-
PDF
- Split View
-
Views
-
Cite
Cite
Melanie Mercado, Jason Diab, Ken Loi, A delayed diagnosis of obturator hernia hoodwinked by previous laparoscopic inguinal hernia repair, Journal of Surgical Case Reports, Volume 2021, Issue 9, September 2021, rjab407, https://doi.org/10.1093/jscr/rjab407
Close - Share Icon Share
Abstract
Obturator hernia is a rare and diagnostically challenging type of pelvic hernia with associated high morbidity and mortality. It is frequently seen in frail, elderly female multiparous patients with non-specific symptoms and signs that may be clouded by multiple gastrointestinal or musculoskeletal comorbidities. This report discusses the case of an 84-year-old woman with refractory groin pain and previous laparoscopic inguinal hernia repair that was misdiagnosed leading to a delayed diagnosis and mortality. Previous laparoscopic repair was a misleading factor that hoodwinked clinicians and surgeons until computed tomography (CT) imaging proved otherwise. In emaciated, elderly female patients presenting with non-specific abdominal or hip pain, early CT imaging can assist in diagnosis when signs or symptoms are unclear. Clinical vigilance and serial examination are important in elderly patients who are often under the care of geriatricians allowing early discovery and treatment of this hernia.
INTRODUCTION
Obturator hernia is a rare type of pelvic hernia presenting with non-specific signs and symptoms. The obturator canal traverses the superior part of the obturator foramen, containing the obturator nerve and vessels. The hernia sac usually contains small bowel resulting in intestinal obstruction, but other contents such as the appendix or bladder may traverse. It ranges from 0.073 to 2.2% of all hernias, and most patients are elderly, multiparous females, hence called the ‘little old lady’s hernia’ [1]. It is often confirmed by computed tomography (CT) with features of a small bowel obstruction secondary to incarceration. This case discusses the impact of delayed diagnosis in an 84-year-old woman with previous laparoscopic hernia repair.
CASE REPORT
A frail 84-year-old European woman (39.5 kg, body mass index < 18.5 kg/m2) presented with right groin pain for 2 days associated with constipation and reduced mobility. Her medical history included chronic obstructive pulmonary disease (COPD) on home oxygen, atrial fibrillation and congestive cardiac failure. Her medications included warfarin, inhalers, diuretics and antihypertensives. Previous surgical operations included open appendectomy and laparoscopic right totally extraperitoneal (TEP) inguinal hernia repair several years prior.
On presentation her vital signs were within normal limits including heart rate 67 beats per minute, blood pressure 145/67 mmHg, respiratory rate 22, temperature 36.2°C and SpO2 100% on nasal prongs (2 L/min). Her abdomen was soft with no palpable masses and normal bowel sounds. The right groin pain was exacerbated by extension and abduction of the right hip and tenderness over the medial adductors. Initial biochemical investigations, including full blood count, electrolytes, renal function, liver function and coagulation panel were normal. A pelvic X-ray did not show any features of fracture or bowel obstruction (Fig. 1). The initial differential diagnoses included adductor strain and occult fracture of the right hip. She was admitted under geriatrics for treatment of constipation and mobility assessment during which time her bowels opened.

Pelvic X-ray on initial admission demonstrated no features of fracture, bowel obstruction or incarcerated hernia.
On Day 4, she developed sudden onset of abdominal distension with nausea and vomiting and an urgent surgical review followed. CT abdomen with intravenous and oral contrast demonstrated small bowel obstruction secondary to strangulated obturator hernia (Fig. 2). Repeat blood investigations revealed an elevated C-Reactive Protein (CRP) (143 mg/L) with mildly elevated lactate (1.1 mmol/L) and urea (8.9 mmol/L). Fluid resuscitation and urgent exploratory laparotomy were performed showing extensive adhesions at the proximal bowel with dilatation of small bowel and ischaemia of the herniated section. The bowel was necrotic and a 10 cm resection followed by a hand-sewn side-to-side anastomosis with direct closure of the hernia defect primarily.
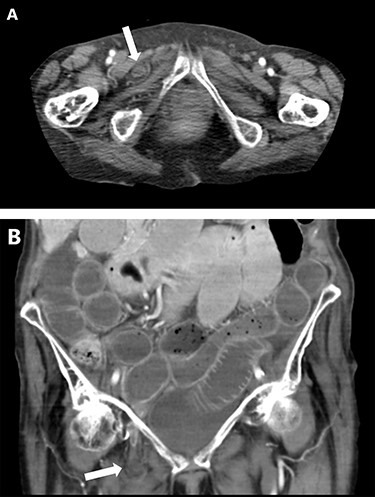
CT abdomen showing small bowel obstruction with right-sided obturator hernia (white arrow) on axial (A) and coronal (B) views.
Postoperatively, she was admitted to intensive care for ventilatory support with worsening hypotension. Within an hour, she deteriorated further due to type II respiratory failure and unfortunately suffered cardiac arrest.
DISCUSSION
Obturator hernia is a diagnostic challenge to surgeons due to its vague symptoms and signs. Associated risk factors include advanced age, multiparity, low body mass index and raised intra-abdominal pressure due to conditions such as COPD and chronic constipation [2]. They are typically right-sided due to the sigmoid colon on the left, less likely to strangulate and females are predisposed due to a broader pelvis and obturator canal [3]. The obturator hernia occurs in three stages: a preperitoneal fat plug enters the canal, followed by dimpling of the peritoneum, and intra-abdominal contents enter this sac, commonly containing small bowel, forming a hernia [4].
Common presentations include abdominal pain, nausea and vomiting consistent with a small bowel obstruction in over 80% of cases [5]. The pathognomonic Howship-Romberg sign, pain on hip extension, abduction and internal rotation, is present in 15–50% of cases [6]. The Hannington-Kiff sign, absent adductor reflex and an intact patellar reflex, is reported as more specific [7]. In our case, a positive Howship-Romberg sign was unrecognised at initial presentation but attributed to musculoskeletal pain. These tests are sometimes hard to perform in frail, elderly patients, and other hip-related pathologies may cloud the diagnosis such as osteoarthritis, pelvic or femoral fracture; less commonly diverticulitis and appendicitis. CT is the most useful imaging modality with the greatest sensitivity and specificity, associated with lower rates of bowel resection and reduced risk of morbidity and mortality [8]. A high index of suspicion supplemented with serial examination and CT imaging can aid the clinician in confirmation of the diagnosis.
In our case, two factors that questioned the likelihood of an obturator hernia included the sudden change in symptoms on Day 4 and a previous TEP repair. Prior to Day 4, clinical suspicion for bowel obstruction remained low as the patient had previously opened her bowels. Yip’s series on obturator hernia reports that spontaneously resolving small bowel obstruction is seen in a third of obturator hernia patients [9].
An obturator case series identified that non-survivors had a significantly longer delay from onset of presenting symptoms to diagnosis and an elevated urea level with a total mortality rate of 27.8% [10]. In this event, fluid resuscitation, anaesthetic input and expediting surgery are imperative to optimising clinical outcomes. Diagnosis delayed by >24 hours increases the risk of death by 3.5 times [11]. A recent systematic review has associated delayed diagnosis and increased length of stay with increased risk of bowel ischaemia and more extensive bowel resection [12].
Surgical intervention is the mainstay of treatment including open midline laparotomy, laparoscopic transabdominal preperitoneal (TAPP) repair and TEP repair [13]. Laparoscopic repair is preferred due to improved visualisation and postoperative outcomes including decreased length of stay, postoperative pain and postoperative mortality [12]. The principles of laparoscopic TEP repair expose the extraperitoneal space of the lower abdomen displaying the deep inguinal ring, cord structures, femoral canal and deeper dissection would expose the obturator canal [14]. The mesh is then positioned from the pubic symphysis covering Cooper’s ligament, Hesselbach’s triangle, deep inguinal ring, femoral and obturator space and with the tail extending laterally towards the space of Bogros [14]. An underlying assumption from initial presentation was that the TEP approach satisfactorily covered all spaces, but the possible causes for recurrence or a missed hernia were most likely technique and mesh related. When managing hernia defects, they may be closed using simple sutures or tissue flaps composed of peritoneum or other adjacent viscera; in the obturator membrane this is largely surrounded by bony structures [15]. We advocate for mesh use as mesh has been associated with reduced morbidity rates, lower risk of recurrence and shortened length of stay [12, 15]. The learning curve for laparoscopic hernia management can be challenging for trainees and experienced surgeons. We advocate the surgical approach (open, TAPP, TEP) should be tailored to the clinical status of the patient and surgeon expertise at the local hospital. To the best of our knowledge, this is the first reported case of an obturator hernia with TEP repair, which hoodwinked clinicians and surgeons until CT imaging proved otherwise.
CONCLUSION
In emaciated, elderly female patients presenting with non-specific pain, early CT imaging assists clinicians’ judgement when signs or symptoms are unclear. Clinical vigilance and serial examination are important in elderly patients often under the care of geriatricians, allowing early discovery and treatment of this type of hernia.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
We have no funding to declare. Patient consent has been obtained.



