-
PDF
- Split View
-
Views
-
Cite
Cite
Tyler Davis, Paige Moudy, Mohamed Abdelgawad, Lutfi Barghuthi, Hishaam Ismael, Gallbladder adenosquamous carcinoma: a case report and literature review, Journal of Surgical Case Reports, Volume 2021, Issue 9, September 2021, rjab365, https://doi.org/10.1093/jscr/rjab365
Close - Share Icon Share
Abstract
Representing 90–95% of all malignant gallbladder neoplasms, adenocarcinoma is by far the most common subtype. Adenosquamous carcinoma is a rare subtype, accounting for only 1–5% of all gallbladder carcinomas. These tumors have been shown to have aggressive biologic behavior, commonly extending to adjacent structures. Some studies have shown that the squamous component often displayed a greater proliferative capacity than the adenocarcinomatous component (possibly even up to twice as fast). Complete surgical resection is currently the mainstay of treatment but the prognosis is often poor. In this paper, we present a case of a 69-year-old male with an AJCC Stage IV moderately differentiated adenosquamous carcinoma of the gallbladder treated with radical cholecystectomy including liver segments IVb, V, VI.
INTRODUCTION
Although rare, gallbladder carcinoma is the most common type of biliary tract cancer. It has a clear predominance for females, but its geographical prevalence is widely variable, suggesting a complex association with genetic and environmental factors. Risk factors include cholelithiasis, obesity, gallbladder polyps and female sex. Many histologic subtypes exist. Representing 90–95% of all malignant gallbladder neoplasms, adenocarcinoma is by far the most common subtype. Adenosquamous carcinoma is a rare subtype, accounting for only 1–5% of all gallbladder carcinomas. Strong controversy exists over its histogenesis. Some believe that it is squamous differentiation in an adenocarcinoma, while others think it may be closely related to the neoplastic process of squamous cell carcinoma. Regardless of how they arise, these tumors have been shown to have aggressive biologic behavior, commonly extending to adjacent structures including the liver, omentum, stomach, duodenum and transverse colon. Some studies have shown that the squamous component often displayed a greater proliferative capacity than the adenocarcinomatous component. Complete surgical resection is currently the mainstay of treatment, but the prognosis is often poor.
In this paper, we present a case of a 69-year-old male with an AJCC Stage IV moderately differentiated adenosquamous carcinoma of the gallbladder treated with radical cholecystectomy including liver segments IVb, V, VI.
CASE PRESENTATION
This paper presents a 69-year-old male initially presenting to the clinic for a new liver lesion identified on screening CT scan. Review of systems was significant for fatigue, weight loss, easy bruising/bleeding, chronic back and joint pain. The patient’s past medical history is significant for tobacco use, cholelithiasis, left renal cell carcinoma status-post left robotic-assisted partial nephrectomy, bilateral Warthrin’s Tumor status-post bilateral superficial parotidectomy, benign prostatic hyperplasia, hypertension and coronary artery disease.
CT guided biopsy of the lesion demonstrated the presence of invasive squamous cell carcinoma with p40-positive and focally positive for CK7 cells. Caris testing was positive for PDL1 (95%) with stable MMR and low TMB. PET scan revealed a large hypermetabolic, centrally necrotic mass involving liver segments V, VI without any abnormal FDG uptake within the head, neck or chest. Pertinent images from the PET scan are demonstrated in Figs 1 and 2.
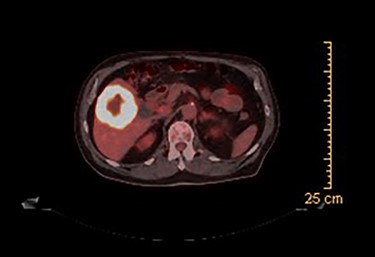
PET scan (axial view): hypermetabolic, centrally necrotic mass involving liver segment V, VI.

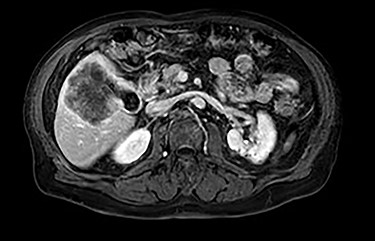
MRI demonstrated a 7.1 × 8.1 cm mass originating from the gallbladder that involved segments IVb, V, VI with areas of peripheral enhancement and central necrosis. Associated cholelithiasis was also noted. Figures 3–5 demonstrate the pertinent MRI findings.
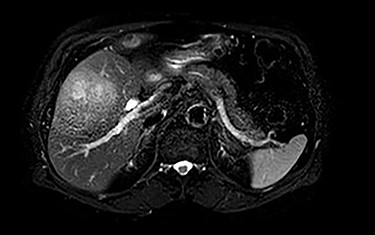
MRI (axial view): 7.1 × 8.1 cm mass originating from the gallbladder involving segments IVb, V, VI with areas of peripheral enhancement and central necrosis.

This patient was treated with a radical cholecystectomy including liver segments IVb, V, VI and portal lymphadenectomy. Using a modified Makuuchi incision, the liver, colon and duodenum were mobilized. There was no identifiable tumor involvement of the bowel. The cystic duct was isolated and divided at the bile duct. A frozen section of the cystic duct was sent for analysis which revealed negative margins. Portal lymphadenectomy and resection of liver segments IVb, V, VI en-bloc with the gallbladder was performed and sent for histopathologic analysis. Falciform and omental pedicle flaps were created and two drains were placed. The patient tolerated the procedure well with no acute intraoperative complications. His post-operative course was unremarkable and he was discharged on post-operative Day 4.
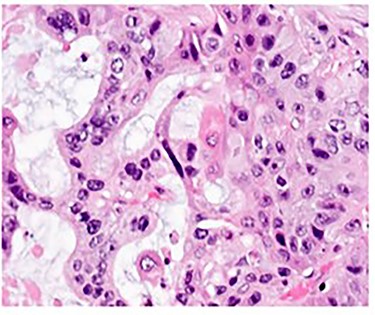
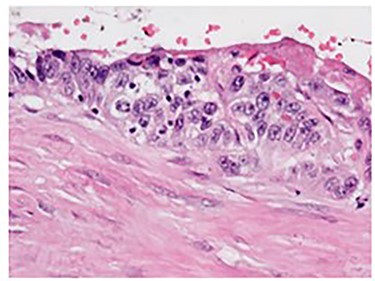
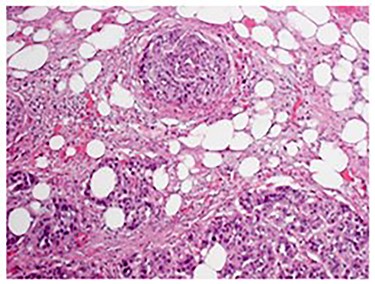
Pathologic analysis revealed an AJCC Stage IV (pT3, N0, M1) 7.7 cm moderately differentiated (histologic grade G2) adenosquamous carcinoma of the gallbladder with lymphovascular and perineural invasion, and tumor extension into adjacent liver, peritoneal surface and residual lesser omentum. Surgical margins were all negative. No tumor was identified in any of the eight portal lymph nodes obtained. Figure 6 shows a gross cross section of the gallbladder. Figure 7 shows H&E stain of the tumor demonstrating adenosquamous features. Figure 8 shows an H&E stain demonstrating peritoneal surface involvement. Figure 9 shows an H&E stain demonstrating involvement of the lesser omentum.
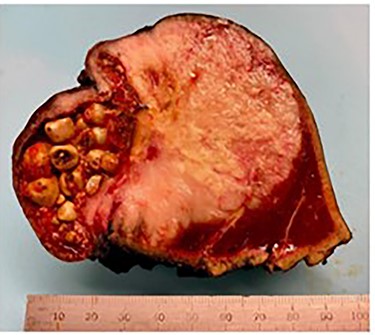
Gross cross section of the gallbladder demonstrating tumor involvement and cholelithiasis.
DISCUSSION
Gallbladder adenosquamous carcinomas are a rare occurrence. Literature review of 69 cases (summarized in Table 1) demonstrated that the average patient age to be 66.6 years old ranging from 43 to 89 years old [1–12]. There was a clear gender predominance with 72.5% (50/69) patients being female, yielding a Female: Male Ratio of 2.6:1. This statistic is similar to those previously reported in the literature. Cholelithiasis was reported in over half of these patients, again suggesting its association as a risk factor for developing gallbladder carcinoma.
| Article title . | Author(s) . | Age . | Gender . | Presentation . | Tumor Size . | Radical resection performed? . | Primary tumor resection performed? . | T . | N . | M . | Stage . | Involvement of adjacent structures . | Outcome (months, status) . |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Adenosquamous carcinoma of the gallbladder warrants resection only if curative resection is feasible | Oohashi Y, Shirai Y, Wakai T, Nagakura S, Watanabe H, Hatakeyama K. | 47 | M | Cholelithiasis in 15 patients | Mean: 7 cm Range: 2.5–14 cm | X | 4 | 2a | 0 | IVb | Liver | 154, Alive | |
| 65 | F | X | 4 | 1a | 0 | IVa | Liver, omentum | 151, Alive | |||||
| 52 | F | X | 3 | 0a | 0 | III | Liver | Alive | |||||
| 60 | F | X | 1a | 0a | 0 | I | None | 121, Alive | |||||
| 69 | F | X | 4 | 1a | 0 | IVa | Liver, colon, duodenum | 62, Alive | |||||
| 62 | M | X | 4 | 2a | 0 | IVb | Liver, colon, duodenum, pancreas | 48, Alive | |||||
| 66 | F | X | 2 | 0a | 0 | III | None | 156, Died of other causes | |||||
| 84 | F | X | 3 | 2a | 1 | IVb | Bile duct | 23, Died of Disease | |||||
| 70 | F | X | 3 | 2a | 1 | IVb | Omentum | 13, Died of Disease | |||||
| 64 | F | X | 4 | 2a | 1 | IVb | Liver, duodenum, stomach | 6, Died of other causes | |||||
| 77 | F | X | 4 | 2a | 0 | IVb | Liver | 5, Died of other causes | |||||
| 62 | F | X | 4 | 2a | 0 | IVb | Liver | 5, Died of Disease | |||||
| 70 | M | X | 3 | 0a | 0 | III | Liver | 4, Died of Disease | |||||
| 83 | F | X | 4 | 0a | 0 | IVa | Liver, colon | 4, Died of Disease | |||||
| 70 | F | X | 4 | 0a | 0 | IVa | Liver, omentum | 3, Died of Disease | |||||
| 78 | M | X | 2 | 0b | 0 | II | None | 45, Died of other causes | |||||
| 60 | F | X | 2 | 2b | 0 | IVb | None | 19, Died of Disease | |||||
| 74 | F | X | 3 | 2c | 1 | IVb | Liver | 8, Died of other causes | |||||
| 72 | F | X | 2 | 2b | 0 | IVb | None | 7, Died of other causes | |||||
| 43 | F | X | 4 | 1b | 0 | IVa | Liver, colon | 5, Died of other causes | |||||
| 62 | M | X | 4 | 2b | 1 | IVb | Liver, colon | 5, Died of other causes | |||||
| 46 | F | X | 3 | 2b | 1 | IVb | Liver | 4, Died of other causes | |||||
| 67 | F | X | 3 | 2c | 0 | IVb | Liver | 3, Died of other causes | |||||
| 78 | F | X | 2 | 2c | 0 | IVb | None | 3, Died of Disease | |||||
| 75 | F | X | 3 | 0c | 0 | III | None | 3, Died of Disease | |||||
| 56 | M | X | 4 | 2c | 0 | IVb | Liver, colon | 3, Died of Disease | |||||
| 74 | F | X | 3 | 0c | 1 | IVb | None | 2, Died of Disease | |||||
| 89 | F | X | 3 | 0c | 1 | IVb | Liver | 1, Died of Disease | |||||
| Adenosquamous/squamous cell carcinoma of the gallbladder | Chan KM, Yu MC, Lee WC, Jan YY, Chen MF | 66 | F | Cholelithiasis, abdominal pain, fever, jaundice, weight loss | X | 3 | 1 | 1 | IVb | Liver | 3.2, Died of Disease | ||
| 62 | F | X | 3 | 1 | 0 | III | Liver | 18.4, Died of Disease | |||||
| 72 | F | X | 4 | 1 | 0 | IVa | Liver, duodenum, colon, bile duct | 4.7, Died of Disease | |||||
| 54 | F | X | 4 | 1 | 0 | IVa | Liver, bile duct | 9.3, Alive | |||||
| 72 | F | X | 4 | 1 | 0 | IVa | None | 87.3, Died of Disease | |||||
| 49 | M | X | 3 | 1 | 0 | III | None | 3.7, Died of Disease | |||||
| 68 | F | X | 3 | 1 | 0 | III | Liver | 4.2, Died of Disease | |||||
| 89 | F | 4 | 1 | 0 | IVa | Liver, duodenum | 0.8, Died of surgical mortality | ||||||
| 55 | M | X | 4 | 1 | 0 | IVa | Liver, stomach | 6.4, Died of Disease | |||||
| 67 | F | X | 4 | 1 | 0 | IVa | Liver, bile duct | 1.5, Died of surgical mortality | |||||
| 75 | M | X | 3 | 0 | 0 | III | None | 14.0, Died of Disease | |||||
| 66 | F | X | 3 | 1 | 1 | IVb | Liver | 1.5, Died of Disease | |||||
| Surgical resection of splenic metastasis from the adenosquamous gallbladder carcinoma: A case report | Utsumi M, Aoki H, Kunitomo T, Mushiake Y, Kanaya N, Yasuhara I, Arata T, Katsuda K, Tanakaya K, Takeuchi H | 62 | F | Abdominal pain | 8.0 cm | X | 4 | 1 | 1 | IV | Liver, colon, spleen, diaphragm | Alive | |
| A primary adenosquamous gallbladder carcinoma with sarcomatoid features | Qian X, Wu Y, Gao B, Wang W | 51 | F | Abdominal pain, anemia, abnormal LFTs | 4.5 x 7.0 cm | X | 5, Died of Disease | ||||||
| Long-term survival of a patient with advanced adenosquamous carcinoma of the gallbladder after radical resection | Fujita T, Fukuda K, Ohmura Y, Nishi H, Mano M, Komatsubara S, Doihara H, Shimizu N | 72 | F | Fatigue, weight loss, anorexia | 4.5 cm | X | 4 | 0 | 0 | IVa | Stomach | 60, Alive | |
| Hepatopancreatoduodenectomy for squamous and adenosquamous carcinoma of the gallbladder | Miyazaki K, Tsutsumi N, Kitahara K, Mori M, Sasatomi E, Tokunaga O, Hisatsugu T | 70 | M | X | 4 | 1b | 0 | IV | Liver, duodenum | 6, Died of Disease | |||
| Adenosquamous carcinoma of the gallbladder: a clinicopathological, immunohistochemical and flow-cytometric study of 20 cases | Nishihara K, Nagai E, Izumi Y, Yamaguchi K, Tsuneyoshi M | 68 | F | Cholelithiasis | Mean: 6.3 cm Range: 3.8–10.6 cm | Radical resection performed in 10 out of 20 patients | Primary tumor resection performed in 10 out of 20 patients | Stage II: 3 Stage III: 11 Stage IV: 6 | Cystic duct, peritoneum | 3, Died of Disease | |||
| 52 | F | Cholelithiasis | None | 12, Died of Disease | |||||||||
| 64 | F | None | 5, Died of Disease | ||||||||||
| 72 | M | Liver | 3, Died of Disease | ||||||||||
| 63 | F | Cholelithiasis | None | 6, Died of Disease | |||||||||
| 73 | F | Duodenum | 1, Died of Disease | ||||||||||
| 63 | F | LN | 11, Died of Disease | ||||||||||
| 78 | F | Cholelithiasis | Duodenum | 7, Died of Disease | |||||||||
| 66 | F | Cholelithiasis | None | 6, Died of Disease | |||||||||
| 78 | F | None | 5, Died of Disease | ||||||||||
| 73 | F | Cholelithiasis | Liver, colon | 12, Died of Disease | |||||||||
| 50 | F | Liver | 6, Died of Disease | ||||||||||
| 64 | M | Liver | 6, Died of Disease | ||||||||||
| 68 | M | Cholelithiasis | None | 56, Alive | |||||||||
| 63 | M | None | 3, Died of Disease | ||||||||||
| 64 | M | Liver, colon | 3, Died of Disease | ||||||||||
| 71 | F | None | 19, Died of Disease | ||||||||||
| 76 | M | None | 3, Alive | ||||||||||
| 72 | M | Cholelithiasis | Omentum | 2, Alive | |||||||||
| 60 | M | Cholelithiasis | None | 5, Died of Disease | |||||||||
| Cholecystic adenosquamous carcinoma mimicking Mirizzi syndrome | Horio T, Ogata S, Sugiura Y, et al. | 73 | F | Cholelithiasis, Obstructive jaundice | X | Hepatoduodenal ligament | 4, Died of Disease | ||||||
| Adenosquamous carcinoma of the gallbladder with tumor thrombus in left portal trunk | Iyomasa, S., Matsuzaki, Y., Hiei, K. et al. | 73 | M | Abdominal pain, palpable epigastric mass | X | Liver, L portal trunk | 120, Alive | ||||||
| Ruptured adenosquamous cell carcinoma of the gallbladder: case report and review of literature | Rustagi T, Rai M, Menon M | 74 | F | Cholelithiasis, abdominal pain, weight loss, anorexia, fever, hepatomegaly | 11 x 10 x 10 cm | X | 3 | 1 | 0 | III | Liver | Alive | |
| A case of primary adenosquamous/squamous cell carcinoma of gallbladder directly invaded duodenum | Saito A, Noguchi Y, Doi C, Mukai K, Fukuzawa K, Yoshikawa T, Amano T, Kondo J, Ito T, Izutsu H | 67 | F | X | Liver, duodenum, pancreas, colon | 4, Died of Disease | |||||||
| Adenosquamous carcinoma of gallbladder presenting as chronic cholecystitis with cholelithiasis- a rare entity | Mohan N, Agrawal R, Kumar P | 45 | F | Cholelithiasis, abdominal pain and distention, fever, SOB, constipation | 9.5 × 5.5 × 3.5 cm | X |
| Article title . | Author(s) . | Age . | Gender . | Presentation . | Tumor Size . | Radical resection performed? . | Primary tumor resection performed? . | T . | N . | M . | Stage . | Involvement of adjacent structures . | Outcome (months, status) . |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Adenosquamous carcinoma of the gallbladder warrants resection only if curative resection is feasible | Oohashi Y, Shirai Y, Wakai T, Nagakura S, Watanabe H, Hatakeyama K. | 47 | M | Cholelithiasis in 15 patients | Mean: 7 cm Range: 2.5–14 cm | X | 4 | 2a | 0 | IVb | Liver | 154, Alive | |
| 65 | F | X | 4 | 1a | 0 | IVa | Liver, omentum | 151, Alive | |||||
| 52 | F | X | 3 | 0a | 0 | III | Liver | Alive | |||||
| 60 | F | X | 1a | 0a | 0 | I | None | 121, Alive | |||||
| 69 | F | X | 4 | 1a | 0 | IVa | Liver, colon, duodenum | 62, Alive | |||||
| 62 | M | X | 4 | 2a | 0 | IVb | Liver, colon, duodenum, pancreas | 48, Alive | |||||
| 66 | F | X | 2 | 0a | 0 | III | None | 156, Died of other causes | |||||
| 84 | F | X | 3 | 2a | 1 | IVb | Bile duct | 23, Died of Disease | |||||
| 70 | F | X | 3 | 2a | 1 | IVb | Omentum | 13, Died of Disease | |||||
| 64 | F | X | 4 | 2a | 1 | IVb | Liver, duodenum, stomach | 6, Died of other causes | |||||
| 77 | F | X | 4 | 2a | 0 | IVb | Liver | 5, Died of other causes | |||||
| 62 | F | X | 4 | 2a | 0 | IVb | Liver | 5, Died of Disease | |||||
| 70 | M | X | 3 | 0a | 0 | III | Liver | 4, Died of Disease | |||||
| 83 | F | X | 4 | 0a | 0 | IVa | Liver, colon | 4, Died of Disease | |||||
| 70 | F | X | 4 | 0a | 0 | IVa | Liver, omentum | 3, Died of Disease | |||||
| 78 | M | X | 2 | 0b | 0 | II | None | 45, Died of other causes | |||||
| 60 | F | X | 2 | 2b | 0 | IVb | None | 19, Died of Disease | |||||
| 74 | F | X | 3 | 2c | 1 | IVb | Liver | 8, Died of other causes | |||||
| 72 | F | X | 2 | 2b | 0 | IVb | None | 7, Died of other causes | |||||
| 43 | F | X | 4 | 1b | 0 | IVa | Liver, colon | 5, Died of other causes | |||||
| 62 | M | X | 4 | 2b | 1 | IVb | Liver, colon | 5, Died of other causes | |||||
| 46 | F | X | 3 | 2b | 1 | IVb | Liver | 4, Died of other causes | |||||
| 67 | F | X | 3 | 2c | 0 | IVb | Liver | 3, Died of other causes | |||||
| 78 | F | X | 2 | 2c | 0 | IVb | None | 3, Died of Disease | |||||
| 75 | F | X | 3 | 0c | 0 | III | None | 3, Died of Disease | |||||
| 56 | M | X | 4 | 2c | 0 | IVb | Liver, colon | 3, Died of Disease | |||||
| 74 | F | X | 3 | 0c | 1 | IVb | None | 2, Died of Disease | |||||
| 89 | F | X | 3 | 0c | 1 | IVb | Liver | 1, Died of Disease | |||||
| Adenosquamous/squamous cell carcinoma of the gallbladder | Chan KM, Yu MC, Lee WC, Jan YY, Chen MF | 66 | F | Cholelithiasis, abdominal pain, fever, jaundice, weight loss | X | 3 | 1 | 1 | IVb | Liver | 3.2, Died of Disease | ||
| 62 | F | X | 3 | 1 | 0 | III | Liver | 18.4, Died of Disease | |||||
| 72 | F | X | 4 | 1 | 0 | IVa | Liver, duodenum, colon, bile duct | 4.7, Died of Disease | |||||
| 54 | F | X | 4 | 1 | 0 | IVa | Liver, bile duct | 9.3, Alive | |||||
| 72 | F | X | 4 | 1 | 0 | IVa | None | 87.3, Died of Disease | |||||
| 49 | M | X | 3 | 1 | 0 | III | None | 3.7, Died of Disease | |||||
| 68 | F | X | 3 | 1 | 0 | III | Liver | 4.2, Died of Disease | |||||
| 89 | F | 4 | 1 | 0 | IVa | Liver, duodenum | 0.8, Died of surgical mortality | ||||||
| 55 | M | X | 4 | 1 | 0 | IVa | Liver, stomach | 6.4, Died of Disease | |||||
| 67 | F | X | 4 | 1 | 0 | IVa | Liver, bile duct | 1.5, Died of surgical mortality | |||||
| 75 | M | X | 3 | 0 | 0 | III | None | 14.0, Died of Disease | |||||
| 66 | F | X | 3 | 1 | 1 | IVb | Liver | 1.5, Died of Disease | |||||
| Surgical resection of splenic metastasis from the adenosquamous gallbladder carcinoma: A case report | Utsumi M, Aoki H, Kunitomo T, Mushiake Y, Kanaya N, Yasuhara I, Arata T, Katsuda K, Tanakaya K, Takeuchi H | 62 | F | Abdominal pain | 8.0 cm | X | 4 | 1 | 1 | IV | Liver, colon, spleen, diaphragm | Alive | |
| A primary adenosquamous gallbladder carcinoma with sarcomatoid features | Qian X, Wu Y, Gao B, Wang W | 51 | F | Abdominal pain, anemia, abnormal LFTs | 4.5 x 7.0 cm | X | 5, Died of Disease | ||||||
| Long-term survival of a patient with advanced adenosquamous carcinoma of the gallbladder after radical resection | Fujita T, Fukuda K, Ohmura Y, Nishi H, Mano M, Komatsubara S, Doihara H, Shimizu N | 72 | F | Fatigue, weight loss, anorexia | 4.5 cm | X | 4 | 0 | 0 | IVa | Stomach | 60, Alive | |
| Hepatopancreatoduodenectomy for squamous and adenosquamous carcinoma of the gallbladder | Miyazaki K, Tsutsumi N, Kitahara K, Mori M, Sasatomi E, Tokunaga O, Hisatsugu T | 70 | M | X | 4 | 1b | 0 | IV | Liver, duodenum | 6, Died of Disease | |||
| Adenosquamous carcinoma of the gallbladder: a clinicopathological, immunohistochemical and flow-cytometric study of 20 cases | Nishihara K, Nagai E, Izumi Y, Yamaguchi K, Tsuneyoshi M | 68 | F | Cholelithiasis | Mean: 6.3 cm Range: 3.8–10.6 cm | Radical resection performed in 10 out of 20 patients | Primary tumor resection performed in 10 out of 20 patients | Stage II: 3 Stage III: 11 Stage IV: 6 | Cystic duct, peritoneum | 3, Died of Disease | |||
| 52 | F | Cholelithiasis | None | 12, Died of Disease | |||||||||
| 64 | F | None | 5, Died of Disease | ||||||||||
| 72 | M | Liver | 3, Died of Disease | ||||||||||
| 63 | F | Cholelithiasis | None | 6, Died of Disease | |||||||||
| 73 | F | Duodenum | 1, Died of Disease | ||||||||||
| 63 | F | LN | 11, Died of Disease | ||||||||||
| 78 | F | Cholelithiasis | Duodenum | 7, Died of Disease | |||||||||
| 66 | F | Cholelithiasis | None | 6, Died of Disease | |||||||||
| 78 | F | None | 5, Died of Disease | ||||||||||
| 73 | F | Cholelithiasis | Liver, colon | 12, Died of Disease | |||||||||
| 50 | F | Liver | 6, Died of Disease | ||||||||||
| 64 | M | Liver | 6, Died of Disease | ||||||||||
| 68 | M | Cholelithiasis | None | 56, Alive | |||||||||
| 63 | M | None | 3, Died of Disease | ||||||||||
| 64 | M | Liver, colon | 3, Died of Disease | ||||||||||
| 71 | F | None | 19, Died of Disease | ||||||||||
| 76 | M | None | 3, Alive | ||||||||||
| 72 | M | Cholelithiasis | Omentum | 2, Alive | |||||||||
| 60 | M | Cholelithiasis | None | 5, Died of Disease | |||||||||
| Cholecystic adenosquamous carcinoma mimicking Mirizzi syndrome | Horio T, Ogata S, Sugiura Y, et al. | 73 | F | Cholelithiasis, Obstructive jaundice | X | Hepatoduodenal ligament | 4, Died of Disease | ||||||
| Adenosquamous carcinoma of the gallbladder with tumor thrombus in left portal trunk | Iyomasa, S., Matsuzaki, Y., Hiei, K. et al. | 73 | M | Abdominal pain, palpable epigastric mass | X | Liver, L portal trunk | 120, Alive | ||||||
| Ruptured adenosquamous cell carcinoma of the gallbladder: case report and review of literature | Rustagi T, Rai M, Menon M | 74 | F | Cholelithiasis, abdominal pain, weight loss, anorexia, fever, hepatomegaly | 11 x 10 x 10 cm | X | 3 | 1 | 0 | III | Liver | Alive | |
| A case of primary adenosquamous/squamous cell carcinoma of gallbladder directly invaded duodenum | Saito A, Noguchi Y, Doi C, Mukai K, Fukuzawa K, Yoshikawa T, Amano T, Kondo J, Ito T, Izutsu H | 67 | F | X | Liver, duodenum, pancreas, colon | 4, Died of Disease | |||||||
| Adenosquamous carcinoma of gallbladder presenting as chronic cholecystitis with cholelithiasis- a rare entity | Mohan N, Agrawal R, Kumar P | 45 | F | Cholelithiasis, abdominal pain and distention, fever, SOB, constipation | 9.5 × 5.5 × 3.5 cm | X |
| Article title . | Author(s) . | Age . | Gender . | Presentation . | Tumor Size . | Radical resection performed? . | Primary tumor resection performed? . | T . | N . | M . | Stage . | Involvement of adjacent structures . | Outcome (months, status) . |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Adenosquamous carcinoma of the gallbladder warrants resection only if curative resection is feasible | Oohashi Y, Shirai Y, Wakai T, Nagakura S, Watanabe H, Hatakeyama K. | 47 | M | Cholelithiasis in 15 patients | Mean: 7 cm Range: 2.5–14 cm | X | 4 | 2a | 0 | IVb | Liver | 154, Alive | |
| 65 | F | X | 4 | 1a | 0 | IVa | Liver, omentum | 151, Alive | |||||
| 52 | F | X | 3 | 0a | 0 | III | Liver | Alive | |||||
| 60 | F | X | 1a | 0a | 0 | I | None | 121, Alive | |||||
| 69 | F | X | 4 | 1a | 0 | IVa | Liver, colon, duodenum | 62, Alive | |||||
| 62 | M | X | 4 | 2a | 0 | IVb | Liver, colon, duodenum, pancreas | 48, Alive | |||||
| 66 | F | X | 2 | 0a | 0 | III | None | 156, Died of other causes | |||||
| 84 | F | X | 3 | 2a | 1 | IVb | Bile duct | 23, Died of Disease | |||||
| 70 | F | X | 3 | 2a | 1 | IVb | Omentum | 13, Died of Disease | |||||
| 64 | F | X | 4 | 2a | 1 | IVb | Liver, duodenum, stomach | 6, Died of other causes | |||||
| 77 | F | X | 4 | 2a | 0 | IVb | Liver | 5, Died of other causes | |||||
| 62 | F | X | 4 | 2a | 0 | IVb | Liver | 5, Died of Disease | |||||
| 70 | M | X | 3 | 0a | 0 | III | Liver | 4, Died of Disease | |||||
| 83 | F | X | 4 | 0a | 0 | IVa | Liver, colon | 4, Died of Disease | |||||
| 70 | F | X | 4 | 0a | 0 | IVa | Liver, omentum | 3, Died of Disease | |||||
| 78 | M | X | 2 | 0b | 0 | II | None | 45, Died of other causes | |||||
| 60 | F | X | 2 | 2b | 0 | IVb | None | 19, Died of Disease | |||||
| 74 | F | X | 3 | 2c | 1 | IVb | Liver | 8, Died of other causes | |||||
| 72 | F | X | 2 | 2b | 0 | IVb | None | 7, Died of other causes | |||||
| 43 | F | X | 4 | 1b | 0 | IVa | Liver, colon | 5, Died of other causes | |||||
| 62 | M | X | 4 | 2b | 1 | IVb | Liver, colon | 5, Died of other causes | |||||
| 46 | F | X | 3 | 2b | 1 | IVb | Liver | 4, Died of other causes | |||||
| 67 | F | X | 3 | 2c | 0 | IVb | Liver | 3, Died of other causes | |||||
| 78 | F | X | 2 | 2c | 0 | IVb | None | 3, Died of Disease | |||||
| 75 | F | X | 3 | 0c | 0 | III | None | 3, Died of Disease | |||||
| 56 | M | X | 4 | 2c | 0 | IVb | Liver, colon | 3, Died of Disease | |||||
| 74 | F | X | 3 | 0c | 1 | IVb | None | 2, Died of Disease | |||||
| 89 | F | X | 3 | 0c | 1 | IVb | Liver | 1, Died of Disease | |||||
| Adenosquamous/squamous cell carcinoma of the gallbladder | Chan KM, Yu MC, Lee WC, Jan YY, Chen MF | 66 | F | Cholelithiasis, abdominal pain, fever, jaundice, weight loss | X | 3 | 1 | 1 | IVb | Liver | 3.2, Died of Disease | ||
| 62 | F | X | 3 | 1 | 0 | III | Liver | 18.4, Died of Disease | |||||
| 72 | F | X | 4 | 1 | 0 | IVa | Liver, duodenum, colon, bile duct | 4.7, Died of Disease | |||||
| 54 | F | X | 4 | 1 | 0 | IVa | Liver, bile duct | 9.3, Alive | |||||
| 72 | F | X | 4 | 1 | 0 | IVa | None | 87.3, Died of Disease | |||||
| 49 | M | X | 3 | 1 | 0 | III | None | 3.7, Died of Disease | |||||
| 68 | F | X | 3 | 1 | 0 | III | Liver | 4.2, Died of Disease | |||||
| 89 | F | 4 | 1 | 0 | IVa | Liver, duodenum | 0.8, Died of surgical mortality | ||||||
| 55 | M | X | 4 | 1 | 0 | IVa | Liver, stomach | 6.4, Died of Disease | |||||
| 67 | F | X | 4 | 1 | 0 | IVa | Liver, bile duct | 1.5, Died of surgical mortality | |||||
| 75 | M | X | 3 | 0 | 0 | III | None | 14.0, Died of Disease | |||||
| 66 | F | X | 3 | 1 | 1 | IVb | Liver | 1.5, Died of Disease | |||||
| Surgical resection of splenic metastasis from the adenosquamous gallbladder carcinoma: A case report | Utsumi M, Aoki H, Kunitomo T, Mushiake Y, Kanaya N, Yasuhara I, Arata T, Katsuda K, Tanakaya K, Takeuchi H | 62 | F | Abdominal pain | 8.0 cm | X | 4 | 1 | 1 | IV | Liver, colon, spleen, diaphragm | Alive | |
| A primary adenosquamous gallbladder carcinoma with sarcomatoid features | Qian X, Wu Y, Gao B, Wang W | 51 | F | Abdominal pain, anemia, abnormal LFTs | 4.5 x 7.0 cm | X | 5, Died of Disease | ||||||
| Long-term survival of a patient with advanced adenosquamous carcinoma of the gallbladder after radical resection | Fujita T, Fukuda K, Ohmura Y, Nishi H, Mano M, Komatsubara S, Doihara H, Shimizu N | 72 | F | Fatigue, weight loss, anorexia | 4.5 cm | X | 4 | 0 | 0 | IVa | Stomach | 60, Alive | |
| Hepatopancreatoduodenectomy for squamous and adenosquamous carcinoma of the gallbladder | Miyazaki K, Tsutsumi N, Kitahara K, Mori M, Sasatomi E, Tokunaga O, Hisatsugu T | 70 | M | X | 4 | 1b | 0 | IV | Liver, duodenum | 6, Died of Disease | |||
| Adenosquamous carcinoma of the gallbladder: a clinicopathological, immunohistochemical and flow-cytometric study of 20 cases | Nishihara K, Nagai E, Izumi Y, Yamaguchi K, Tsuneyoshi M | 68 | F | Cholelithiasis | Mean: 6.3 cm Range: 3.8–10.6 cm | Radical resection performed in 10 out of 20 patients | Primary tumor resection performed in 10 out of 20 patients | Stage II: 3 Stage III: 11 Stage IV: 6 | Cystic duct, peritoneum | 3, Died of Disease | |||
| 52 | F | Cholelithiasis | None | 12, Died of Disease | |||||||||
| 64 | F | None | 5, Died of Disease | ||||||||||
| 72 | M | Liver | 3, Died of Disease | ||||||||||
| 63 | F | Cholelithiasis | None | 6, Died of Disease | |||||||||
| 73 | F | Duodenum | 1, Died of Disease | ||||||||||
| 63 | F | LN | 11, Died of Disease | ||||||||||
| 78 | F | Cholelithiasis | Duodenum | 7, Died of Disease | |||||||||
| 66 | F | Cholelithiasis | None | 6, Died of Disease | |||||||||
| 78 | F | None | 5, Died of Disease | ||||||||||
| 73 | F | Cholelithiasis | Liver, colon | 12, Died of Disease | |||||||||
| 50 | F | Liver | 6, Died of Disease | ||||||||||
| 64 | M | Liver | 6, Died of Disease | ||||||||||
| 68 | M | Cholelithiasis | None | 56, Alive | |||||||||
| 63 | M | None | 3, Died of Disease | ||||||||||
| 64 | M | Liver, colon | 3, Died of Disease | ||||||||||
| 71 | F | None | 19, Died of Disease | ||||||||||
| 76 | M | None | 3, Alive | ||||||||||
| 72 | M | Cholelithiasis | Omentum | 2, Alive | |||||||||
| 60 | M | Cholelithiasis | None | 5, Died of Disease | |||||||||
| Cholecystic adenosquamous carcinoma mimicking Mirizzi syndrome | Horio T, Ogata S, Sugiura Y, et al. | 73 | F | Cholelithiasis, Obstructive jaundice | X | Hepatoduodenal ligament | 4, Died of Disease | ||||||
| Adenosquamous carcinoma of the gallbladder with tumor thrombus in left portal trunk | Iyomasa, S., Matsuzaki, Y., Hiei, K. et al. | 73 | M | Abdominal pain, palpable epigastric mass | X | Liver, L portal trunk | 120, Alive | ||||||
| Ruptured adenosquamous cell carcinoma of the gallbladder: case report and review of literature | Rustagi T, Rai M, Menon M | 74 | F | Cholelithiasis, abdominal pain, weight loss, anorexia, fever, hepatomegaly | 11 x 10 x 10 cm | X | 3 | 1 | 0 | III | Liver | Alive | |
| A case of primary adenosquamous/squamous cell carcinoma of gallbladder directly invaded duodenum | Saito A, Noguchi Y, Doi C, Mukai K, Fukuzawa K, Yoshikawa T, Amano T, Kondo J, Ito T, Izutsu H | 67 | F | X | Liver, duodenum, pancreas, colon | 4, Died of Disease | |||||||
| Adenosquamous carcinoma of gallbladder presenting as chronic cholecystitis with cholelithiasis- a rare entity | Mohan N, Agrawal R, Kumar P | 45 | F | Cholelithiasis, abdominal pain and distention, fever, SOB, constipation | 9.5 × 5.5 × 3.5 cm | X |
| Article title . | Author(s) . | Age . | Gender . | Presentation . | Tumor Size . | Radical resection performed? . | Primary tumor resection performed? . | T . | N . | M . | Stage . | Involvement of adjacent structures . | Outcome (months, status) . |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Adenosquamous carcinoma of the gallbladder warrants resection only if curative resection is feasible | Oohashi Y, Shirai Y, Wakai T, Nagakura S, Watanabe H, Hatakeyama K. | 47 | M | Cholelithiasis in 15 patients | Mean: 7 cm Range: 2.5–14 cm | X | 4 | 2a | 0 | IVb | Liver | 154, Alive | |
| 65 | F | X | 4 | 1a | 0 | IVa | Liver, omentum | 151, Alive | |||||
| 52 | F | X | 3 | 0a | 0 | III | Liver | Alive | |||||
| 60 | F | X | 1a | 0a | 0 | I | None | 121, Alive | |||||
| 69 | F | X | 4 | 1a | 0 | IVa | Liver, colon, duodenum | 62, Alive | |||||
| 62 | M | X | 4 | 2a | 0 | IVb | Liver, colon, duodenum, pancreas | 48, Alive | |||||
| 66 | F | X | 2 | 0a | 0 | III | None | 156, Died of other causes | |||||
| 84 | F | X | 3 | 2a | 1 | IVb | Bile duct | 23, Died of Disease | |||||
| 70 | F | X | 3 | 2a | 1 | IVb | Omentum | 13, Died of Disease | |||||
| 64 | F | X | 4 | 2a | 1 | IVb | Liver, duodenum, stomach | 6, Died of other causes | |||||
| 77 | F | X | 4 | 2a | 0 | IVb | Liver | 5, Died of other causes | |||||
| 62 | F | X | 4 | 2a | 0 | IVb | Liver | 5, Died of Disease | |||||
| 70 | M | X | 3 | 0a | 0 | III | Liver | 4, Died of Disease | |||||
| 83 | F | X | 4 | 0a | 0 | IVa | Liver, colon | 4, Died of Disease | |||||
| 70 | F | X | 4 | 0a | 0 | IVa | Liver, omentum | 3, Died of Disease | |||||
| 78 | M | X | 2 | 0b | 0 | II | None | 45, Died of other causes | |||||
| 60 | F | X | 2 | 2b | 0 | IVb | None | 19, Died of Disease | |||||
| 74 | F | X | 3 | 2c | 1 | IVb | Liver | 8, Died of other causes | |||||
| 72 | F | X | 2 | 2b | 0 | IVb | None | 7, Died of other causes | |||||
| 43 | F | X | 4 | 1b | 0 | IVa | Liver, colon | 5, Died of other causes | |||||
| 62 | M | X | 4 | 2b | 1 | IVb | Liver, colon | 5, Died of other causes | |||||
| 46 | F | X | 3 | 2b | 1 | IVb | Liver | 4, Died of other causes | |||||
| 67 | F | X | 3 | 2c | 0 | IVb | Liver | 3, Died of other causes | |||||
| 78 | F | X | 2 | 2c | 0 | IVb | None | 3, Died of Disease | |||||
| 75 | F | X | 3 | 0c | 0 | III | None | 3, Died of Disease | |||||
| 56 | M | X | 4 | 2c | 0 | IVb | Liver, colon | 3, Died of Disease | |||||
| 74 | F | X | 3 | 0c | 1 | IVb | None | 2, Died of Disease | |||||
| 89 | F | X | 3 | 0c | 1 | IVb | Liver | 1, Died of Disease | |||||
| Adenosquamous/squamous cell carcinoma of the gallbladder | Chan KM, Yu MC, Lee WC, Jan YY, Chen MF | 66 | F | Cholelithiasis, abdominal pain, fever, jaundice, weight loss | X | 3 | 1 | 1 | IVb | Liver | 3.2, Died of Disease | ||
| 62 | F | X | 3 | 1 | 0 | III | Liver | 18.4, Died of Disease | |||||
| 72 | F | X | 4 | 1 | 0 | IVa | Liver, duodenum, colon, bile duct | 4.7, Died of Disease | |||||
| 54 | F | X | 4 | 1 | 0 | IVa | Liver, bile duct | 9.3, Alive | |||||
| 72 | F | X | 4 | 1 | 0 | IVa | None | 87.3, Died of Disease | |||||
| 49 | M | X | 3 | 1 | 0 | III | None | 3.7, Died of Disease | |||||
| 68 | F | X | 3 | 1 | 0 | III | Liver | 4.2, Died of Disease | |||||
| 89 | F | 4 | 1 | 0 | IVa | Liver, duodenum | 0.8, Died of surgical mortality | ||||||
| 55 | M | X | 4 | 1 | 0 | IVa | Liver, stomach | 6.4, Died of Disease | |||||
| 67 | F | X | 4 | 1 | 0 | IVa | Liver, bile duct | 1.5, Died of surgical mortality | |||||
| 75 | M | X | 3 | 0 | 0 | III | None | 14.0, Died of Disease | |||||
| 66 | F | X | 3 | 1 | 1 | IVb | Liver | 1.5, Died of Disease | |||||
| Surgical resection of splenic metastasis from the adenosquamous gallbladder carcinoma: A case report | Utsumi M, Aoki H, Kunitomo T, Mushiake Y, Kanaya N, Yasuhara I, Arata T, Katsuda K, Tanakaya K, Takeuchi H | 62 | F | Abdominal pain | 8.0 cm | X | 4 | 1 | 1 | IV | Liver, colon, spleen, diaphragm | Alive | |
| A primary adenosquamous gallbladder carcinoma with sarcomatoid features | Qian X, Wu Y, Gao B, Wang W | 51 | F | Abdominal pain, anemia, abnormal LFTs | 4.5 x 7.0 cm | X | 5, Died of Disease | ||||||
| Long-term survival of a patient with advanced adenosquamous carcinoma of the gallbladder after radical resection | Fujita T, Fukuda K, Ohmura Y, Nishi H, Mano M, Komatsubara S, Doihara H, Shimizu N | 72 | F | Fatigue, weight loss, anorexia | 4.5 cm | X | 4 | 0 | 0 | IVa | Stomach | 60, Alive | |
| Hepatopancreatoduodenectomy for squamous and adenosquamous carcinoma of the gallbladder | Miyazaki K, Tsutsumi N, Kitahara K, Mori M, Sasatomi E, Tokunaga O, Hisatsugu T | 70 | M | X | 4 | 1b | 0 | IV | Liver, duodenum | 6, Died of Disease | |||
| Adenosquamous carcinoma of the gallbladder: a clinicopathological, immunohistochemical and flow-cytometric study of 20 cases | Nishihara K, Nagai E, Izumi Y, Yamaguchi K, Tsuneyoshi M | 68 | F | Cholelithiasis | Mean: 6.3 cm Range: 3.8–10.6 cm | Radical resection performed in 10 out of 20 patients | Primary tumor resection performed in 10 out of 20 patients | Stage II: 3 Stage III: 11 Stage IV: 6 | Cystic duct, peritoneum | 3, Died of Disease | |||
| 52 | F | Cholelithiasis | None | 12, Died of Disease | |||||||||
| 64 | F | None | 5, Died of Disease | ||||||||||
| 72 | M | Liver | 3, Died of Disease | ||||||||||
| 63 | F | Cholelithiasis | None | 6, Died of Disease | |||||||||
| 73 | F | Duodenum | 1, Died of Disease | ||||||||||
| 63 | F | LN | 11, Died of Disease | ||||||||||
| 78 | F | Cholelithiasis | Duodenum | 7, Died of Disease | |||||||||
| 66 | F | Cholelithiasis | None | 6, Died of Disease | |||||||||
| 78 | F | None | 5, Died of Disease | ||||||||||
| 73 | F | Cholelithiasis | Liver, colon | 12, Died of Disease | |||||||||
| 50 | F | Liver | 6, Died of Disease | ||||||||||
| 64 | M | Liver | 6, Died of Disease | ||||||||||
| 68 | M | Cholelithiasis | None | 56, Alive | |||||||||
| 63 | M | None | 3, Died of Disease | ||||||||||
| 64 | M | Liver, colon | 3, Died of Disease | ||||||||||
| 71 | F | None | 19, Died of Disease | ||||||||||
| 76 | M | None | 3, Alive | ||||||||||
| 72 | M | Cholelithiasis | Omentum | 2, Alive | |||||||||
| 60 | M | Cholelithiasis | None | 5, Died of Disease | |||||||||
| Cholecystic adenosquamous carcinoma mimicking Mirizzi syndrome | Horio T, Ogata S, Sugiura Y, et al. | 73 | F | Cholelithiasis, Obstructive jaundice | X | Hepatoduodenal ligament | 4, Died of Disease | ||||||
| Adenosquamous carcinoma of the gallbladder with tumor thrombus in left portal trunk | Iyomasa, S., Matsuzaki, Y., Hiei, K. et al. | 73 | M | Abdominal pain, palpable epigastric mass | X | Liver, L portal trunk | 120, Alive | ||||||
| Ruptured adenosquamous cell carcinoma of the gallbladder: case report and review of literature | Rustagi T, Rai M, Menon M | 74 | F | Cholelithiasis, abdominal pain, weight loss, anorexia, fever, hepatomegaly | 11 x 10 x 10 cm | X | 3 | 1 | 0 | III | Liver | Alive | |
| A case of primary adenosquamous/squamous cell carcinoma of gallbladder directly invaded duodenum | Saito A, Noguchi Y, Doi C, Mukai K, Fukuzawa K, Yoshikawa T, Amano T, Kondo J, Ito T, Izutsu H | 67 | F | X | Liver, duodenum, pancreas, colon | 4, Died of Disease | |||||||
| Adenosquamous carcinoma of gallbladder presenting as chronic cholecystitis with cholelithiasis- a rare entity | Mohan N, Agrawal R, Kumar P | 45 | F | Cholelithiasis, abdominal pain and distention, fever, SOB, constipation | 9.5 × 5.5 × 3.5 cm | X |
Important prognostic factors of this disease are histologic grade and stage of the tumor. Because patients commonly present late, prognosis is often poor. In this population, 85% (59/69) presented at an advanced stage (defined as pT3 and greater OR Stage III and greater). The most involved adjacent structure in this population was the liver, which occurred in 53% (37/69) of patients. The overall 5-year survival rate has been estimated to be less than 5%. In this population, 60.8% (42/69) of patients died of their disease with a mean survival of 8.5 months prior to passing.
Treatment of this disease is difficult. Chemotherapy has shown little success, so surgery is often the gold standard. Two main approaches exist in the surgical treatment of gallbladder cancer: radical resection vs. resection of primary tumor alone; 52.9% (36/58) of this population underwent radical resection. It has been reported, however, that the overall survival rate is significantly better after radical resection when compared with primary resection of tumors that were incidentally found after a standard cholecystectomy.
CONCLUSION
Gallbladder carcinoma is a rare cancer with the most common subtype being adenocarcinoma. Adenosquamous carcinoma, a much less common subtype, has been shown to have more aggressive biologic behavior than adenocarcinoma. This greater proliferative capacity often leads to tumor extension to adjacent structures such as the liver rather than nodal metastasis. There is conflicting evidence in the literature regarding the prognosis of adenosquamous carcinoma compared with adenocarcinoma, although both usually have a poor outcome. With little role for chemotherapy, surgery currently appears to be the gold standard. Due to the lack of available literature on this rare disease, more studies are needed to determine a more targeted approach of treatment.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



