-
PDF
- Split View
-
Views
-
Cite
Cite
Yukihiro Tatekawa, A case of ultrashort-segment Hirschsprung’s disease discovered after taking polyethylene glycol electrolyte solution for chronic constipation, Journal of Surgical Case Reports, Volume 2021, Issue 9, September 2021, rjab390, https://doi.org/10.1093/jscr/rjab390
Close - Share Icon Share
Abstract
We report a case of ultrashort-segment Hirschsprung’s disease (HD) involving a 4-year-old girl. She was born at 29 weeks gestation from a twin pregnancy. She weighed 1013 g. After birth, she received glycerin enemas and sodium picosulfate hydrate to facilitate defecation. She passed stool once every 4–5 days. When she was 4 years old, she was medicated with polyethylene glycol electrolyte solution. After she drank the solution twice, the abdomen distended rapidly without passage of stool. An abdominal X-ray showed a stored stool mass and a barium enema study revealed dilatation from the rectum to the sigmoid colon due to the stool mass. She underwent anorectal manometry and a rectal biopsy, and was suspected to have HD. She underwent a Soave endorectal pull-through with an oblique anastomosis. She passed stool 4–10 times a day for 6 months postoperatively, but the frequency of passing stool gradually deceased without medications.
INTRODUCTION
Hirschsprung’s disease (HD) is classified based on aganglionic lesions as follows: short segment, rectosigmoid segment, long segment and entire colon aganglionosis. A barium enema study is useful to demonstrate the zone of transition between the aganglionic distal segment and the ganglionic proximal segment. In short segment aganglionosis, the transition zone is often obscure, and it is difficult to diagnose short segment HD [1]. In contrast, a rectal biopsy is a more reliable examination to demonstrate aganglionic lesions, but the distance from the aganglionic bowel wall to the dentate line is normal [2–4]. It has been reported that the distance from the aganglionic bowel from the dentate line in Meissner’s plexus is longer than the corresponding distance in Auerbach’s plexus. Therefore, it is difficult to determine the site for a biopsy and the site of the mucosal suction biopsy should be higher than the full-thickness biopsy.
CASE REPORT
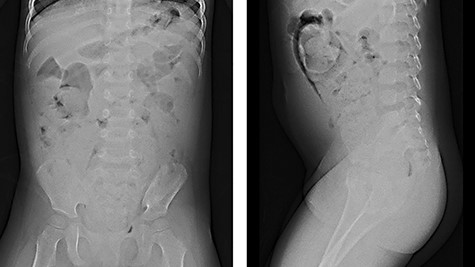
We report herein a case of a 4-year-old girl with ultrashort-segment HD (USHD). She was born at 29 weeks gestation from a twin pregnancy. Her birth weight was 1013 g. After birth, she was administered glycerin enemas to facilitate defecation. Thereafter, she was medicated with sodium picosulfate hydrate for chronic constipation, but she passed stool once in 4–5 days. When she was 4 years old, she was medicated with polyethylene glycol electrolyte solution (MOVICOL® [macrogol 4000]; EA Pharma Co., Ltd, Tokyo, Japan) in another hospital for chronic constipation. After she drank the MOVICOL® twice, her abdomen distended rapidly without passing stool, and she was transported to a hospital. An abdominal X-ray showed a stored stool mass (Fig. 1). A barium enema study revealed dilatation from the rectum to the sigmoid colon due to the stool mass and the rectum was smooth with funnel-shaped tapering toward the anus when she forced herself to defecate (Fig. 2). USHD was suspected, so she underwent anorectal manometry, which showed negative normal reflux. A surgical rectal full-thickness biopsy was performed 2 cm proximal to the dentate line under general anesthesia, which revealed very few ganglion cells in Auerbach’s plexus (Fig. 3a–c). She was suspected to have HD and underwent a Soave endorectal pull-through with an oblique anastomosis, where the pulled-through bowel was anastomosed posteriorly 0.5 cm from the dentate line, laterally 1.0 cm from the dentate line and anteriorly 1.5 cm above this point (Fig. 4). The posterior wall of the aganglionic anorectum was split longitudinally to the level of the dentate line. The resected specimen showed sparse ganglion cells with small cytoplasm in Auerbach’s plexus of the mucosectomy in the rectum (Fig. 5 ①, a and b). In the sigmoid colon of the resected specimen, most of the ganglion cells had scanty cytoplasm, whereas occasional ganglion cells with abundant cytoplasm were visualized (Fig. 5 ②, c and d). She passed stool 4–10 times a day for 6 months postoperatively, but the frequency of passing stool gradually deceased to once or twice a day without anastomotic strictures. Defecation was controlled without medications for 12 months postoperatively.
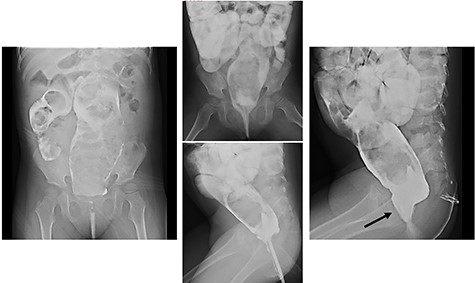
Barium enema: barium enema revealed dilatation from the rectum to the sigmoid colon due to a stool mass and the rectum showed a smooth funnel-shaped tapering toward the anus when she forced herself to defecate (black arrow: funnel-shaped tapering).
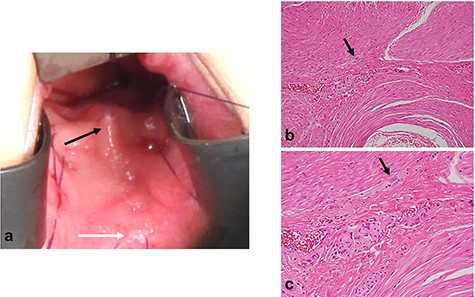
Surgical rectal full-thickness biopsy. (a) Surgical rectal full-thickness biopsy was performed 2 cm proximal to the dentate line under general anesthesia. (b, c) Pathologic findings revealed few ganglion cells in Auerbach’s plexus (b: low-power field, c: high-power field, black arrow; ganglionic cells).
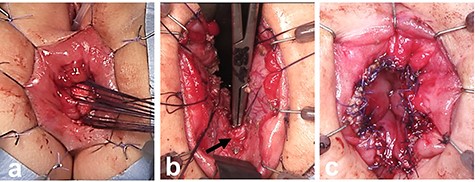
Soave endorectal pull-through with an oblique anastomosis. (a) The site of mucosectomy in the rectum was located posteriorly 0.5 cm from the dentate line, laterally 1.0 cm from the dentate line, and anteriorly 1.5 cm above this point. (b) The posterior wall of the aganglionic anorectum was split longitudinally to the level of the dentate line. (c) The oblique anastomosis between the pulled-through bowel and the rectum was performed posteriorly 0.5 cm from the dentate line, laterally 1.0 cm from the dentate line and anteriorly 1.5 cm above this point.
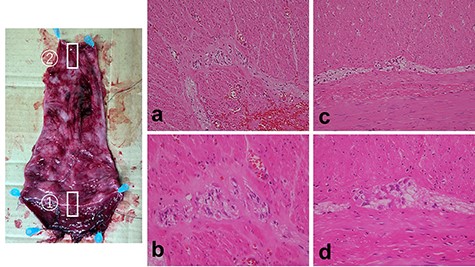
Resected specimen and pathologic findings. Resected specimen (①: anal side; ②: anal side). (a, b) In Auerbach’s plexus of the mucosectomy in the rectum, few ganglion cells with scanty cytoplasm were visualized (a: low-power field, b: high-power field). (c, d) In Auerbach’s plexus of the sigmoid colon, most of the ganglion cells had scanty cytoplasm, whereas few ganglion cells with large cytoplasm were visualized.
DISCUSSION
To diagnose HD, a barium enema study can reveal the transition zone between the aganglionic distal segment, which is narrow or of normal caliber, and the dilated proximal colon with normal ganglion cells. The transition zone to the dilated segment is often characterized as funnel-shaped or an inverted cone. Although the transition zone can be a very reliable sign, non-visualization of this sign does not rule out HD [1]. In classifying HD, USHD is only involved at the distal part of the rectum.
The normal aganglionic zone in the distal rectum has been described based on a histologic evaluation of a cadaveric strip myectomy with overlying mucosa. The mean distance of aganglionic bowel from the dentate line was 6.6 mm (range, 0–21 mm) in Meissner’s plexus and 5.1 mm (range, 0–15 mm) in Auerbach’s plexus. The normal distance of the aganglionic bowel wall from the dentate line is ≤2 cm [2]. Based on such a basic study, the absence of ganglion cells in a full-thickness rectal biopsy obtained 2 cm proximal to the dentate line confirmed a diagnosis of USHD [3, 4].
For chronic constipation, Bentley first performed a posterior anorectal myectomy. Scobie and Mackinlay managed 26 cases with chronic constipation who underwent anorectal myectomies; 4 required repeat myectomies and 3 underwent anterior resections [5]. Complete excision of the megarectum and any adjacent dilated colon, such as a Soave transanal pull-through procedure with a posterior myectomy, is considered to be a reasonable alternative [3]. The postoperative complications of a Soave endorectal pull-through (mainly anastomotic strictures) are problematic. Recently, a new technique involving an oblique anastomosis between the pulled-through colon and the anus has been described [6, 7]. There are multiple causes of anastomosis strictures, one of which is circular anastomosis. In a report involving an oblique anastomosis in a Soave endoanal pull-through, the oblique anastomosis is associated with a lower stricture rate [6, 7]. In the current case, the girl passed stool 4–10 times a day 6 months postoperatively, but gradually the frequent of passing stool deceased to once or twice a day without anastomotic strictures and defecation was controlled without medications 12 months postoperatively.
Constipation treatment with MOVICOL® was included in the Japan National Health Insurance drug price list as of November 2018. MOVICOL® is the first polyethylene glycol preparation indicated for the treatment of chronic constipation in Japan and is available for adults and children ≥2 years of age. MOVICOL® increases the moisture in the intestinal tract as a result of the osmolality of the main ingredient, polyethylene glycol (macrogol 4000), which activates the peristaltic movement of the colon physiologically to promote a bowel movement. In patients with underlying diseases and chronic constipation, abdominal distension may worsen the risk of intestinal perforation, which may easily occur when using MOVICOL®. It is necessary to rule out stenosis or obstruction in the intestinal tract as causes of constipation, especially in patients with USHD.
CONFLICT OF INTEREST STATEMENT
None declared.
References
- pregnancy
- anorectal manometry
- chronic constipation
- defecation
- hirschsprung's disease
- anastomosis, surgical
- dilatation, pathologic
- feces
- glycerol
- abdominal radiography
- sigmoid colon
- enema administration
- rectum
- polyethylene glycol-electrolyte solution
- barium enema
- abdominal swelling
- endorectal resection
- twin pregnancy
- rectal biopsy
- sodium picosulfate



