-
PDF
- Split View
-
Views
-
Cite
Cite
Tia Morosin, M Shella De Robles, Chylous ascites as a marker for intestinal viability in a small bowel obstruction: a case report, Journal of Surgical Case Reports, Volume 2021, Issue 9, September 2021, rjab411, https://doi.org/10.1093/jscr/rjab411
Close - Share Icon Share
Abstract
Chylous ascites (CA) is the uncommon extravasation of triglyceride-rich fluid into the abdominal cavity as a result of the disruption of the abdominal lymphatic system. A patient who had previously undergone a subtotal colectomy presented with a closed-loop small bowel obstruction (SBO), underwent an emergency laparotomy with adhesiolysis and had intra-operative findings of milky intra-abdominal free fluid confirmed on analysis as CA. His post-operative period was complicated by a prolonged ileus, and following resolution, he was subsequently discharged home. Here, we present a case of a closed-loop SBO in which CA may be an indicator of intestinal viability.
INTRODUCTION
Chylous ascites (CA) is the uncommon extravasation of triglyceride-rich fluid into the abdominal cavity, typically occurring as a result of malignancy, surgery or trauma due to disruption of the abdominal lymphatic system [1, 2]. While CA has been reported acutely post-colorectal cancer resection, to our knowledge, this is the first case reported as a result of an adhesional small bowel obstruction (SBO) in a patient with preceding history of colorectal cancer.
CASE REPORT
A 52-year-old man presented with a 1-day history of generalized abdominal pain, distension and vomiting. Two years prior, he underwent a subtotal colectomy for colorectal cancer associated with Lynch syndrome and adjuvant chemotherapy. He was haemodynamically stable on presentation. Examination revealed a soft abdomen with marked distension and left periumbilical tenderness, however, no peritonism. Biochemistry showed lactate: 1.9, white cell count: 17 and C-reactive protein: 10. Computed tomography (CT) abdomen demonstrated a closed-loop SBO with transition point mid-abdomen, free fluid but no free gas (Figs 1 and 2). The patient was resuscitated with intravenous fluids, a nasogastric tube was inserted and they proceeded to an exploratory laparotomy for the closed-loop SBO. Intra-operative findings noted a loop of distended small bowel adherent to the anterior abdominal and pelvis side walls, with a loop of ileum twisted at the mesentery secondary to a band adhesion causing the closed-loop obstruction. The patient underwent adhesiolysis and untwisting of the mesentery, which demonstrated viable ileum with no evidence of perforation. In addition, the liver was smooth, there was no evidence of peritoneal metastases and the previous side-to-side ileo-sigmoid anastomosis was intact with no evidence of stricture or cancer recurrence. Lastly, milky intra-abdominal fluid was noted intra-operatively, with a sample sent for biochemistry showing a triglyceride level of 1584 mg/dl indicative of CA. Post-operative recovery was delayed by a prolonged ileus for which they were commenced on total parenteral nutrition (TPN) and slowly upgraded to a low-fat diet following resolution of the ileus. They were discharged home on Day 49 post-operatively.
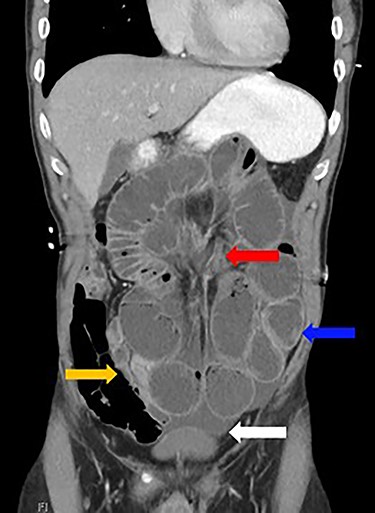
Dilated loops of small bowel (blue arrow), oedematous mesentery (suggestive of closed-loop obstruction; red arrow), free fluid (evidence of CA; white arrow) and collapsed small bowel (orange arrow)
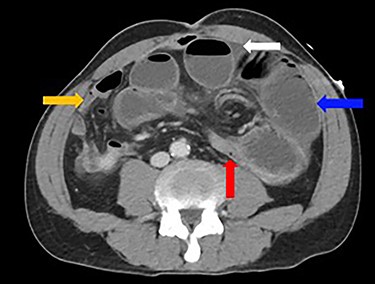
Dilated loops of small bowel (blue arrow), transition point (red arrow), free fluid (evidence of CA; white arrow) and collapsed small bowel (orange arrow).
DISCUSSION
CA is a rare condition characterized by the presence of lymphatic fluid within the abdominal cavity. The frequency of cases is difficult to determine, given the rarity of presentation; however, studies have indicated incidence of 1 in 11 589 [3]. While uncommon, the prognosis is poor, with mortality rates of 70–90% [3]. Underlying aetiology contributes most significantly to mortality and includes congenital or acquired, specifically neoplastic, inflammatory, post-operative and traumatic [3]. Malignancy is the most common cause of CA (25%) in adults, with children showing greater affinity for lymphatic abnormalities (84%; [1, 3, 4]). Numerous theories for CA have been proposed, including (i) injury to lymphatic vessels secondary to trauma or surgery, (ii) malignant or metastatic invasion of lymph nodes and lymphatic channels causing duct occlusion and chyle leakage and (iii) exudation from dilated lymphatics in the bowel wall and mesentery as a result of obstruction [1, 2, 3, 5]. Post-operative cases typically develop 1 week to month post-surgery due to damage of lymphatic vessels intra-operatively. While noted most commonly post-abdominal aortic and pelvic surgery (including lymphadenectomy for testicular, renal and gynaecological malignancies), few cases of chyloperitoneum have been reported post-colorectal surgery. One study reported nine cases of CA associated with colorectal cancer over a 3-year period, deemed likely secondary to intra-operative lymphatic injury [6]. While the incidence of CA during the study was 1%, it should be interpreted with caution due to the small sample number. Chan et al. also reported CA post-neoadjuvant radiotherapy and anterior resection for rectal cancer, however, the patient presented symptomatic with metastatic adenocarcinoma 2 years post-surgery. In this circumstance, delayed presentation of CA was attributed to either obstructed lymph channels as a result of radiotherapy or metastatic lymphadenopathy [7]. While the current case notes similarities, given the presentation, history and lack of metastatic disease, the chyloperitoneum was likely secondary to exudation of chyle from the bowel wall and mesentery as a result of closed-loop SBO secondary to adhesions rather than a history of malignancy. The association of SBO and CA is rare with a limited number of cases reported to date. Akama et al. and Koyama et al. both reported cases of CA associated with volvuli secondary to a Petersen’s hernia and internal hernia (post-gastrectomy with Roux-en-Y), respectively. Interestingly, both cases reported intestinal viability intra-operatively with no resection required. Furthermore, both studies hypothesized that CA associated with SBO may be an indication of intestinal viability, as veins and lymphatics operate at a lower pressure system and are the first to be occluded during a bowel obstruction, while arterial supply is required for lymphatic production and CA accumulation [8, 9]. In addition, Akama et al. identified eight cases of CA associated with a SBO, all who underwent surgical intervention. All cases demonstrated bowel viability without the need for an enterectomy during surgery supporting the hypothesis that CA is an indicator of intestinal viability [8–11]. Clinical presentation includes abdominal distension with or without pain, nausea, anorexia, dyspnoea and oedema [1, 2, 4, 5]. CT abdomen scan is useful in assisting diagnosis of SBO, intra-abdominal lesions, the exclusion of haemoperitoneum and the presence of CA, given its similar density to water [1, 9]. In the present case, CT scan demonstrated a closed-loop SBO with evidence of free fluid that was indistinguishable from water. Elevated fluid triglyceride levels >110 mg/dl are widely recognized as diagnostic for CA [1, 2]. The combination of CT and intra-operative findings, with the fluid triglyceride level, were sufficient to diagnose our patient with CA. Treatment of the underlying aetiology is vital for the management of CA. Our patient underwent a laparotomy and division of adhesions given the presence of a closed-loop obstruction. Intra-abdominal accumulation of chyle can result in the loss of proteins, electrolytes, water and vitamins, highlighting how essential adequate nutritional replacement is for the management of CA. Our patient required surgical intervention for resolution of the underlying SBO with TPN dietary supplementation for a prolonged post-operative ileus after which they were transitioned to an unrestricted diet. CA is uncommon and is typically associated with malignant disease. Here, we have described a case of CA associated with an adhesional SBO.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



