruptures [5]. In our case, delayed diagnosis was related to treatment of supraglottitis and parapharyngeal abscess with initial discharge from the referring unit prior to re-presentation.
Nasoendoscopy can be helpful in diagnosing supraglottitis and pharyngeal abscesses, but CT should follow and pan-endoscopy should be undertaken if surgical emphysema is present as this may result from a perforation which has caused an abscess.
Most of the literature discusses management of oesophageal perforation which is mostly surgical with pleural or mediastinal drainage (presentation within 48 h with sepsis; [8]), endoscopic interventions in non-septic patients with minimal contamination [1, 7, 8] or conservative approach with antibiotics and percutaneous drainage of abscesses for patients presenting after 48 h with no sepsis [1, 4, 7, 8]. A hybrid combination of endoscopic and minimally invasive surgery to drain collections and place stents has also been proposed [10]. In our case of hypopharyngeal perforation, there is limited literature and management is mostly conservative.
Perforation should be considered if patients present with non-specific symptoms. It is primordial to minimize delay in treatment due to high morbidity and mortality (up to 50%) of hypopharyngeal and oesophageal rupture and complications of intrathoracic infections and sepsis [9]. Nasoendoscopy should be complemented by radiological imaging as perforations can masquerade as supraglottitis. Presence of deep neck space collections and surgical emphysema should prompt diagnostic pan-endoscopy. Although most oesophageal rupture cases require surgical repair, hypopharyngeal perforations are managed conservatively when clinically appropriate.
CONFLICT OF INTEREST STATEMENT
There is no conflict of interest to declare.
References
- inflammation
- deglutition disorders
- esophageal diseases
- endoscopy
- abscess
- autoimmunity
- follow-up
- mediastinal emphysema
- neck pain
- rupture
- surgical procedures, operative
- diagnosis
- diagnostic imaging
- emphysema, pulmonary
- heart
- hypopharynx
- mucous membrane
- shoulder region
- chest
- swallowing painful
- dysphonia
- retropharyngeal area
- supraglottitis
- parapharyngeal abscess
- neck spaces
- foreign body, swallowed
- misdiagnosis
- endoscopy of nose
- conservative treatment
- histopathology tests
- contrast swallow
- neck exploration



