-
PDF
- Split View
-
Views
-
Cite
Cite
Sung Hyun Kim, Sejin Park, Jangkyu Choi, A cystic artery arising from the middle hepatic artery detected during laparoscopic cholecystectomy: a case report, Journal of Surgical Case Reports, Volume 2022, Issue 1, January 2022, rjab088, https://doi.org/10.1093/jscr/rjab088
Close - Share Icon Share
Abstract
We herein report a case in which a cystic artery arising from the middle hepatic artery (MHA) was encountered during cholecystectomy. A 42-year-old man visited the outpatient department complaining of chronic epigastric pain and a laparoscopic cholecystectomy was decided upon. During the preoperative evaluation, an interesting finding was observed on computed tomography. The patient had a cystic artery arising from the MHA. An MHA derived from the hilum of the proper hepatic artery runs along the medial border of the gallbladder and enters segment IV. In the operative field, the MHA that entered segment IV was observed. Dissecting downward along the MHA, a cystic artery was observed around the cystic duct. The cystic artery and duct were isolated and each was separately ligated and cut. Rare anatomical variations of the cystic artery, as in this case, can be a pitfall inducing complications during cholecystectomy.
INTRODUCTION
Laparoscopic cholecystectomy is accepted as a standard surgical procedure for the management of benign gallbladder diseases and <0.5% of complications have been reported in recent data [1]. One of the risk factors inducing complications is anatomic variation [2]. These variations are common in the general population and can lead to iatrogenic damage of biliary ducts or aberrant vessels. Therefore, a thorough understanding of the relevant anatomy is important. Several uncommon anatomic variations around the gallbladder have been previously reported [2–4]. Here, we present a case in which a cystic artery arising from the middle hepatic artery (MHA) was observed during cholecystectomy.
CASE REPORT
A 42-year-old man visited the outpatient department complaining of chronic epigastric pain for the past 1 year, without surgical or medical history. The frequency and severity of epigastric pain had increased since 6 months. Ultrasonography revealed gallbladder wall thickening with stones, indicating chronic cholecystitis, and it was decided to perform laparoscopic cholecystectomy. During the preoperative evaluation, an interesting finding was observed on computed tomography. The patient had a cystic artery arising from the MHA (Fig. 1A). An MHA derived from the hilum of the proper hepatic artery runs along the medial border of the gallbladder and enters segment IV (Fig. 1B).
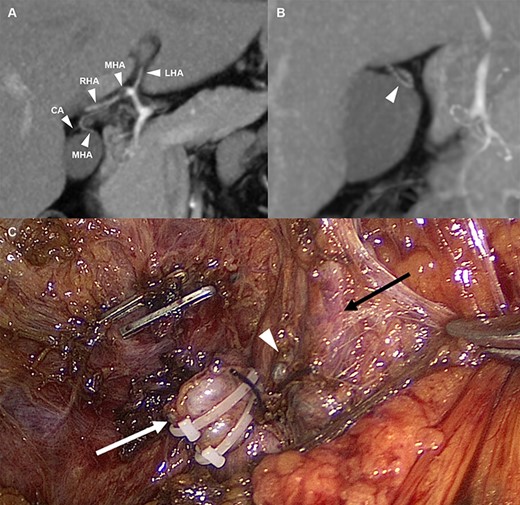
(A) Arterial anatomy; the MHA derived from the hilum of the hepatic artery and the CA arising from the MHA (B) The MHA that runs into segment IV (C) Anatomical structures after cholecystectomy; white arrow: cystic duct stump, white wedge: CA stump, and black arrow: MHA. LHA, left hepatic artery; MHA, middle hepatic artery; RHA, right hepatic artery; CA, cystic artery.
Keeping in mind this anatomical variation, laparoscopic cholecystectomy was performed. Moderate adhesion around Calot’s triangle was observed due to previous colic attacks. The omentum, round ligament and gallbladder were adhered to each other, and it was difficult to separate each of them. After careful dissection of the medial border of the gallbladder, the MHA that ran to segment IV was observed. Dissecting downward along the MHA, a cystic artery was observed around the cystic duct. The cystic artery and duct were isolated and each was separately ligated and cut. The gallbladder was detached from the liver and hemostasis was achieved. After insertion of a drainage catheter into the subhepatic space, abdominal closure was performed. The patient was discharged on postoperative Day 5 without any adverse events.
DISCUSSION
Although ~80% of cystic arteries arise from the right hepatic artery, there are many origins of the cystic artery, such as the proper hepatic artery, left hepatic artery, common hepatic artery, gastroduodenal artery, celiac artery and superior mesenteric artery. These variations account for ~1–2% [2]. In addition, several rare sites have been reported [3, 4].
The MHA is a hilar artery that supplies blood to segment IV [5]. The MHA is present in ~15% of the population; therefore, a cystic artery arising from the MHA is an extremely rare occurrence [5]. Reviewing previous articles, one case reported in a cadaver was found that was similar to the present case [3]. However, the site of origin was different, with the MHA originating as a branch of the right hepatic artery. On the contrary, the present case had a normal hepatic artery configuration.
Three arteries, namely, the right, middle and left arteries are involved in the embryonic development of the liver. In its developmental stages, these arteries act as hepatoenteric vessels and supply nutrition to organs through hepatoenteric circulation. The inferior branches of the left and middle arteries develop into the left gastric artery and gastroduodenal artery, respectively. As development progresses, the right and left arteries play a dominant role in enteric organs, and the middle artery plays a dominant role in the liver. Finally, the three arteries are anastomosed in the hilum of the liver. During this stage, the gallbladder and cystic duct develop from the pars cystica, and the cystic artery arises from the right branch of the middle artery [5]. Because of this, the cystic artery can exhibit various origins.
Therefore, every surgeon should keep in mind the rare possibility of anatomical variation encountered during cholecystectomy. In this case, the MHA mimicked a branch of the cystic artery. There is a high possibility of causing iatrogenic damage to MHA, if such anatomic variations are left unconsidered. Fortunately, in the present case, a preoperative assessment of the anatomical structures aided in avoiding any specific complications while performing cholecystectomy.
In conclusion, a rare anatomical variation of the cystic artery, as in this case, can be a pitfall inducing complications during cholecystectomy. Surgeons are needed to understand the relevant anatomy before laparoscopic cholecystectomy.
CONFLICT OF INTEREST STATEMENT
The authors declare that there is no conflict of interest.
FUNDING
None.



