-
PDF
- Split View
-
Views
-
Cite
Cite
Akihiro Kohata, Wataru Shimizu, Masatoshi Kochi, Yuji Takakura, Hideki Ohdan, A case of effective Delorme’s procedure for colonic mucosal prolapse after intersphincteric resection, Journal of Surgical Case Reports, Volume 2021, Issue 9, September 2021, rjab359, https://doi.org/10.1093/jscr/rjab359
Close - Share Icon Share
Abstract
Recent surgical technical improvements, such as endoscopic surgery with intersphincteric resection (ISR), could help avoid a permanent colostomy for patients with low-lying rectal tumors. However, the problems associated with anal dysfunction following ISR remain unresolved. We performed ISR and temporary ileostomy in a patient with low-lying rectal cancer. After evaluating the stability of the anastomosis, we planned to close the ileostomy, but the patient developed post-operative colonic mucosal prolapse (CMP). Although there are treatment methods available for CMP, there is no consensus on the treatment for post-operative CMP. In this case, we performed Delorme’s procedure because the method has been reported to have advantages in terms of improving post-operative anal function. Post-operative anorectal manometry showed improvement in maximum squeeze pressure, and the patient’s anal function improved; subsequently, ileostomy closure was performed. Delorme’s procedure may be useful for patients with CMP after ISR to achieve good post-operative anal function.
INTRODUCTION
Since abdominoperineal resection (APR) was reported in the 1920s, this surgical method has been a standard treatment for low rectal cancer [1]; however, over the last two decades, surgical treatments have dramatically improved, and now, patients have options other than a permanent colostomy [2]. Recently, intersphincteric resection (ISR) is performed for very low-lying rectal cancers. This procedure requires a temporary colostomy or ileostomy because of the risk of an anastomotic leak but preserves the anus compared to a permanent stoma. However, it may decrease anal function.
Colonic mucosal prolapse (CMP) is a benign anal disease that adversely affects the anus by causing symptoms such as pain and discomfort, bleeding during defecation and worsened anal function.
There are various surgical procedures for CMP. Delorme’s procedure is a minimally invasive procedure that maintains anal function.
Here, we report a case of Delorme’s procedure for CMP that developed after ISR. The post-operative anal function was preserved to some extent.
CASE REPORT
The patient was a 61-year-old man who presented to the clinic with a chief complaint of positive fecal occult blood. Total colonoscopy revealed an erythematous, elevated 25-mm Type 0–Is tumor in the lower rectum, and the tumor was detected as a hypoechoic mass on endoscopic ultrasound. Computed tomography showed no distant metastases or lymph nodes around the tumor. Endoscopic submucosal dissection was performed. Pathology revealed that the tumor depth was pT1b (submucosa, 5000 μm, Ly0, V0, BD2), and additional surgical resection was required; thus, robot-assisted total-ISR with temporary ileostomy was performed. The patient recovered and did not have any post-operative complications and was discharged on post-operative Day 11.
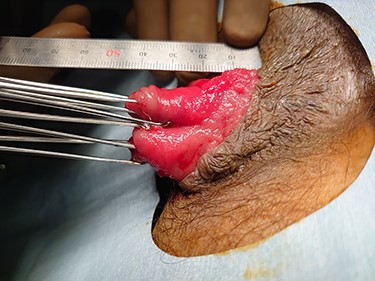
When the patient visited the outpatient clinic after discharge, he was diagnosed with CMP due to prolapse of the bowel anastomosis from the anus (Fig. 1).
It was determined that the patient had anal dysfunction, thus, surgery for CMP was performed prior to the ileostomy closure.
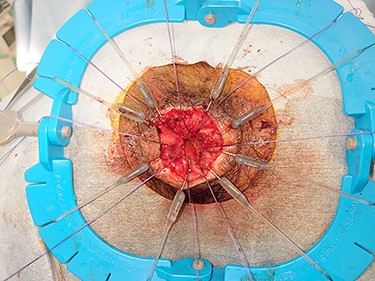
Considering its less invasive nature, we selected Delorme’s procedure (Fig. 2). The patient’s post-operative course was good, and he was discharged 4 days after surgery.
Anal function was assessed prior to surgery and post-operatively. Although the maximum resting pressure (MRP) remained low (13.2–18.0 mmHg), the maximum squeeze pressure (MSP) score changed from 214 mmHg preoperatively to 350 mmHg post-operatively. Subsequent anorectal function was good, and ileostomy closure surgery was performed.
DISCUSSION
ISR is a surgical procedure for sphincter-saving rectal surgeries in patients with very low rectal cancer and is an alternative to APR to avoid permanent colostomy. ISR has produced acceptable oncological results for early-stage cancer with similar recurrence and survival rates to APR [3]. Although ISR preserves the anus, there may be deterioration of quality of life due to fecal incontinence caused by anal dysfunction [2].
ISR is classified into three types according to the height of the circular incision in the anal canal: circular incision of the anal canal is started at the dentate line in partial-ISR, between the dentate line and intersphincteric groove in subtotal ISR and at the intersphincteric groove in total ISR [4].
As total ISR involves complete internal anal sphincter (IAS) removal, anal dysfunction is a serious potential complication as the MRP is mainly affected by the IAS [4].
There are several subtypes of rectal prolapse. Complete full-thickness rectal prolapse involves the protrusion of the full thickness of the rectal wall through the anus. The pathogenesis of rectal prolapse remains controversial. Full-thickness prolapse can be recognized as a sliding hernia through a pelvic fascial defect, or an internal rectal intussusception that progresses to a full-thickness prolapse with straining. CMP is often recognized in prolapsing colostomies or prolapsing hemorrhoids at the rectum, or an anastomotic complication occurring in 5–10% of patients, following total ISR [5]. It may be attributed to stretching and weakness of the connective tissue in the colonic mucosa [6]. Additionally, CMP after ISR may be associated with reduced anal sphincter function due to resection of the IAS.
There are two approaches to surgical treatment for rectal prolapse: transabdominal and perineal. Although the abdominal approach is thought to have significantly lower recurrence rates, randomized trials have not found evidence supporting superiority of the abdominal—over the perineal approach [6].
There are studies in which the median reduction of the improvement using the Wexner continence score following perineal resection, including Delorme’s procedure, exceeded that following laparoscopic ventral mesh rectopexy or posterior sutured rectopexy [6]. These functional improvements are thought to be due to the recovery of anal sphincter tone after removal of the prolapsed rectum, which was stretching and attenuating its muscle fibers [6]. In addition, Delorme’s procedure may result in an internal sphincter-like function by adding sutures to the intestinal muscle layer after mucosal resection [5]. This may have improved the Wexner score even in post-ISR cases.
There are treatments for rectal prolapse, but there is no certainty about the treatment of CMP after ISR. Narihiro et al. reported that among 720 cases of ISR, 33 (4.5%) were diagnosed with post-operative mucosal prolapse in the anastomosis after the long-term follow-ups. Furthermore, they stated that once prolapse occurred around the anus, patients complained of severe local symptoms, requiring surgical interventions, which undermined their quality of life [5]. Delorme’s procedure was performed for all patients with post-operative CMP, and symptoms improved in all of them. No patients complained of anal discomfort due to incontinence or prolapse, except for pain in four patients [5].
Post-operative Delorme’s surgery for CMP increases the MRP and MSP and decreases the minimum expression of feces and the maximum tolerated dose. The addition of sutures to the muscle layer brings about a sphincter-like function and may be responsible for the increase in MRP or MSP.
Although there is literature suggesting good anal function with Delorme’s surgery after ISR, there are no reports describing anorectal manometry. In our case, we confirmed the MSP improvement, and this led us to perform ileostomy closure.
This case suggests that Delorme’s surgery is a potential treatment option for CMP after low rectal surgery like ISR.
ACKNOWLEDGEMENTS
We would like to thank Editage (www.editage.jp) for English language editing.
CONFLICT OF INTEREST STATEMENT
None declared.



