-
PDF
- Split View
-
Views
-
Cite
Cite
Paola Caprino, Franco Sacchetti, Luca Tagliaferri, Maria Antonietta Gambacorta, Angelo Eugenio Potenza, Dario Pastena, Luigi Sofo, Use of electrochemotherapy in a combined surgical treatment of local recurrence of rectal cancer, Journal of Surgical Case Reports, Volume 2021, Issue 9, September 2021, rjab403, https://doi.org/10.1093/jscr/rjab403
Close - Share Icon Share
Abstract
Recurrence of rectal cancer (RRC) affects up to one-third of patients. The survival is strictly dependent on the possibility of performing surgery without microscopic tumor residues (R0).
Electrochemotherapy (ECT) is based on the effect that electric pulsations have on increasing the permeability of the cell membrane to certain drugs. We propose the association of ECT to the surgical excision of perineal RRC in a 72-year-old male patient. Given the proximity between the recurrence and the urethra, it was decided to use ECT in order to clean any further neoplastic residues 10 mm from the surgical resection margin. Pelvic MRI at 4 and 7 months and clinical follow-up conducted for 9 months did not document disease recurrence. ECT combined with surgery can prove to be a valid choice in selected cases and could be the best treatment the patient is willing to accept.
INTRODUCTION
The recurrence of rectal cancer (RRC) after radical surgery develops in a percentage that ranges from 2.6 to 32% of the cases, and the 5-year survival of these patients is less than 5% in absence of an appropriate surgical treatment. A radical surgical treatment of the recurrence (R0) is closely related to increased chances of survival (up to 60% at 5 years) [1].
The choice of the surgical treatment is strongly influenced by the strategy to carry out a radical resection, and the site of the recurrence is one of the determining conditions for the surgical possibilities. The adjuvant integrated and intraoperative radiotherapy (+/− chemotherapy) treatment revealed to be useful for a survival prolongation if associated to salvage surgery.
CASE REPORT
The combined surgical and electrochemotherapy technique proposed was adopted to treat a 72-year-old male patient with an RRC developed in a long-standing ulcerative colitis of the rectum. In 1991, the patient underwent surgery for intra-abdominal total colectomy with terminal ileostomy for acute severe UC. In 2018, he noticed the appearance of right ischial-rectal abscess associated with a perianal fistula with evidence of rectal adenomatous villous lesion with high-grade dysplasia. So, the patient went to surgery with proctectomy in November 2018 for adenocarcinoma G2 infiltrating the muscle tunic (pT2 pN0 M0 sec. ajcc 2017). The surgical resection margins were free from neoplastic localization.
After a multidisciplinary consult, an adjuvant chemotherapy and pelvic radiotherapy treatment was proposed to the patient, but he refused and avoided to undergo oncological follow-up until October 2019 when he noticed the appearance of a hard-wooden swelling in the soft tissue of right perineal region (6–7 cm in diameter). After a CT scan (Fig. 1) and MRI that confirmed a local recurrence of cancer, following a multidisciplinary discussion between surgeons, radiation oncologists, radiologists and oncologists, a surgical resection indication was given.
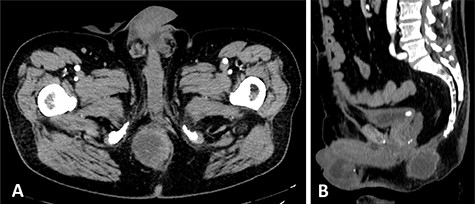
Preoperative CT that documents the absence of a clear cleavage plane between the neoplasm and the urethra in axial (A) and sagittal (B) scans.
However, the CT investigation documented a close relationship between the neoplastic lesion and the root of penis and urethra, with consequent difficulty in obtaining the certainty of disease-free margins without a major demolition procedure that the patient firmly refused.
To increase the chance of best treatment of the margin and perform a local remediation of the tissue adjacent to the neoplasm, it was decided to associate resective surgical treatment to ECT.
Intraoperative time I: the mass infiltrated the perineal muscles and appeared anteriorly tightly close to the prostate plane and root of penis. Removal of the neoformation was made en-bloc with a portion of skin and perineal muscles.
Intraoperative time II: after intravenous infusion of Bleomycin (28 500 IU), intraoperative electrochemotherapy on the muscular and prostate planes was performed (n. 30 electrical discharges). The electrodes were set with a depth of 1.5 cm in order to treat the tumor bed with attention to the anterior wall where the margins were surely closer (Fig. 2).
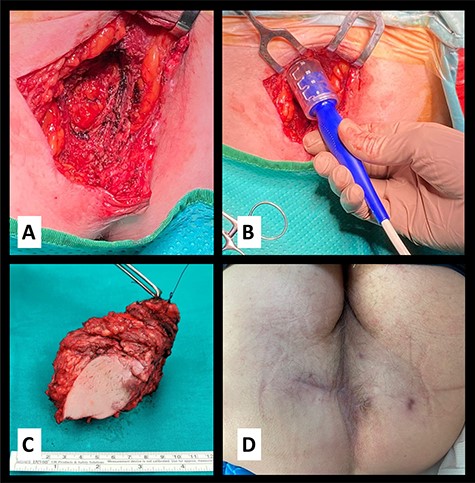
(A) Operative detail with partial removal of the pelvic floor muscle infiltrated by the neoplasm; (B) application of electrical stimulation by penetrating the electrodes for 1.5 cm; (C) surgical specimen, reference thread on the deep margin near the base of the penis and (D) surgical site eight months after surgery.
An aspiration drain was placed in the residual surgical cavity, and the skin was sutured without the need of cutaneous flap.
Histological examination documented moderately differentiated mucinous adenocarcinoma with component mucosecernent representing about 95% of the neoplasm and intense positivity for CDX2, CK19, CK20, CK7, MUC2, MUC1 and MUC5AC, in agreement with intestinal primitiveness.
The resection margins were microscopically free of disease (variable distance between 0.1 and 0.4 cm from the neoplasm).
The postoperative course was regular and without complications.
Pelvic MRI with contrast was performed during the follow-up at 4 and 7 months after surgery without documenting neoplastic recurrence.
Clinical follow-up was conducted for 9 months, and during this period, the patient presented no clinical signs of neoplastic recurrence or other noteworthy perineal, genitourinary or sexual problems.
DISCUSSION
ECT is a relatively recent technique based on the effect that electric pulsations have on increasing the permeability of the cell membrane to certain drugs.
The first applications dates back to 1982 from Neumann et al., and it consists in being able to convey, through electrical impulses, drugs that are poorly permeant inside the target cell, increasing the effect of chemotherapy [2].
The drug most used in this technique is Bleomycin, with a powerful cytotoxic activity, which, however, in consideration of its charge, hardly penetrates through the cell wall. With the aid of electric current to enter the cell, Bleomycin enhances its cytotoxic activity about 300-fold [3].
Although there are no absolute contraindications to the administration of bleomycin, attention must be paid to old age, smoking habit, renal function and previous pulmonary diseases [4].
To date, the main use of this technique concerns the treatment of neoplastic lesions (primary or secondary) of the skin and subcutaneous tissues, or rather these sites easily reachable by the needle-like electrodes through which the electrical impulse is administered to the pathological tissue.
The most recent uses also concern ECT applications through endoscopy for the treatment of colorectal tumors in patients who were deemed ineligible for or had declined standard treatments [5].
Our proposed use of a combined technique has had the curative intent to widen the radial margin on a surgical site without sacrificing bordering organs; this approach allows to clear the nearby tissue from eventual microscopic spots of neoplastic disease radially gaining till 10 mm from the resection margin avoiding direct damages to the ‘non-resectable’ structures.
The procedure has revealed to be easy, safe and fast without postoperative complication.
One of the major, well-known, postoperative complication after surgery for distal rectal tumors subjected to radiotherapy is the surgical site infections and the consequent difficult and delayed wound closure [5].
The ECT allows to perform surgery on a perianal district not subjected to neoadjuvant radiotherapy, with a lower risk of local infectious complications that often significantly impair the quality of life of the patients. This clinical case also confirms the importance of discussing cases in multidisciplinary meetings [6, 7].
However, considering the absence of robust scientific evidence, this new approach needs a clinical validation with prospective clinical trials [8].
CONCLUSIONS
We suggest that the use of ECT combined with surgery, in selected cases and in the absence of distant metastases, is a safe technique that can be used with curative intent.
Larger future studies will allow to evaluate the effects in terms of possible improvement of prognosis and survival.
AUTHORS' CONTRIBUTIONS
Each author contributed to the creation, drafting and approval of the final manuscript.
CONFLICT OF INTEREST STATEMENT
The authors declare that there is no conflict of interest.
FUNDING
The authors received no financial support for the research, authorship and/or publication of this article.



